Home-Based Mirror Therapy with Individual Set of Exercises Improves Phantom Limb Pain and Phantom Limb Sensation of Lower Extremity Amputees
Introduction
Lower limb amputation could be the final decision to solve uncurable disorders due to trauma, infection and other general diseases [1,2]. However, the amputees might suffer lasting phantom limb phenomenon (PLPh) (including phantom limb pain (PLP) and phantom limb sensation PLS [3]) with many negative impacts on their life such as the increasing demand of pain killer, depression and impairment of daily activities and social functions [4]. The rate of PLPh is about 85% [5,6]. A study found that more than 50% of patients with PLP suffered daily pain with the significant intensity rated from moderate to severe [7]. The treatment mainly includes three main groups: pharmacology, non-pharmacology and surgery. Each approach has its own advantages and disadvantages relating to complications and cost benefit. Recently, mirror therapy is emerging and considered as a safe, economic and effective procedure in treatment of PLPh [9-11], although it was first used by Ramachandran VS in 1996 [8]. By placing a mirror parasagittally between the arms or legs and viewing the reflected movements of the intact limb while attempting simultaneous movements with the phantom limb, the intention is that the patient perceives the reflection to be their amputated limb. This phenomenon possibly addresses incongruence between proprioceptive and visual inputs caused by cortical reorganization. Currently, the method is improved with many kinds of exercises so that the patients could do at home by themselves. However, one of the key for success is to select the appropriate exercise for individual.
Objectives
Our study was designed to investigate the improvement of PLP and depression after home-based mirror therapy with personalized exercises for lower limb amputee amputation.
Methods
We conducted the study with any patient who did not reduced the PLP symptoms after a month of surgery
Criteria
Inclusion Criteria
a) Unilateral lower limb amputation
b) Phantom limb pain score (40-100 on VAS)
c) Either gender.
Exclusion Criteria
a) Amputees with psychological/neurological impairments.
b) Amputees having neuropathic pain other than phantom limb pain.
c) Patients having visual-spatial impairments.
d) Patients having residual limb pain.
e) Inability to give informed consent.
f) Infectious stump
g) Severe hearing loss
h) Any condition that restricts the movement of opposite limb, pain or limited range of motion in the intact limb
i) Infectious and systematic diseases.
Research Design
Case -Series Study
Procedures
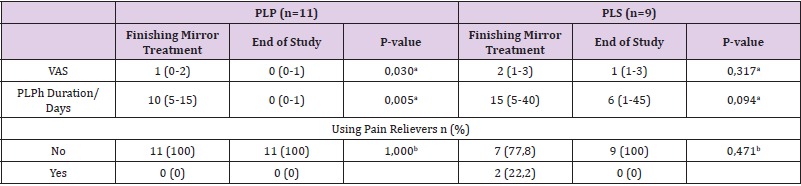
The patients were initially recorded information and assessed about pain with VAS and their use of pain killer and depression with CESD(Center for Epidemiologic Studies Depression Scale. Each patient also received an appropriate mirror and a booklet that contains guides of basic eleven exercises. In general, the exercise program was based on Netherlands guidelines [12] and the Ministry of Health’s guidelines on mirror therapy for PLPh [13] and included three groups: facilitation of visual illusion, sensory exercises, and basic motor exercises. However, each patient had individual exercises according to their preferences. The patients were asked to try every exercise, note which one made them comfortable and select at least one exercise of each group. That meant each patient had a personal set of exercise.
