Accuracy of Elastography for Differentiation Benign and Malignant Breast Lesions
Introduction
Breast cancer is one of the foremost common cancers in women and its leading cause of cancer mortality in women and constitutes 14% of female cancer passing. It is expected that 41,070 passing due to BC happened within the year 2017 [1]. The expanding worldwide rate of malignant maladies has been recorded by World Health Organization (WHO) and is an issue of genuine concern, especially in creating countries where the increment appears to be more dominant [2]. Breast cancer has gotten to be a major danger to female wellbeing in Iraq, where it is the driving cause of passing after cardiovascular diseases among women, with a cancerrelated mortality rate of 23% [3]. It has been the highest-ranked malignancy among the Iraqi populace in common since 1986. The most recent Iraqi Cancer Registry uncovered that among an evaluated populace estimate of 32,500,000, an add up to of 21,101 unused cases of cancer were enrolled in 2012. Breast is reliable of diverse tissues counting fibrous, glandular as well. Breast is reliable of diverse tissues counting fibrous, glandular as well as fatty tissues [4,5]. The soft consistency of the breast is made of fatty tissues that encompass the breast glands.
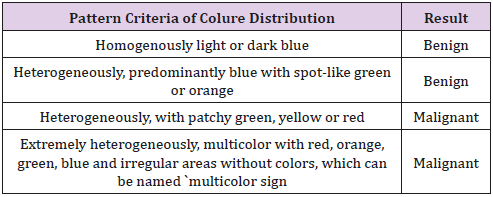
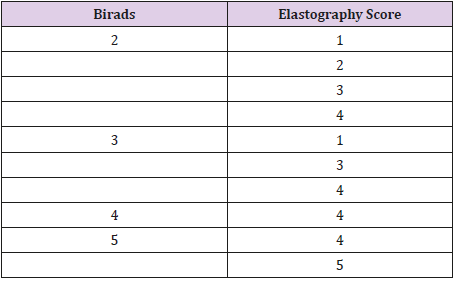
Distinctive breast lesions are shown, fibroadenoma is considered the commonest benign tumor whereas the invasive ductal carcinoma is the commonest malignant tumor [6]. Therefore, elastography has as of late been presented to move forward the exactness and specificity of diagnostic ultrasound [7]. Ultrasound elastography is utilized to evaluate tissue stiffness. The procedure depends on the hypothesis that malignant and benign breast lesions have inalienable contrasts in solidness [7]. Distinctive ultrasound elastography procedures have been risen, counting compression strain imaging, and real-time shear velocity. These days compression ultrasound elastography is considered the foremost commonly utilized strategy in breast imaging [8]. A color outline is produced and is comparing to the gray-scale ultrasound images. A grading scale utilized to classify lesions, concurring to the color signature, has been presented by Youk et al. [9] (Table 1). The point of this pondering was to assess the diagnostic utility of sonoelastography in combination with ultrasonography in arranging to distinguish breast masses (benign from malignant).
Patients and Methods
Patients: This prospective study included 80 female patients who were alluded to the radiology department at Oncology teaching clinic, medical city, Baghdad, Iraq. The study was performed between March 2018 and May 2018 for assessment of not completely diagnosed solid breast lesions.
Inclusion criteria: Any female persistent who had a single solid breast lesion that was palpable by clinical examination or obvious on ordinary ultrasound and classified utilizing the Breast Imaging Reporting and Data System (BI-RADS) as categories II –V.
