Defined as secondary toxic fungal metabolites, mycotoxins are the greatest feed safety concerns in tropical regions [1]. They are also the most potent natural carcinogens linked to severe illnesses and an increase in the risk of liver cancer in humans as well as performance decline in commercial poultry [2]. Nonetheless, several agricultural products used for poultry feed formulation are highly susceptible to mycotoxin contamination under humid conditions. As a result, these toxins are more prevalent in tropical areas where humid environmental conditions favor fungal growth and mycotoxin production [2]. For that reason, many countries and multilateral agencies have established regulations to protect humans and poultry from consuming such contaminated products [3]. On the contrary, many underdeveloped countries like Uganda have no regulations on poultry feed safety, leaving farmers with the burden of battling the mycotoxin-associated production constraints.
Among the numerous mycotoxins, aflatoxins (AF) are the most predominant toxins hence largely contributing to the pool of toxins in the poultry feeds [4,5]. These toxins are produced by Aspergillus flavus and Aspergillus parasiticus which are common contaminants in cereal grains, oilseeds, nuts, and animal-based feed formulation ingredients [6,5]. Since these are the key feed formulation ingredients, the risks of aflatoxin toxicity are high in intensive poultry production systems. However, defined as clinical defects associated with aflatoxin ingestion, aflatoxicosis is associated with increased susceptibility to microbial stress, reduction in immune function, feed utilization, egg-laying percentage, and organ health in poultry [6,7]. Since most of the poultry feeds in Uganda are heavily contaminated with aflatoxins [8], a grave threat to commercial poultry production resulting from reduced vaccine efficacy, organ health, and feed conversion efficiency is inevitable [6,9].
On the other hand, there is no practically effective means of decontaminating feeds by destroying aflatoxins without compromising their nutritional quality [9]. This implies that the utilization of chemically inert aflatoxin sequestering agents like bentonite clays and activated carbon needs to be prioritized. However, the choice of any binder is greatly dependent on its availability and the economic feasibility of its utilization. Among the substances investigated as potential aflatoxin-binding agents, bentonites clays and activated charcoal have proved to be the most promising [10]. However, the cost-effectiveness of activated charcoal has been so variable [11], while different bentonite clays have yielded consistently promising results [6]. Recognized for forming stable complexes with aflatoxins, bentonites clays have strong affinities for aflatoxin sequestration in the gastrointestinal tract (GIT) [12]. Such sequestration is achieved through bentonite clay hydration in which the polar water molecules weaken the interaction between the closely packed bentonite layers for aflatoxin molecule intercalation [13,14]. Consequently, the resultant complex can be eliminated in the fecal materials hence preventing aflatoxin absorption into the bloodstream [15-17]. Therefore, among the several aflatoxin decontaminations approaches, bentonite clay utilization is envisaged to offer the most reliable responses.
The Aflatoxicosis Feed Problem
Most of the poultry feeds in Uganda are highly contaminated with aflatoxins (65-1000 ppb) far beyond the acceptable limits of 20 ppb [18]. Due to the dependence on such feeds, commercial poultry in Uganda is highly susceptible to aflatoxicosis, which is reflected in the reduced growth and health performance [9,19]. As a result, severe losses due to poor poultry productive performance and health defects are common due to the consumption of aflatoxin-contaminated feeds [20,21]. On the other hand, commercial aflatoxin decontaminants are not readily accessible which culminates in both technological and logistical challenges. Nonetheless, Phillips et al. and Hesham et al. studied the utilization of dissimilar bentonites in broilers and recommended contradictory inclusion levels of 0.5% and 1.0%, respectively [22,23]. In addition, bentonites are very specific in toxin adsorption, yet they also exhibit great diversities in nature [24,25]. This implies that, any attempts to improve poultry performance through bentonite clay-based aflatoxin-decontamination yield inconsistent results for different bentonite clay deposits. Such inconsistencies are attributed to the highly variable location-specific physiochemical properties among the bentonite’s clays hence the need for location-specific optimum inclusion level determination [25].
