Rox Index as Predictor of Ventilatory Failure in Patients Admitted to ICU July 2020 to January 2021
Introduction
Coronavirus disease 2019 (COVID-19) caused by the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first emerged in China in December 2019 and caused a global pandemic [1]. Approximately 10% to 20% of patients admitted to hospital require intensive care, most of whom undergo mechanical ventilation (MV) for pneumonia complicated by severe hypoxemia [2]. The high-flow nasal cannula (HFNC) and continuous positive airway pressure (CPAP) are recognized treatments for hypoxemic respiratory failure caused by community-acquired pneumonia (CAP) [3-7]. HFNC and CPAP may represent definitive therapy that avoids unnecessary MV or provides bridging respiratory support that compensates for the need for immediate MV, preserving finite critical care resources. However, the costs of the system such as HFNC as well as CPAP and the low availability of this in health institutions in developing countries make it necessary to consider the use of other devices such as the non-rebreathing mask in patients who have hypoxemia refractory to low-flow systems. The ratio of the oxygen saturation index (ROX) is used to predict the failure of HFNC in the treatment of CAP [6,7]. There are few published data that describe the use of the ROX index to guide the use of HFNC to treat respiratory failure associated with COVID-19, and there are fewer studies where the system known as the nonrebreathing mask is used; The ROX index was developed as a simple bedside test to predict HFNC failure and the need for MV, although it is likely that patients with viral pneumonia were underrepresented in referral and validation studies [8,9].
Objectives
To evaluate the positive predictive value of the ROX index in patients admitted in the period from July 2020 to January 2021. To determine its power to determine the risk of death and the requirement of invasive mechanical ventilation.
Methodology
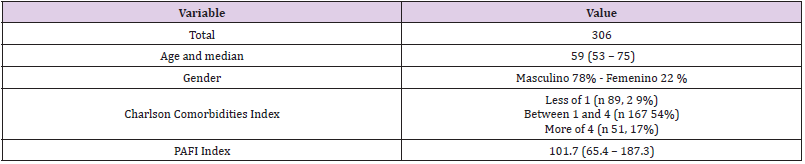
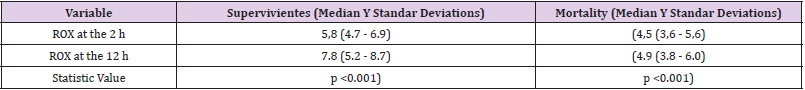
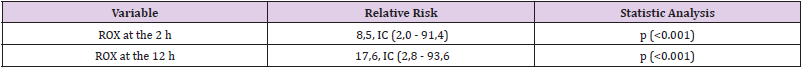
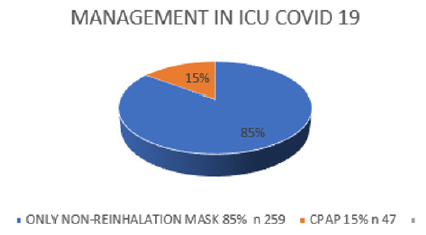
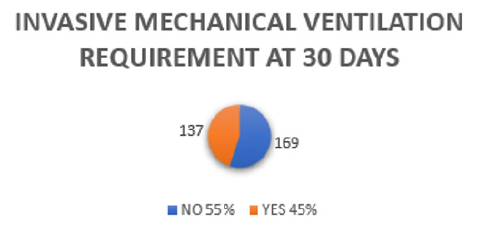
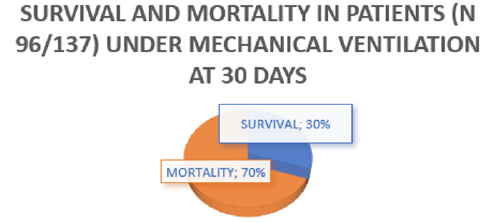
We conducted a retrospective observational study of individuals with laboratory-confirmed COVID-19 through molecular or antigenic tests, which were presented at a health institution in Piedecuesta Santander Colombia between July 2020 and January 2021. Patients who received a mask were identified. no rebreathing, CPAP or VM Tables 1-3. Medical records review captured demographic data and clinical and respiratory parameters. Of 405 hospitalized patients with laboratory confirmed COVID-19 during the study period, 306 individuals (306/405, 76%) admitted to the ICU were eligible for Non-Rebreathing Mask or CPAP as determined by treating physicians according to the national and international guidelines [10]. Of these, 259 people received only a non-rebreathing mask (85%), 47 (15%) received a combination with CPAP. The majority of people who received non-rebreathing mask or CPAP experienced severe outcomes, defined as mortality or MV at 30 days of follow-up, for mechanical ventilation (137/306, 45%) and for mortality (96/137, 70%). Table 4 in the case of patients who required ventilatory support, in agreement with the findings of multiple studies in this regard in the field of morbidity and mortality. (Figures 1-3) For those admitted, the median of the ROX indices in both deceased and survivors at 2 hours were (4.5 (3.6 - 5.6) vs 5.8 (4.7 - 6.9), p <0.001) and the 12 hours (4.9 (3.8 - 6.0) vs 7.8 (5.2 - 8.7), p = <0.001), were significantly lower in the group with severe results. ROX indices adjusted for age and sex below 4.88 at 2 (OR 8.5, CI 2.0 - 91.4) and 12 (OR 17.6, CI 2.8 - 93.6) hours after the start of the non-rebreathing mask the chances of a serious outcome increased.