Exclusion criteria:
a) Patients with BI-RADS 0 and I categories, or with numerous lesions.
b) Patients with a histopathologically affirmed malignant breast mass, or who had already experienced ipsilateral breast surgery or gotten breast radiotherapy.
c) Pregnant and breastfeeding women
d) Women how used HRT
Methods
All patients were examined using B-mode ultrasound and elastography employing a 5-17-MHz linear transducer (GE Voluson E6) amid one examination sitting, by one radiologist with encounter more than 10 years in breast imaging. Both B mode and elastography has done by the same radiologist. The study convention was endorsed by the radiology department at health and technology college and informed consent was gotten from each subject included within the study. Each participant was subjected to complete history taking, and thorough clinical examination and they did the followings:
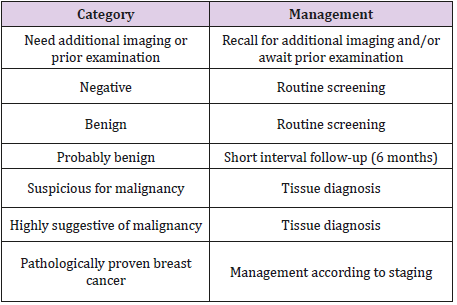
B-Mode Ultrasound: B-mode ultrasound was performed at first for all breast lesions. At that point, lesions were classified as agreeing to the BI-RADS category (Table 2) [10].
Elastography: Elastography was conducted employing a superficial transducer, which was connected opposite to the longest diameter of the breast lesion, applying light pressure to avoid distortion of high elasticity. The elastography images were gotten in “one-shot scan” mode. Contact jelly was applied (inadequate sums to decrease artifacts) and patients were inquired to hold their breath for some seconds whereas they were scanned. Colour mode information, speed, proliferation, and tissue elasticity were analyzed for each lesion once, using the frozen picture. Engendering mode shows a design of lines representing the exactness and reliability of the procured shear wave information. The more parallel lines, the more exact information. The width between the lines is more prominent in stiff lesions than in solid soft tissue. This data is utilized to direct the distinguishing proof of a region of interest (ROI) on ranges with more parallel form lines [3]. Color mode employments four color patterns (depicted in Table 1). Patterns 1 and 2 are considered to represent a benign lesion, while patterns 3 and 4 are considered positive for malignant lesion [10]. The imaging results were compared with histopathological results.
Statistical Analysis
Information was examined using IBM SPSS Insights 25. Descriptive statistic was performed in a shape of number and rate for qualitative data. Chi-squared test (χ2) and independent paired t-test were utilized to consider the significance of affiliation between elstosonography of breast lesion and histopathology. A p-value of ≤ 0.05 was considered significant.
Results
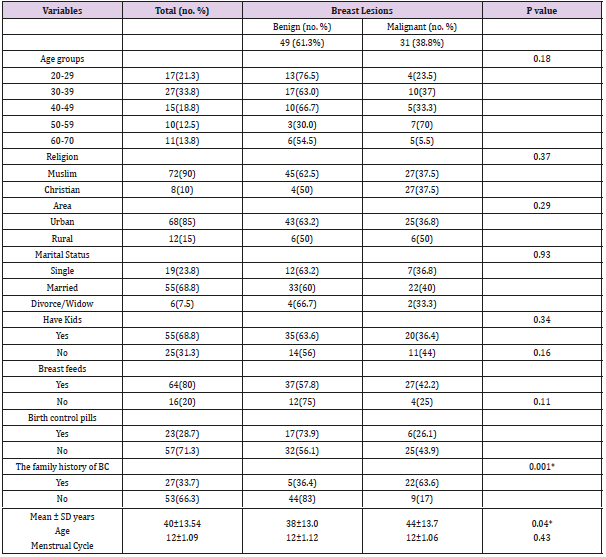
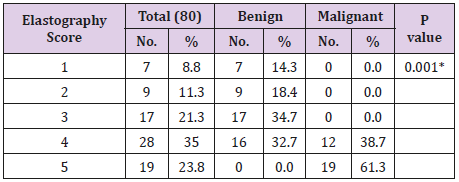