Furthermore, comparable studies on other bentonites clays have been conducted, while none has been done particularly on the Albertine bentonite clays. Besides, these studies also do not highlight responses of broiler and layer chickens with respect to aflatoxin carry-over, relative organ health, blood antibody titers alongside egg production indices. In addition, no studies have compared the performance of commercially available aflatoxin binders with the Albertine bentonite clays. Therefore, due to the inconsistent and insufficient information regarding the optimum bentonite clay inclusion levels in poultry feeds coupled with a dearth of information on the Albertine bentonites clays as aflatoxin binders [9], a study to assess the effect of adding these clays and commercial binders as aflatoxin decontaminants was necessary.
The Decontamination Potential of Bentonite Clays
The consumption of aflatoxin-contaminated feeds poses vast aflatoxicosis-related production deficits as well as contamination of poultry products [26]. The resultant aflatoxicosis, which is associated with compromised feed conversion efficiency, reduced vaccine efficacy, and histological organ deterioration, becomes a key production challenge [7,6]. Such challenges not only increase the cost of production but also the risk of losing birds due to highly infectious diseases like Newcastle and infectious bursal disease, which are known to cause up to 100% chicken mortality [26,27]. For that reason, poultry productivity cannot be improved without embracing aflatoxin-decontamination technologies from the feeds. Whereas research has shown that aflatoxin decontamination improves commercial poultry performance [26] the spectrum of decontamination techniques is limited to chemically inert bentonite clay binders and activated carbon. However, the costs involved in the production of activated carbon are prohibitive which results in its scarcity while bentonite clays are readily available as waste in oil extraction [9]. Fortunately, Uganda is endowed with huge deposits of bentonite clays in the Albertine graben region. Elsewhere, these bentonite clays have been reported to have aflatoxin sequestration abilities but with noticeable variations due to physiochemical diversity [28,22,25]. In addition, there is also a scarcity of literature regarding the optimum inclusion levels of the different Albertine bentonite clays as well as their comparative performance with respect to the commercial binders in poultry feeds. Consequently, despite the availability of such bentonite clays, farmers still make huge aflatoxicosis-induced losses due to poor feed utilization, reduced vaccine potency, and hence high mortalities. Therefore, the use of the Albertine bentonite clays as aflatoxin- binders would be a more sustainable decontamination method of averting aflatoxicosis to offset the heavy poultry production losses and the carcinogenic consequences of consuming contaminated poultry products.
Occurrence of Mycotoxins in Foods
Defined as secondary toxic metabolites of Aspergillus species, mycotoxins can be produced on a variety of products from plant and animal origins containing more than 95% water activity [29,30]. The term mycotoxin comes from the Greek word ‘mykes’ meaning mold, and ‘toxicum’ meaning poison that causes a clinical condition referred to as mycotoxicosis [30,31]. Besides, mycotoxins are also reported to be harmful to both humans and animals when absorbed either through ingestion, inhalation, or dermal absorption [4]. However, it was later discovered that ingestion through contaminated foods is the main source of exposure to both humans and livestock [29]. This implies that; besides the direct consumption of contaminated products, humans can also get intoxicated during livestock feed preparation [4]. Recognized for their toxicity, mycotoxins have been reported to be more serious in tropical humid regions where climatic conditions favor the growth of Aspergillus species [32,18]. Such humid conditions, poor postharvest handling, and poor storage facilities make poultry feeds highly susceptible to fungal contamination [32]. Consequently, most poultry feeds in Uganda are found to be highly contaminated with aflatoxins ranging between 65 and 1000 ppb [18]. However, such contamination levels are far beyond the limit of 20 ppb beyond which feeds become unsafe for consumption [33]. Among the many mycotoxins discovered, aflatoxins are the most toxic and highly carcinogenic metabolites of Aspergillus species [4]. Moreover, these toxins which also naturally occur in combination are identified as class one human hepatocellular carcinogens [34]. In addition, aflatoxins B1 can also be metabolized in animal tissues to aflatoxin M1 from bio-activation pathways and excreted in milk [35] hence propagating the effects to infants and higher in the food chain.