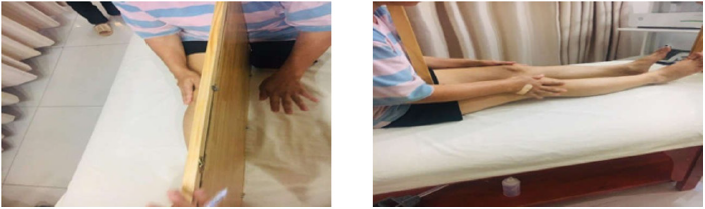
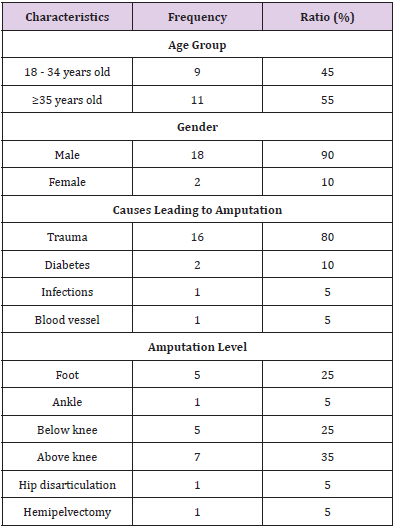
In this study, we used a 3mm thick acrylic glass with a cushion and a wooden frame to enhance its stability and prevent the injuries caused by the edge of the mirror. It had the enough length and width so that the reflection of the normal legs during exercise was complete and clear in the mirror (Figure 1). We recommended they would finish their set twice a day, at least 15 minutes per one time. The investigator would perform video call to check their adherence every two days of the first week and then once a week for 3 weeks. After finishing the one month program, the patients would be reassessed.
Data Analysis
All analytical procedures use Stata 14.2 software.
Results
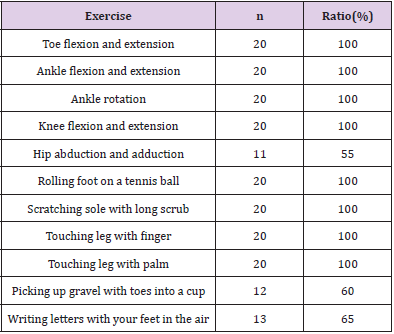
20 patients were recruited in the study from January 2020 to August 2020 at HCMC Hospital for Rehabilitation and Occupational Diseases. More than half of them were 35 years or older (55%). Male was the majority (90%). The cause of amputation mainly was trauma. The level of amputation around knee was met in 60% (Table 1A). The point of time to start the mirror therapy was about 35.5 days after amputation. The average follow-up time was 4 months. The pain characteristics were illustrated in Table 1B. The chief complain was both phantom limb pain(PLP) and phantom limb sensation (PLS). Its onset appeared rather soon from 1 to 3 days after amputation. The pain intensity was significant from moderate to severe. The sorrow lasted long with 150 minutes per day in average (Table 2). The depression condition was illustrated in Table 3. Two third of patients had signs and symptoms of depression with CESD more than 16. 19/20 patients demonstrated their adherence at the time of call. One half said they could finished all the exercises with interesting;nearly50% did not prefer Hip abduction and adduction , picking up gravel with toes into a cup and writing letters with your feet in the air (Table 2).
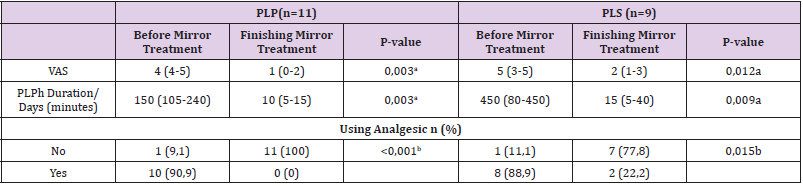
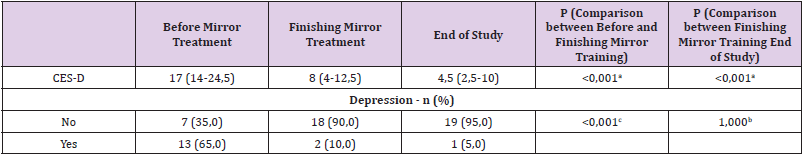
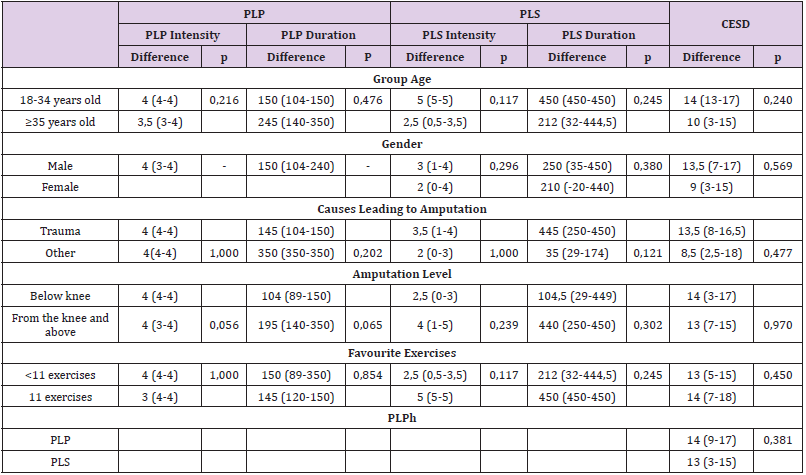
The intensity and the total daily time experiencing pain(TDTEP) of PLP significantly decreased after training mirror exercises in both groups of patients with PLP and PLS (Table 4). The extent of drug use also decreased up to ‘no use’ in patients with PLP and to a rather small extent in patients with PLS (p < 0.05 Table 4). The results was still kept maintenance or improved (Table 3) after finishing the therapy program. Depression scores also decreased after treatment and continued to decline (p <0,001 Table 5). The study results did not find a statistical significance relationship between the effect of reducing the intensity, duration of PLPh, depression score CESD with factors such as age, gender, cause of amputation, degree of amputation with p-values > 0.05 (Table 5). We did not find the relationship between pain and depression improvement with the factors such as age, gender, cause of amputation, level of amputation (Table 6).
