Sexual Function and Continence in A Urinary Diversion-Undiversion Case
Introduction
Radical cystectomy (RC) currently represents the gold standard of treatment for non-metastatic muscle invasive bladder cancer (BC) [1]. Over the last decades the complexity of urinary derivations has changed dramatically, from a simple technique aimed to divert urine to complex surgical intervention allowing a normal voiding pattern through the native urethra [2]. BC patients undergoing RC should be offered with different types of urinary diversions (UD), according to oncologic prognosis of disease, technical feasibility, patients’ age and comorbidities. Younger patients with a non-trigonal or urethral urothelial cancer, a good life expectancy, with a preserved renal and liver function should be offered with orthotopic neobladder (ON) [3]. ON ileal reconfiguration is a highly challenging and time-consuming procedure, with a high rate of early and long-term complications [4,5]. On the other hand, Ileal Conduit (IC) represents the most worldwide diffusion type of UD, with shorter operative time, fewer post-operative complications and lower incidence of metabolic disorders [2,6].
Regardless the type of UD, RC represent a sort of “mutilation” for the patient and it could affect psychological behavior with strong impact in quality of life, especially in case of incontinent diversion [3]. Therefore, the Health Related- Quality of Life (HR-QoL) is an important concept, recently developed to define patients’ health taking into account emotional, psychological, physical aspects and their social interactions. Multiple validated questionnaires have been used to assess HR-QoL in patients who underwent RC, with different items according to the type of UD [7]. We aim to present the case of a young BC men that previously underwent RC with ON, converted to IC due to early surgical complications, who demanded a further ON conversion because of a perceived altered self-body image and poor QoL.
Case Presentation
A 46-year-old man with IC diversion referred to our department in 2008 with the diagnosis of a 3 cm lower pole right renal stone, with recurrent back pain and hydronephrosis. The patient had no co-morbidity besides essential hypertension and obesity (BMI 34). Concerning urological history, in 1998, at the age of 35 years old, the patient underwent RC (pathologic examination: transitional cell carcinoma, pT4 N0 R0 Mx and Grade 3) with ON reconstruction at a different tertiary care urologic institute: a 55-cm distal ileal segment was isolated and reconfigured into a “U” fold to reproduce the standard Studer technique [8]. On the 12th postoperative day the patient was submitted to a further surgical procedure to convert the ON into IC urinary diversion due to an entero-urinary fistula. Intraoperative exploration of the abdomen revealed the presence of two surgical dehiscences of the reservoir with no evidence of any damage at the level of neo-bladder neck. The surgeon detached the ON from the urethral stump and tried to connect the reservoir to the abdominal wall to perform an IC.
Due to the fixity and the insufficient length of the ON, the surgeon needed to isolate and add a further 7cm ileal tract to the ON, to perform the IC. The next hospital stay proceeded with no further complications. The patient subsequently underwent 2 cycles of adjuvant chemotherapy. In 2008, the patient performed a computed tomography (CT), which detected a 25mm stone at the lower pole of the right kidney and no evidence of disease’s recurrence was identified. The patient referred to our center for the renal stone’s treatment and in May he underwent percutaneous nephrolithotripsy for treatment of renal stone increased to 3cm, with complete resolution. During following diagnostic evaluations, the patient reported a fully preserved sexual potency without assumption of PDE-5 inhibitor or intracavernous injection of prostaglandin but he reported a low number of sexual intercourses, due to his altered body image. The patient expressed a deep dissatisfaction about the impaired quality of life related to the presence of a cutaneous stoma. Considering his young age, strong motivation, a preserved renal function, good performance status and no evidence of recurrence of disease, the patient was proposed a further IC into an ON surgical conversion.
Figure 1: Note:
a) CT scan with evidence of novel orthotopic neobladderand
b) regular renal excretory phase with bilateral grade 1 hydronephrosis.