Table 2: Median and standard deviations of the ROX index in deceased and survivors at 2 and 12 h after admission.
Table 3: ROX index adjusted for age and gender at 2 and 12 h after admission of the patient with its corresponding relative risk.
Figure 1: Percentages of use of non-rebreathing mask and CPAP of the patients admitted to the study.
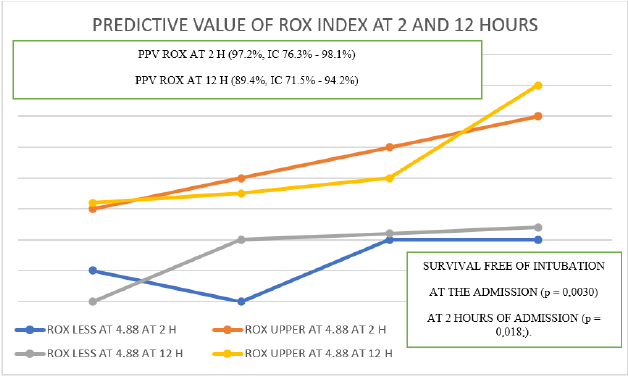
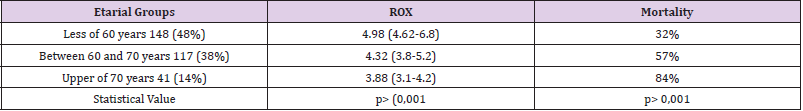
The ROX Index less than 4.88 at 2 hours after the start of the non-rebreathing mask had the highest positive predictive value for the severe outcome (97.2%, CI 76.3% - 98.1%) of the respiratory variables analyzed. For patients who received a non-rebreathing mask, intubation-free survival was significantly reduced for people with an ROX index less than 4.88 at the time of its calculation (p = 0.0030) and at 2 hours (p = 0.018). ;). For people who also received CPAP, the ROX index was a strong predictor of complications with a severe outcome, as well as mortality. The use of ROX index on the basis of suitability has been widely used even in high-resource settings [11,12]. It is essential to explore the role and results of the non-rebreathing mask and CPAP in the treatment of hypoxemic respiratory failure due to COVID-19 in patients at risk of ventilatory failure. As expected, the people with the highest mortality were older than 70 years compared to those younger than 60 years, p> 0.001), more fragile and with greater comorbidities Table 5.
Table 5: Correlation between age groups, ROX index and cumulative mortality of the patients admitted to the study.
Conclusion
The main limitation of our study is its retrospective and singlecenter nature. There were a number of variables improperly recorded in the electronic notes. Clinical observation data is lacking; however, these missing data are clearly highlighted in our summaries and do not preclude analysis. Our study consisted of a male population; a high group of these patients presented a Charlson comorbidities index of between 1 and 4 (n 167 54%) corresponding to more than half of the sample. It was appreciated that both at admission and at 12 hours the ROX index values were significantly lower in the group with severe results. Most of the people who received non-rebreathing mask or CPAP experienced morbidity and mortality outcomes and complications defined as mortality or ventilatory support at 30 days of follow-up, respectively for mechanical ventilation (137/306, 45%) about half of these patients required it and mortality (96/137, 70%) was higher than two thirds in the case of patients who required ventilatory support, in agreement with the findings of multiple studies in this regard in the field of morbidity and mortality. Our study suggests that the ROX index is a useful predictor of ventilatory failure in COVID-19 respiratory failure to identify early patients likely to require MV, as suggested in previous studies, and warrants prospective validation studies in this setting. The positive predictive value of the ROX index was greater than 85% to determine negative outcomes, especially when it was less than 4.88 both at 2 and 12 hours after admission. Likewise, the people with the highest mortality were the age group that was over 70 years of age in comparison with those under 60 years of age, p> 0.001), more fragile and with greater comorbidities.
In addition to the scarcity of existing literature where it is proposed to carry out studies in low-resource countries such as ours, expanding even more the total sample, our data suggest the use of the non-rebreathing mask guided by the ROX index in people with predictors of severity. Our study showed that an ROX index lower than 4.88 at 2 and 12 h showed a high risk of ventilatory failure associated with the requirement of mechanical ventilation, had the highest positive predictive value for the severe outcome (97.2%, CI 76.3% - 98.1 %) of the respiratory variables analyzed. Further studies are required to characterize the role of the ROX Index and risk stratification of ventilatory failure to guide resource management and decision making including the exact time to start mechanical ventilation.
For more Articles on : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.