Occurrence of Aflatoxins in Livestock Feeds
Aflatoxins were first isolated and characterized from Aspergillus species in poorly stored grains [36]. They were later identified to be associated with the killing of young turkeys in England and ducklings in Kenya as well as Uganda [36,29]. Therefore, these outbreaks gave way to a multitude of discoveries in determining the different types of aflatoxins alongside the associated clinical signs [37]. In addition, these toxins were discovered to be hepatotoxic with their susceptibility being dependent on species, age, nutritional status, and duration of exposure [38]. Currently, aflatoxins are known to be mainly produced by Aspergillus flavus, Aspergillus parasiticus, Aspergillus nomius which use livestock feeds as substrates [39]. Whereas 20 aflatoxins have been identified, only four (B1, B2, G1, and G2) have been widely studied due to their magnitudes of toxicity [40]. Among the four, aflatoxin B1 is the most common and dangerous to both humans and livestock [3]. However, aflatoxins naturally exist in combinations implying that focus has to be put on their synergistic effects rather than the individual effects [41]. Aflatoxins B1, B2, G1, and G2 are widely studied due to their high prevalence in food products and toxic effects [42,30]. Identified to be metabolites of aflatoxin B1 and B2, respectively, aflatoxins M1 and M2 occur in both milk and eggs of species fed aflatoxincontaminated diets [41] Besides the active aflatoxins, significant quantities of conjugated aflatoxins have also been reported to exist in feeds as well [43]. Such conjugated aflatoxins can cause unexpected toxicity when they are hydrolyzed to the precursor toxins in the gastrointestinal tract (GIT) [43]. Furthermore, as part of plant metabolism, some aflatoxins can be transformed into conjugated forms presenting additional forms of toxicity [44]. For instance, zearalenone-4-beta-d- glucopyranoside, zearalenone and deoxynivalenol glucosides which are precursors can be metabolized to the respective active toxins in the GIT [45,46]. Unfortunately, these precursors cannot be detected during routine analysis, yet they can hydrolyze during digestion contributing to the toxin pool in the GIT [45].
Perseverance of Aflatoxicosis
More than ten thousand million metric tons of grains are lost annually due to aflatoxin contamination [47]. In addition, more than four billion individuals in developing countries get chronically exposed to aflatoxicosis every year due to contaminated food consumption [48]. Such chronic exposure is largely attributed to heavy dependence on subsistence farming, unregulated local markets, and the lack of policy regulations on food and feed safety [49]. Consequently, the large aflatoxicosis outbreaks like those in Kenya and Togo claimed many lives [41] while survivors suffered from jaundice, leg edema, and hepatomegaly as well as malnutrition- related symptoms [50,51]. In fact, these outbreaks are traced to be originating from homegrown maize by subsistence farmers who have poor storage facilities [41] Typically, in this crisis 55% of maize products had contamination levels greater than 20 ppb, 35% had levels exceeding 100 ppb, and 7% beyond 1000 ppb [41]. Similarly, related cases were reported in India and China [52] which cases were all established after detecting the clinical signs of acute aflatoxicosis [48].
