Introduction
Lung cancer is the leading cause of cancer death in both men and
wen. It is divided into three main categories that include non-small
cell lung cancer (NSCLC; 80-85%), small cell lung cancer (SCLC; 10-
15%) and lung carcinoid tumor (5%). It mainly occurs in elderly
age group (65 years or older) with an average age of 70 years at
the time of diagnosis. However, it is very rare in young population
with no identified risk factors, environmental exposures, or genetic
predisposition.
Case
A 26-year-old female with insignificant past medical history
presented to the emergency department with worsening shortness
of breath following an upper respiratory tract infection for which
she completed a course of azithromycin (Z-pack). A chest x-ray
was done which showed abnormal parenchymal opacity at the left
lower lung consistent with atelectasis and/or infiltrate, in addition
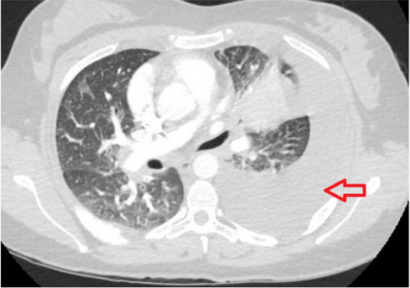
to a small left effusion. A computed tomography imaging (CT scan)
of the chest with intravenous (IV) contrast ruled out pulmonary
embolism but showed very large left-sided pleural effusion and soft
tissue density extending outward from the left hilum representing
atelectasis with the possibility of an underlying mass (Figure 1).
The patient had thoracentesis of her left lung and the pathological
analysis of the pleural fluid showed exudates with malignant cells.
Trans-abdominal ultrasound (US) to rule out Meigs syndrome
showed no acute findings, however, it did show a heterogeneous
lesion measuring up to 1.5 cm within the musculature of the
right lower abdominal wall which corresponded to the palpable
abnormality on her physical examination. US ascites survey showed
no abdominal ascites. US pelvis showed 1.5 cm intramuscular
lesion. CT of the abdomen and pelvis showed no acute process but
a subtle 1.8 cm hypodense lesion in the right hepatic lobe that is
indeterminant. Flexible bronchoscopy with bronchoalveolar lavage
and biopsies was performed.
Figure 1: A computed tomography imaging of the chest with intravenous contrast showing very large left-sided pleural effusion and soft tissue density extending outward from the left hilum with the possibility of an underlying mass.
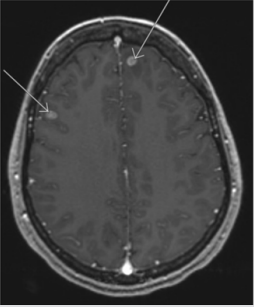
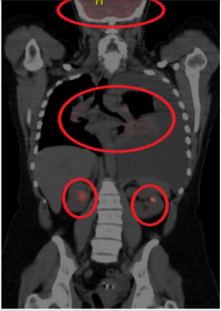
It showed evidence of stage IV adenocarcinoma with immunohistochemistry positive for anaplastic lymphoma kinase (ALK-D5F3) in the neoplastic cells. Oncology service was notified, and the patient was scheduled for outpatient chemotherapy. A follow up magnetic resonance imaging of the brain (MRI) showed multiple scattered enhancing masses situated along the gray-white interface throughout both cerebral hemispheres compatible with metastases (Figure 2). Nuclear medicine positron emission tomography (PET)/ CT scan of the skull to thigh showed multiple hypermetabolic areas suspicious for neoplastic process and metastases including the right supraclavicular lymph node, left perihilar region, right posterior lateral chest wall/rib cage, right anterior chest wall/subpectoral region, right lower anterior abdominal wall and right medial thigh. Moreover, it showed hypermetabolic liver lesion concerning for liver metastases and scattered skeletal hypermetabolic lesions suspicious for osseous metastasis including lytic sclerotic lesion in the left proximal femur (Figure 3). Taking into account her ALK positive status, the patient was planned for therapy with Alectinib and was scheduled for pleurx catheter placement by thoracic surgery to manage her pleural effusions.
Figure 2: Magnetic resonance imaging of the brain showing multiple scattered enhancing masses situated along the gray-white interface throughout both cerebral hemispheres compatible with metastases.
Figure 3: Nuclear medicine positron emission tomography of the skull to thigh showing multiple hypermetabolic areas suspicious for neoplastic process and metastases.
Discussion
Among all types of lung cancers, NSCLC is the most common
[1]; and of NSCLC subtypes, adenocarcinoma is the highest in
prevalence. Although tobacco smoking is the strongest risk factor
for lung cancers, it is less likely associated with adenocarcinoma as
compared to SCLC and squamous cell carcinoma [2]. Age has been
recognized as a risk factor for all lung cancers. In young population,
NSCL along with all other lung cancers are extremely rare with
an incidence of 0.3-0.5% [3-4]. Interestingly, among this minor
population, adenocarcinoma represents the highest portion (48%).
In this patient, who has not had any modified risk for lung cancer,
environmental exposures, or genetic predisposition, extensive
metastasis to the brain, liver, abdominal wall and bone was very
surprisingly seen at time of diagnosis. This, in fact, reflects the
aggressiveness of lung adenocarcinoma which tend to be detected
at advanced stages when diagnosed in young adults.
Conclusion
Our case report highlights the rare incidence of lung
adenocarcinoma with extensive metastases in young adults. It adds
to the literature an uncommon presentation that questions the need
for future studies and clinical trials for evaluation of metastatic
lung cancer in young age groups.
For more Articles on : https://biomedres01.blogspot.com/

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.