Lymphoma Masquerading as Chondrosarcoma: The Importance of Bone Biopsy Prior to Definitive Treatment
Introduction
Enchondromas are common, benign cartilage tumors that typically present as solitary lesions of long bones [1]. They begin growth in childhood, from chondroblasts and fragments of epiphyseal cartilage that leave the growth plate and subsequently proliferate within the marrow space. They are typically asymptomatic but can occasionally cause bone pain or pathologic fracture [2]. They carry an approximately 1% lifetime risk of malignant degeneration to chondrosarcoma [3]. When this occurs, they often transform to Grade 1 chondrosarcoma or dedifferentiated chondrosarcoma, and this diagnosis is challenging to make. Atraumatic development of deep bone pain is the most common suggestive symptom [3]. Radiographic features suggesting transformation are endosteal scalloping, cortical thinning and expansion, and intralesional lysis beside/replacing the well-calcified enchondroma [4-6]. En chondromas and Grade 1 chondrosarcomas are both treated effectively with intralesional curettage and an adjuvant to decrease local recurrence.
Due to the identical treatment methodology and the sampling error that exists when performing needle biopsy of cartilage tumors, some surgeons advocate against biopsy as a means to distinguish enchondroma from Grade 1 chondrosarcoma. Instead, they rely solely on radiographic findings and symptomatology to indicate surgical intervention [7]. Degeneration to a higher grade chondrosarcoma is suggested by frank cortical destruction, soft tissue mass formation, and extensive bone edema. Intermediateand high-grade chondrosarcomas are treated with wide en bloc excision.
Considerably less common are primary and secondary bone lymphomas. Diffuse large B cell lymphoma (DLBCL) comprises 70- 80% of all bone lymphomas and often presents with painful lytic bone lesions, which can be subtle and nonspecific. Occasionally, these lesions can be misdiagnosed as benign or malignant primary bone tumors. Therefore, clinical-radiological suspicion of bone lymphoma must be confirmed with histopathology.
Making this distinction is of utmost importance, as treatment of primary and secondary bone lymphomas differs greatly from treatment of primary bone malignancies such as chondrosarcoma [8]. Chemotherapy and potential radiotherapy are the gold standard treatments for DLBCL and can be curative [9], while cartilage tumors are surgically treated [8]. We present the case of a 58-year-old woman who presented with a painful right proximal tibia bone lesion, demonstrating a lytic area surrounding a wellcalcified enchondroma. Suspicion for secondary chondrosarcoma was high. The lesion underwent biopsy which revealed aggressive DLBCL, not chondrosarcoma, drastically changing the anticipated treatment. The patient was informed that data concerning the case would be submitted for publication, and she provided consent.
Case Presentation
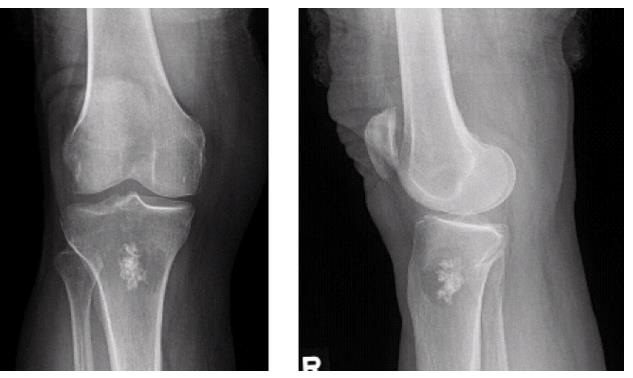
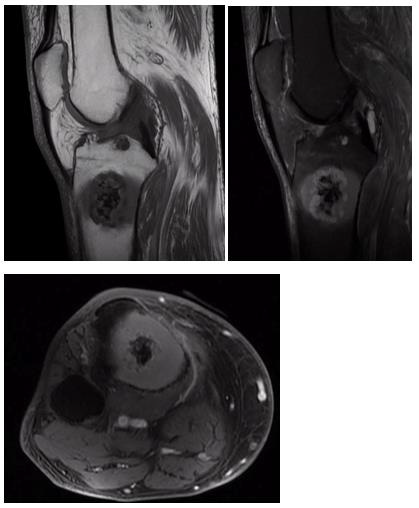