Effects of Aflatoxins on Human Health
Recognized as a risk factor for cancer [4], aflatoxicosis is characterized by adverse immunological and nutritional effects [48]. Among the aflatoxins, AFB1 and mixtures of AFG1, and AFM1 have been reported to be the major causes of chronic aflatoxicosis and human carcinogens [34]. Besides the carcinogenic effects, ingestion of foods contaminated with relatively lower aflatoxin levels over a long period has been reported to cause jaundice, liver cancer, chronic hepatitis [53], infertility, and impaired nutrient utilization in infants [54]. On the other hand, the ingestion of highly contaminated feeds results in acute hepatic failure, hemorrhages, digestion alterations, mental changes, and coma [48]. Besides direct chronic aflatoxicosis, aflatoxins have also been reported to complement hepatitis B in the causation of liver cancer [55]. Ultimately, the lack of policy regulations in developing countries of Southeast Asia and sub-Saharan Africa accounts for the high incidences of aflatoxicosis [41]. Such incidences, therefore, account for the fact that hepatocellular carcinoma is the fifth leading cause of cancer mortality in the world [56]. Therefore, this fact justifies the correlation between the high levels of aflatoxins contamination in maize with a high incidence of human hepatocellular carcinomas.
Biochemical Properties and Aflatoxin Metabolism
Given suitable conditions of 80-85% relative humidity and temperature of 28-35˚C up to 20 types of aflatoxins can be produced on a variety of feed substrates. However, among these naturally occurring toxins, aflatoxin B1, B2, G1, and G2 have been reported to be the most potent with aflatoxin B1 (AFB1) posing the highest degree of carcinogenicity [57]. Aflatoxins are characterized by high melting points of 260˚C and a thermal degradation temperature of 269˚C [58]. This implies that aflatoxins exhibit high thermostability although they can be decomposed by strong oxidizing agents. Aflatoxin metabolism plays the biggest role in determining the degree of toxicity in animal cells, especially in the liver [57]. The liver is considered the principal target organ for aflatoxins based on the first pass effect [59]. Since AFB1 is the most biochemically reactive, most research is focused on its metabolic pathways which justify its carcinogenic properties [57]. When aflatoxins are absorbed by the liver, they undergo biotransformation where AFB1 is metabolized through activation by cytochrome P450 enzymes to form the intermediate adduct AFB1-8, 9-epoxide. Characterized by its low stability, this adduct is responsible for the covalent modification of DNA, preferentially at the N7 position of guanine bases thereby affecting the complementary base pairing mechanisms [30]. Besides DNA modification, AFB1-8, 9-epoxide undergoes base-catalyzed reactions to form a more stable AFB1- 8, 9-dihydrodiol which is reported to be the most mutagenic metabolite [35]. In addition, Kellerman et al. reported that AFB1 can also be bio-activated to a highly active and labile intermediate AFB1 2, 3-epoxide, which reacts with various nucleophiles in the cell besides binding with DNA, RNA, and proteins [60]. Furthermore, according to [30]. Yunus et al. AFB1 can also be converted to hydroxylated metabolites (via monooxygenase’s) which are then metabolized to glucuronide and sulfate conjugate in the endoplasmic reticulum. Consequently, aflatoxicosis results in mutagenesis, carcinogenesis, and teratogenesis due to the alkylation of nuclear DNA by highly electrophilic adducts. In addition, chronic aflatoxicosis culminates into reduced protein synthesis, production of essential metabolic enzymes and structural proteins for growth [30] and immunosuppression hence poor poultry performance [61].
Aflatoxin Prevalence in Poultry Feeds
Aflatoxins are produced on a wide range of food commodities especially cereals and oilseeds which are the key ingredients in livestock feed formulation [62]. Identified as the third most consumed cereal worldwide [63], maize is most likely to be contaminated with aflatoxins at higher levels than any other feed ingredients [64]. Consequently, most of the maize-based poultry feeds in Uganda are highly contaminated with aflatoxins beyond recommended levels of 20 ppb [18]. The key predisposing factor to poultry feed contamination is poor post-harvest handling of maize which leads to high contamination levels by Aspergillus Flavus [65]. Such practices lead to high levels and prevalence of aflatoxin contamination in maize [66]. In addition, poultry feeds are stored at a relative humidity between 80% - 90% which is within the optimum range for fungal development [66]. Such conditions render the stored feeds more susceptible to fungal attacks within the normal feed storage time [32]. Whereas fungal contamination depends on postharvest handling, fungal development and aflatoxin production are dependent on storage time [66]. This implies that, as traders tend to hold maize back waiting for better market prices after harvest, high aflatoxin contamination is inevitable. Consequently, in an attempt to mitigate the aflatoxicosis-induced production declines, the Food and Drug Administration legislations set up an action level of 20 ppb as the maximum residue limit allowed in poultry feeds [67].