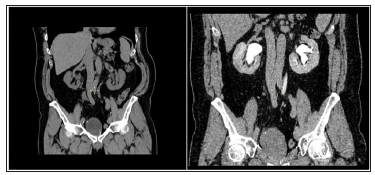
Pre-operative urethroscopy revealed the persistence of urethral lumen up to the urinary sphincter, which appeared still preserved and contractile (Figure 1). The abdominal contrast enhanced CT revealed no ureteral obstruction, with the evidence of a 40cm ileal reservoir and no significant hydronephrosis. In May 2009, the patient underwent a further surgical intervention consist of mobilization of the ileal conduit and the reconfiguration of the residual ileal tract in a novel J pouch, leaving intact both the uretero-ileal anastomosis. Then, the distal tract of the J pouch was connected to the urethral stump using non-absorbable suture with separated stitches. No intra- or post-operative complications were recorded. The naso-gastric tube was removed on postoperative day 3 and defecation was signaled on postoperative day 7. The patient was discharged on postoperative day 10. Bladder catheter was removed on 15th post-operative day following a retrograde cystography, which was negative for urinary leakages at the level of pouch-urethral anastomosis.
Results
The patient reported full day-time continence from about 2 weeks after the removal of the bladder catheter, using a single daily pad for self-assurance. Furthermore, the patient reported complete and fully satisfactory sexual intercourses, without any additional PDE-5 inhibitor or prostaglandin penile injections. No difficulties in maintaining the erection to completion sexual intercoursewas reported. Specific domains were analysed using International Index of Erectile Function 5 (IIEF-5), with the result of 24.8 years after the latter conversion, during latest clinical examination the patient was administered with 36-Item Short Form Health Survey SF-36 which revealed good-to-optimal results in each domain (Table 1).
Discussion
Choice of UD after RC is based on different features including oncologic aspects, patients related co-morbidities such as age at surgery, renal and liver function, previous enteric surgery and patient preference. A proper patient selection is essential to achieve satisfactory QoL outcomes for any type of diversion. Patients with ON will need initial and sometimes long follow up, to increase time between clocked voiding and/or self-catheterization to gradually expand the bladder storage capacity, with seldom lasting nighttime incontinence [5,9]. On the other hand, patients with IC will experience a greater alteration of their self-body image, along with a long period required to comprehend an adequate stoma care. According to current literature, postoperative daytime and nocturnal continence after RC with ON ranges between 87-95% and 72-95 % respectively [10]. Moreover, postoperative erectile function (EF) is another important factor which further impairs BC male individuals following RC. RC significantly affects EF recovery, as result of removal or damage of the neurovascular bundles.
When considering nerve-sparing RC, the two main outcomes are represented by the gain of a sufficient rate of EF recovery and a nonetheless adequate local cancer control [13]. In very selected patients with non-muscle invasive BC, good pre-operative IIEF score and highly motivated to preserved sexual function, several sex-sparing techniques of RC have been proposed through the years, with potency rates between 75100% [12,13]. Several questionnaires have been proposed to measure QoL in patients who underwent RC evaluating physical, emotional, cognitive, work- and role- related and seldom spiritual aspects [7]. The SF- 36 is structured with 36 questions which considers eight aspects of HR-QoL and demographics with a 0-100 score. However, despite minimal differences in terms of QoL in general, patients with ON scored better in Role functioning and Role-emotional specific items than those with IC: the absence of a cutaneous stoma and therefore a preserved image of theirself, improved the state of mind in patients with a good life expectancy [13]. Furthermore, patients aged less than 65 with ON presented a better SF 36 score throughout the whole examination [14].
Our patient reported a fully recovered sexual potency right after the first surgical procedure, however, the presence of the cutaneous stoma impaired greatly his sexual, affective and personal sphere, with few sexual intercourses and impaired libido. Despite the lack of previous evidence of similar case described in literature, taking into account his motivations and according to his relatively young age, good performance and optimal oncological status, we chose to attempt the surgical conversion into a novel ON. No early nor late surgical complications were recorded at last follow up. Urinary continence was reached two weeks after bladder catheter removal, despite a 9 year-span of inhabited urethra. Furthermore, he reported a deep satisfaction concerning sexual activity and overall status. Despite the lack of clear evidences, a young and motivated BC patient with good life expectancy from an oncological and general standpoint could benefit from an “atypical” surgical conversion of IC into a ON, especially concerning the psychological sphere. We present an extremely singular case, with huge technical difficulties due to an altered abdominal anatomy following previous surgery. Beside oncological and medical outcomes in general, QoL has to be considered as an important endpoint when considering the most suitable type of diversion.
Study of Prevalence and Associated Risk Factors of Bovine Fasciolosis in and Around Ambo District Abattoir and Field Survey Western Ethiopia-https://biomedres01.blogspot.com/2020/05/study-of-prevalence-and-associated-risk.html



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.