A 58-year-old woman presented for evaluation of unilateral proximal tibial pain. Plain radiographs showed an intramedullary lesion within the proximal tibial metaphysis, with stippled calcification and intralesional/perilesional lysis, concerning for malignant degeneration of benign enchondroma to chondrosarcoma (Figure 1). MRI demonstrated an area of T2 hyperintensity and post-contrast enhancement surrounding the calcified tumor, with cortical thinning, further suggesting transformation of an enchondroma to chondrosarcoma (Figure 2). An open biopsy with frozen section of the right proximal tibia was performed, with the plan being to perform intralesional curettage with adjuvant treatment if low grade cartilage tumor was found. If higher grade malignancy was detected on frozen section, the plan would be to abort further excision at that time and defer to permanent section which would dictate further oncologic treatment. Frozen section indeed demonstrated a high-grade malignancy with sheets of blue cells that was not consistent with cartilage neoplasm. Additional tissue was sent for biopsy and flow cytometry, hemostasis was achieved, and the wound was closed at that time.
Figure 1: AP and lateral plain radiographs of right knee, demonstrating bone lesion in proximal tibia with calcifications in center, surrounded by lucency.
Figure 2: T1 sagittal MRI (a, left panel), T2 fat saturated sagittal MRI (b, right panel), and T1 fat saturated postcontrast axial MRI (c, bottom panel) demonstrating cartilaginous tumor surrounded by enhancing bone lesion and associated cortical thinning.
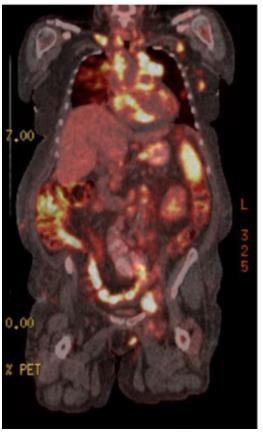
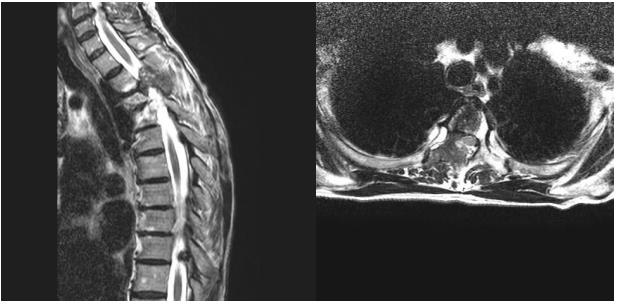
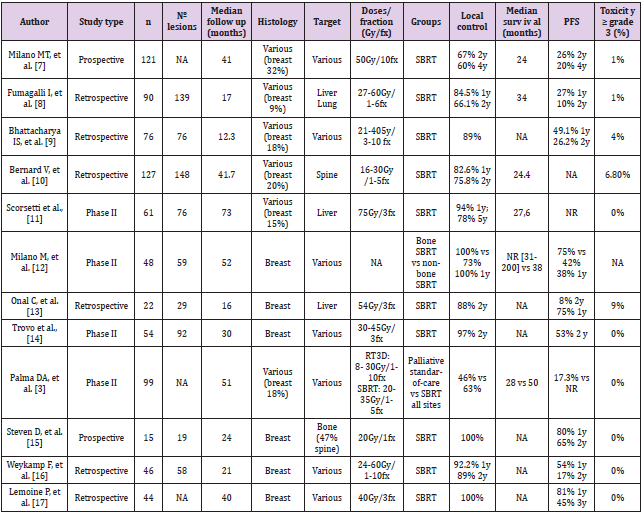
Permanent pathology indicated aggressive large B-cell lymphoma with germinal center derived phenotype, characterized by BCL6 gene rearrangement. A bland appearing hyaline cartilaginous lesion consistent with enchondroma was also noted among the biopsied tissue. A PET scan was obtained to evaluate the extent of her systemic involvement, which revealed extensive involvement of multiple lymph nodes in the axillary, supraclavicular, pelvic, and iliac regions, consistent with diffuse involvement of lymphoma (Figure 3). Six cycles of R-CHOP with radiation were planned. Her care was subsequently transferred to another medical center due to insurance issues and she was initiated on this program at the new facility. Shortly thereafter, the patient presented to the outside medical center for a bone marrow biopsy and port placement but was admitted due to hypoxia and hypercalcemia. She was diagnosed with pneumonia and cardiac tamponade and therefore underwent a cardiac window. After this, she completed her initial cycle of R-CHOP. During her hospital stay, she developed metabolic abnormalities, tumor lysis syndrome with subsequent acute kidney injury, as well as neutropenia status post chemotherapy. Soon after, she developed Pseudomonas urosepsis and shock, requiring intensive care. Her family was contacted, and comfort care was initiated. The patient passed away shortly thereafter.