Effects of Aflatoxicosis on Poultry Performance
Effects of Aflatoxins on Chicken Physiology: Due to the heavy aflatoxin contamination of feed ingredients, commercial poultry is highly susceptible to chronic and acute aflatoxicosis [5,68,38]. Whereas acute is associated with the consumption of highly contaminated feeds [51], prolonged consumption of feeds with relatively low aflatoxin contamination levels is associated with chronic aflatoxicosis [69]. As a consequence, chronic aflatoxicosis is associated with poor feed utilization and increased susceptibility to microbial stress which is reflected in performance declines [70,47]. Furthermore, chronic aflatoxicosis has been reported to be the primary cause of teratogenicity, carcinogenicity, and mutagenicity as well as growth inhibitory effects in poultry [71]. These defects, therefore, result in biochemical, hemato [72] logical, and immunological alterations in the chronically affected poultry [73,74].
Effects of Aflatoxicosis on Feed Intake, Energy and Amino Acid Utilization: While feed intake and utilization are key determinants of poultry performance, aflatoxicosis has been reported to reduce feed acceptability, utilization, and enzyme efficiency [26,75]. In addition, aflatoxins interfere with calcium uptake and organic nutrient utilization in poultry while excess calcium impedes phytase enzyme activity due to insoluble complex formation with phytate phosphorous [76,77]. Furthermore, chronic aflatoxicosis decreases amino acid and energy utilization due to declines in cell metabolic efficiency [78]. Since the interaction between sulfur-containing amino acids and synthesis of aflatoxin B1-epoxide deter protein utilization and hence weight gain, it’s worth investing in available local options for sustainable aflatoxin decontamination for improved feed utilization [79].
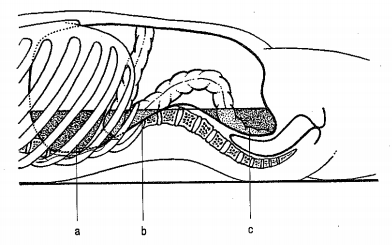
Effects of Aflatoxicosis on Humoral Immunity and Organ Health: Besides hindering nutrient utilization, aflatoxicosis results in a reduction in antibody titers of Newcastle and Infectious Bursal disease as well as regression of the bursa of Fabricius [71]. This implies that, through regression of the bursa of Fabricius, aflatoxins interact with the T-cells to affect cell-mediated immunity in poultry to suppress vaccine efficacy [71]. In addition, a reversal in chemostatic inhibition of phagocytic abilities of leucocytes as well as heterophils has been reported to be associated with aflatoxicosis. Therefore, the synergistic effect of both antibody synthesis and phagocytotic suppression contributes to the increased response to environmental stress in poultry. Relative organ weight is a key indicator of organ health, whereas chronic aflatoxicosis has been reported to increase relative liver and kidney weights it results in the regression of the Bursa of Fabricius [80] In fact, the liver and kidney are considered to be the target organs for aflatoxicosis in all the affected species. As a consequence, the accumulation of nitrogenous wastes and aflatoxin metabolites results in histopathological changes as well as inflammatory thickening of the uterine mucosa in the tissues [80]. This implies that the reduced efficiency in nitrogenous waster excretion which results from liver and kidney damage greatly accounts for aflatoxicosis-related stress in poultry.