This study included 80 patients with palpable breast lumps. Their ages extended from 20 years to 70 years with a mean±SD age of 40±13.54 years and the mean±SD, to begin with, the menstrual cycle was 12±1.09 years. Table 4 appears sociodemographic variables distribution in connection to breast screening by ultrasound combined with elastography, most respondents are Muslim, Urban, married with kids on breastfeeding, most of these women did not utilize birth control pills, Most of the participant had no family history of breast cancer (66.3). All patients were assessed by grayscale ultrasound and sono-elastography examination, 80 cases had numerous diverse pathological lesions. Histopathologic examination uncovered that 49 lesions (61.3%) were benign and 31 (38.8%) were malignant (Table 3), this table appears there’s no significant association between breast lesions (benign and malignant) with sociodemographic factors but in term of family history of BC and age with p<0.05. Agreeing to the BI-RADS classification, 7 breast lesions (8.8%) were BI-RADS 2, 42 lesions (52.5%) were BI-RADS 3, 8 lesions (10%) were BI-RADS 4 and 23 lesions (28.7%) were BIRADS 5. The connection between the BIRADS of the examined lesions and the diagnosis are summarized in Table 4. This table appears significant affiliation with a p-value < 0.05. Elastography was performed in 80 cases and being classified agreeing to modified Ueno and Ito elasticity score system. Benign lesions had elastography score 1, 2, 3 and 4 as follow: 7 lesions (14.3%) had elastography score 1, 9 lesions (18.4%) had elastography score 2, 17lesions (34.7%) had elastography score 3 and 16 lesions (32.7%) had elastography score 4. However malignant breast lesions had elastography score 4 and 5 as follow: 12 injuries (38.7%) had elastography score 4, 19 injuries (61.3%) had elastography score 5 (Table 5).
This table appears noteworthy affiliation between elastography score with the diagnosis of breast lesions with a P value <0.05. None of the malignant lesions had score 1or 2, whereas none of the benign lesions had score 5.
As regards the connection between BI-RADS classification and elastography score (Table 6):
a) Lesions with BI-RADS 2 had elastography score 1, 2, 3 and 4.
b) Lesions with BI-RADS 3 had score 1, 2, 3 and 4.
c) Lesions with BI-RADS 4 had score 4.
d) Lesions with BI-RADS 5 had score 4 and 5.
e) Lesions with BI-RADS 6 had score 3. (These cases were diagnosed as breast cancer but we evaluate a de novo lesion after administration of the essential).
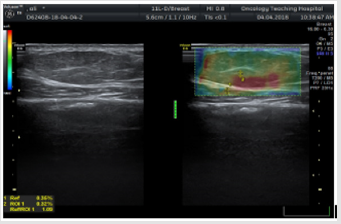
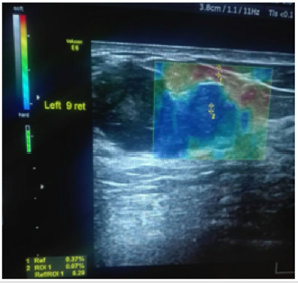
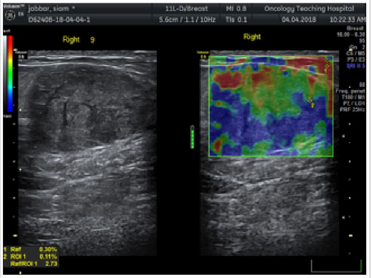
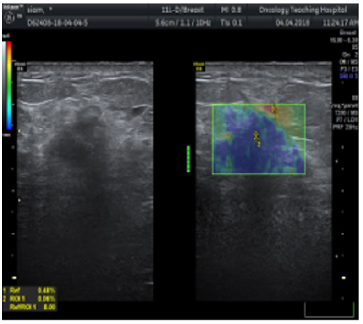
In this study: Fibroadenoma, simple cyst, and fibrocystic changes were the foremost common benign lesions whereas infiltrative ductal carcinoma was the foremost common malignant lesion. Fibroadenomas showed up smooth oval or adjusted in shape with well-defined edges, homogenous echotexture, isoechoic with bilateral acoustic shadowing, wider than taller and either softer than or had the same elasticity as adjoining glandular tissue with score 1, 2 or 3 (Figure 1). Fibroadenomas sometimes have size and stiffness pattern by elastography which is similar to that of malignant lesions as in calcified fibroadenomas with elasticity score 3 or 4 (Figure 2). Malignant breast lesions are speculated, irregularly formed, unwell outlined, with heterogeneous echotexture, distorted design, central shadowing, taller than wider, small calcifications, elastography score 4 or 5. They appeared larger on the elastography image due to higher visualization of the encircling desmoplastic reaction (Figures 3 & 4).