Figure 3: Coronal PET scan image demonstrating multiple areas of intense abnormal hypermetabolism in the neck, right clavicle, mediastinum, and the nodes of the right supraclavicular, left axilla, chest wall, and pelvic/iliac basins; consistent with diffuse involvement in lymphoma.
Discussion
The differential diagnosis for an adult patient with a painful new bone lesion is broad. Plain radiographs are a quick and easy way to evaluate the patient’s condition, but this case report demonstrates the importance of tissue biopsy prior to definitive management of a bone tumor. The argument surrounding bone biopsy is not a recent development. In his study from 1982, Dr. Henry Mankin emphasizes the importance of a technically sound biopsy and highlights several pitfalls that can pose challenges to surgeons [10]. It is an inherently difficult yet invaluable procedure. Non-representative sampling can lead to errors in diagnosis, and poorly planned biopsies can lead to poor outcomes including amputation. Intramedullary tumors composed of cartilage matrix are still prone to sampling error [11].
With these considerations in mind, some surgeons today do not perform biopsies for tumors that have strong clinical and radiographic evidence to support chondrosarcoma diagnosis. Often, these cases suggest intermediate- or high-grade chondrosarcoma due to pain symptoms, an associated soft-tissue mass, endosteal scalloping, and aggressive radiological findings [12]. Therefore, these practitioners will rely heavily or exclusively on radiographic characteristics and clinical judgment, skipping biopsy and proceeding directly to wide en bloc excision. This patient’s presenting imaging studies were extremely concerning for high-grade malignant degeneration of a previously benign enchondroma of the proximal tibia; imaging showed intralesional lysis and bony destruction beside an area of calcified cartilage matrix, with marrow edema and enhancement. It is the authors’ opinion that, depending on their level of concern, many surgeons would have recommended definitive proximal tibia resection and endoprosthetic reconstruction based on these imaging findings suggestive of high-grade chondrosarcoma, and not learned of the true lymphoma diagnosis until several days postoperatively. Diagnosing this bone tumor as lymphoma was shocking and humbling to the surgeon, demonstrating that clinical suspicion can be gravely wrong and that rarities such as DLBCL arising within/ around an enchondroma do occur.
Mankin et al. supports the belief that a carefully performed and uncomplicated biopsy is essential to the operative treatment and control of disease despite potential biopsy dangers, suggesting that the benefits of biopsy far outweigh the considerable risks [10]. This case supports this argument that all suspected malignant bone lesions should be biopsied prior to definitive treatment, even those that are traditionally thought to be diagnoseable on imaging studies. If the surgeon in this case had empirically treated the patient with orthopaedic oncologic surgery based on the suspicion of highgrade chondrosarcoma, the patient would have been exposed to the considerable perioperative risks of unnecessary tibial resection and reconstruction, as well as a delay in systemic treatment for lymphoma. While chemotherapy in this patient unfortunately did not prolong life due to her comorbidities, the extent of her disease, and toxicity, the importance of biopsy cannot be understated.