Effect of Aflatoxicosis on Layer Production and Eggshell Characteristics: Poultry layers are bred to convert feed nutrients into egg production rather than body muscles. Aflatoxicosis has been reported to reduce egg production without noticeable variations in layer weight gains [81,82]. Aflatoxicosis in layers has been reported to cause cytoplasmic vacuolation of the hepatocytes through impaired lipid transport and synthesis [83,84]. Such impairment is accompanied by lipid deposition in the liver, and suppressed lipid levels in the blood circulation [60]. This implies that aflatoxicosis induces phospholipid and cholesterol inhibition in the liver which results in far-reaching effects on layer performance [84]. Defined as the fastest bio-ceramic calcifying process among biological systems [85], eggshell strength is a key aspect in egg storage and transportation. However, aflatoxicosis has been reported to affect eggshell characteristics by interfering with the absorption and transportation of calcium and phosphorous [86]. In addition, aflatoxins have been reported to interfere with vitamin D3 metabolism [2,87] hence affecting calcium immobilization for eggshell development. Furthermore, chronic aflatoxicosis results in hepatic damage and a reduction in hepatic zinc levels in poultry [88]. Yet, the enzyme-dependent conversion of bone calcium into egg calcium is grossly affected by the generation and composition of zinc bicarbonate in blood circulation [89]. Therefore, in addition to aflatoxin decontamination, calcium supplementation through calcium bentonite clay inclusion may not only sequester aflatoxins but also possibly improve dietary calcium availability in layers.
Aflatoxin Decontamination Approaches: Whereas preventing feed contamination offers the best option it is practically impossible to get reasonable quantities of aflatoxin-free feeds. This implies that prevention of fungal contamination during harvesting and storage [11,90], as well as fungal growth inhibition, offer more practical solutions [11]. On the contrary, most of the poultry farmers in Uganda don’t produce their feed ingredients hence the lack of such phytosanitary adherence. This, therefore, leaves feed fortification and decontamination as the most practically viable option to control aflatoxicosis. Fortification of poultry rations with synthetic methionine alleviates aflatoxicosis-induced growth depression [91]. This is attributed to the ability of sulfur-containing amino acids to inhibit AFB1 mutagenicity and AFB1- epoxide synthesis during biotransformation [79]. Nevertheless, sulfur amino acids are some of the essential and limiting amino acids in poultry diets rendering this approach less cost-effective. Therefore, aflatoxin adsorption renders one of the most effective approaches since it reduces their bioavailability in the liver [11,22].
Consequently, since there is a relatively broader spectrum of nonnutritive aflatoxin sequestering feed additives decontamination remains an economically viable option. Besides amino acid fortification, biological approaches on the other hand can be used to absorb mycotoxins through enzymatic degradation and modification [92]. As a result, these characteristics led to the creation of biofilters for fluid decontamination and probiotics which also bind and remove aflatoxins [92]. However, such biological decontamination works mainly through sorption and enzymatic degradation making it a limited approach for biological systems [93]. Besides, biological control approaches developed for decontamination of aflatoxins in feeds have equally had limited attention and a multitude of criticisms as well [94]. Similarly, chemical decontamination using acids, salts, oxidizing, and reducing agents which require drying, and cleaning have equally had setbacks [11]. These setbacks are associated with the health decline of the animals and many chemical residues in animal systems [95]. However, Huwing et al. suggested that chemicals like calcium propionate successfully inhibited mold proliferation without affecting livestock health but with significant cost implications. For that reason, toxin decontamination using inorganic and chemically inert binders like some bentonites renders the most practical and economic approach.