Table 5: The results of depression after mirror treatment (n=20).
aAccredit Wilcoxon signed-rank, bAccredit Fisher, cAccredit Chi square.
Discussion
Post-amputation phantom limb pain (PLP) is highly prevalent and might be very difficult to treat. The high-prevalence, high-pain intensity levels, and decreased quality of life associated with PLP compel scientists to find out the ways to prevent, manage, and reverse this chronic pain condition. Currently, Nonoperative and non-drug PLP interventions include targeted muscle reinnervation (TMR), repetitive transcranial magnetic stimulation (rTMS), imaginal phantom limb exercises, mirror therapy (MT), virtual and augmented reality, and eye movement desensitization and reprocessing (EMDR) therapy. They are reported to be effective , however, no one is widely accepted or clearly superior to the others. Moreover, not one intervention has been found to be consistently effective [16]. Mirror therapy seems to be an suitable way for developing countries with their high rate of amputation because mirror could be available with low cost in anywhere. Mirror therapy is expected to be widely used for the treatment of phantom limb pain since it is easy to use at both home and in outpatient departments.
There are many theories to explain the mechanism of mirror therapy. Despite how the therapy has effect on central nervous system and reduce pain, one of the most important keys for success is the patient’s adherence. It is much easy to strictly follow the treatment program if the program includes simple and feasible exercises. It is also more significant if the patients experience the exercises at least one time and that makes them comfortable. That is the reason why we built a set of exercises basing on the patient’s preference. To our knowledge few study have similar treatment approach. Our encouraging results reinforce the previous studies in which mirror therapy reduced PLP in lower extremity amputees [9-11,16]. However, the “rebound phenomenon” after stopping practicing mirror exercises might be a big concern. In order to evaluate the stability of the effectiveness we still followed up our patients for about 4 months . We found that the intensity and TDTEP of PLPh continued to decrease. We also found some accompanying positive effects such as the decrease of the demand of pain killer and improvement of depression condition. The Darnall BD study also gave similar results [10].
Conclusion
Home based Four- week practice of mirror therapy with an individual set of exercises based on the patient’s result in significant reduction of PLP and PLPh and their improvement of depression condition in lower limb amputees. The interventions are simple and cost- benefit thus appropriate to the low-resource communities.
For more Articles on : https://biomedres01.blogspot.com/




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.