Figure 1: 36 year’s females with single left palpable breast lump.
a) The conventional US showed well-defined iso to the hypoechoic focal lesion
b) On elastography: the lesion showed a heterogeneous but mostly green color signature with elastography score 2. The diagnosis was confirmed by follow up after 6 months to be fibroadenomas.
Figure 2: 23 years female with a palpable left breast lump, conventional US displayed hypoechoic lesion with irregular borders, posterior acoustic shadowing, elastography of the lesion revealed score 4 (the lesion was uniformly blue color signature confined to the visible margin of the lesion). The identification was confirmed infiltrating ductal carcinoma.
Figure 3: 33 years female with a single right palpable breast lump.
a) The conventional US showed well outlined hypoechoic focal lesion with multiple calcifications
b) On elastography: the lesion showed a heterogeneous however largely green and blue colors signature with elastography score four. The diagnosing was confirmed to be fibroadenomas.
Figure 4: 33 years female with a palpable right breast lump, US and elastography, showed mass dense glandular tissue with score 5 (the lesion was blue color). The final identification was confirmed by core biopsy as ductal carcinoma in situ.
Discussion
Over the years breast ultrasound elastography has evolved as an adjunct to the traditional US, changing into a valuable tool in clinical applications and currently there’s competition with different imaging modalities like PET CT and magnetic resonance imaging [11,12]. ultrasound is the main imaging tool in young females. it’s thought of as a sensitive modality to find breast cancers [13]. B-mode US depends primarily on morphologic criteria of breast lesions. A biopsy may be a necessary method to verify the identification of malignant lesions. but increased frequency of breast biopsies for benign lesions is taken into account another downside because of price, stress and redoubled risk of infection and don’t forget it’s still an invasive technique [14]. Our findings showed that breast screening during this group of women was comparable with the findings of the Iraqi Cancer Registry/Ministry of Health (2000- 2009). The mean age was 42 years. The incidence in the age group (30-39) didn’t decline since 2003; the incidence of all female breast cancer in Iraq (all ages) has up. However, breast cancer among Iraqi women still affects younger age groups than their counterparts in developed countries. any medical specialty analysis is required to look at doable causes and prevention measures [15]. Our result showed the urban ladies had a higher incidence than rural women this finding matched the study that done in Iraq among Kurdish women [16].
In this study 49 lesions (61.3%) from 80 lesions were benign and 31 lesions (38.8%) were malignant. consistent with BI-RADS analysis of the conventional B mode US, there have been 7 (14.3%) lesions from 49 benign lesions had BI-RADS 2 and 42 (85.7%) lesions had BI-RADS 3. whereas among 31 malignant breast lesions, 8 (25.8%) lesions had BI-RADS 4 and 23 (75.2% lesions had BI-RADS 5. The chi-square statistical test was unconcealed that BI-RADS categories were considerably increased among malignant cases (P < 0.001). This was in close conformity with results according to by Ikeda et al. who reported that B-mode US supported the characters of the BI-RADS had the sensitivity of 93.9%, specificity of 88.3% and accuracy of 90.6% for all breast lesions [17]. The basic elasticity of biological tissue is altered by pathological processes. Since the important time elastography depicts useful tissue elasticity changes, its addition to B-mode US hyperbolic the performance in interpretation and final analysis of breast masses [18,19].The interpretation criteria in elastography depend upon the qualitative parameter of the elasticity score [20]. Considering the elastography score on a complete range of 80lesions being classified consistent with changed Ueno and Ito elasticity score system. Among the 49 benign lesions in our study 7 Lesions had elastography score 1, 9lesions (18.4%) had elastography score 2, 17 lesions (34.7%) had elastography score 3 and 16 lesions (32.7%) had elastography score 4.
Among 32 malignant lesions in our study 12 lesions (38.7%) had elastography score 4, 19 lesions (61.3%) had elastography score 5. consistent with our study, considering the benign lesion with elasticity scores 1–3 and malignant lesion with elasticity scores 4–5, our results were slightly totally different from the studies of Thomas et al. [21] and Navarro et al. [22]. These slight variations could also be attributed to the totally different incidence of breast cancer, different selection criteria of the patient in addition as a distinction within the variety of the studied cases and variations in the used elastography techniques. Our patients with simple breast cysts pictured the characteristic 3 layers pattern of blue–green–red colors (positive BGR sign) with blue color is being the superficial one whereas red color is that the deep one, with an es of one, even in massive dimension lesions. This pattern was explained to be an aliasing artifact [23]. Our results corroborate findings according to by previous studies of Booi RC et al. [23] US elastography will diagnose the simple breast cysts and differentiate it from complicated cysts consistent with the B mode findings additionally to elastography with high confidence so as to avoid biopsy in some case. Among benign lesions, fibroadenomas tumors represent the foremost common kind of solid breast mass.
At mammography, these lesions seem also outlined lobulated hypoechoic lesions with coarse benign popcorn calcification with the benign options because the lesion is wider than taller with its long axis parallel to the skin, but if fibroadenomas by B mode ultrasound have size options almost like malignant lesions elastography can facilitate in confirming the diagnosis of its benign nature. This is matching with a study conducted by Garra bs et al. [24] who proven that 73 of fibroadenomas may be diagnosed and differentiated type malignant lesions relying upon its size, stiffness, and brightness in ultrasound and elastography examination. Among 25 lesions of fibroadenomas, 9 lesions had elastography score 4 (false positive), this in agreement with studies as well as Giuseppetti gm et al. [25] WHO according that fibroadenomas sometimes have size and stiffness features in grayscale ultrasound and elastography that is a lot of or less almost like that of malignant lesions, nonetheless these false positive findings common to occur in fibroadenomas quite 2cm with calcification. In our study ultrasound elastography of invasive ductal carcinoma unconcealed tougher lesions than benign and normal tissues with the larger size in elastography. This was according to some studies by Kamoi K et al. [26] that confirmed that elastography diagnoses the stiffness of the invasive ductal carcinoma and accurately diagnose its actual extension.
Also, sonoelastography is beneficial in diagnosis atypical carcinomas like the terribly little or hyperechoic ones or those related to acoustic improvement [26]. Invasive ductal carcinoma could categorically well outline rounded mass on ultrasound, however, this can be uncommon. In our study, 3 lesions from 17 malignant lesions were solid with areas of necrosis that show score with high strain, this was matching with studies together with Insana MF et al. [27] that reportable, tumor necrosis could provide false negative results with low strain index because it seems like a cyst. Some breast cancer could show benign options (score 1–3) on elasticity imaging like non-differentiated DCI, inflammatory carcinoma, hypercellular, necrotic or pseudocystic malignant lesion deep little neoplastic nodules and huge cancers over 2.5 cm in diameter [27]. Our study had some limitations. one observer study, that the interobserver agreement for the elasticity measuring couldn’t be assessed, we have a tendency to assessed breast lesions with no thought of breast thickness, lesion depth or size, which can influence diagnostic performance. Therefore, a further study is required to verify the connection between the elasticity values and every variable and to spot the variables that contribute to false-negative or false-positive results. additionally, the results of B-mode ultrasound combined with elastography wasn’t obtained by a radiologist however from statistical analysis of the results of the combined technique. Therefore, we’ve got not provided specific pointers for combining the BI-RADS categories with B-mode ultrasound and elastography options.
Conclusion
Combined B-mode ultrasound with shear-wave elastography can improve the general diagnostic show for the differentiation of benign and malignant breast lesion.
More BJSTR Articles: https://biomedres01.blogspot.com/




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.