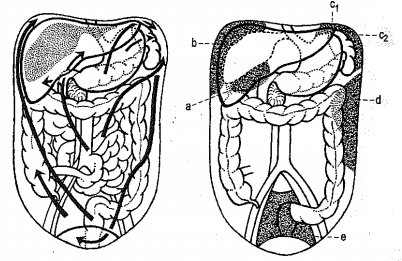
Aflatoxin Decontamination Using Binders: The most cost-effective approach to aflatoxin decontamination known is deactivation using aflatoxin binders like activated carbon and bentonite clays [95,96]. However, the chemical structure of both the aflatoxin and the binder determines the effectiveness of adsorption and binder-aflatoxin compatibility [97]. The important characteristics of the adsorbent to be taken into consideration, therefore, include its physical structure, charge, pore size, and surface area [95] in addition to the inert effect on other livestock physiological processes. Consequently, given such requirements activated carbon and hydrated sodium calcium aluminosilicates (bentonites) stand out to be the most suitable candidates for aflatoxin decontamination. Identified as a general toxin adsorptive material with a high surface to mass ratio, activated charcoal has been reported to show great potential for aflatoxin decontamination in biological systems [98]. However, the effects of activated charcoal on livestock performance have been variable [11] while responses in poultry resulted in lower economic viability than clay-based binders [1]. Such challenges consequently rule out the possibility of using activated carbon as long as bentonite clays can technically substitute them. Aflatoxin decontamination by clay binders like bentonites on the other hand is associated with hygroscopicity, polarity, and solubility which favor aflatoxin intercalation with the bentonites in water [13]. This implies that, as the bentonite clay gets hydrated in the gastrointestinal tract, the polar water molecules weaken the interaction between the closely packed bentonite layers by lowering the charge density of the sequestered exchangeable cations such as Ca2+, Mg2+, Na+ and K+ [14]. Therefore, the mechanism of aflatoxin absorption is primarily through the exchangeable cations which neutralize the interlayer charges in aluminosilicates and are involved in the binding mechanism of aflatoxin B1 [21,13] and Hydrogen bonding [99,100]. Since hydrated sodium calcium aluminosilicates have a high affinity for aflatoxin specifically, this character results in the formation of strong aflatoxin-clay complexes hence adsorption [101]. However, the properties of bentonites vary from one geological deposit to another hence the need to test the efficiency of each batch of bentonites clays as aflatoxin detoxifiers [101].
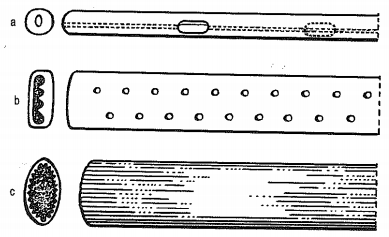
Practical Methods of Aflatoxin Decontamination: The practicability of any aflatoxin decontamination approach depends on its effectiveness and the costs associated with its application. However, the application of physical, biological, and chemical methods of decontamination separately or in combination provides varying degrees of effectiveness [102]. While physical means are less practical, with biological methods the degrading microorganisms have limited degradation mechanisms and stability in the GIT at different pH levels [103]. This consequently leaves chemically inert bentonite clays as the most suitable adsorbents for aflatoxin sequestration. Defined as a smectite clay mineral generated from the crystallization of volcanic ash, bentonite clays adopt a sheetlike structure where double layers of tetrahedral sandwich an octahedral layer to make up individual sheets. They adopt negative charges which are derived from the replacement of Al3+ with divalent Ca2+ or Mg2+ ions. Then the sheets are interconnected by the exchangeable Na+ and Ca2+ whose predominance differentiates calcium bentonite from sodium bentonite [25]. Due to its absorptive and colloidal effects, bentonite is used as a filler in pharmaceuticals and oil purification as well as additives in livestock feeds. However, their utilization in livestock feeds is limited by the fact that their physiochemical properties which are its aflatoxin sequestration signature are highly variable hence the need for localized performance evaluations.
Characterized as hydrated sodium calcium aluminosilicates, bentonites effectively bind aflatoxins in the GIT hence preventing their absorption into the bloodstream [16]. Moreover, Hesham, et al. [ 23] and Shi, et al. [33] reported an improvement in body weight gain and feed conversion ratio of broilers fed on diets fortified with bentonites. Consequently, this effectiveness of bentonites is attributed to the expanding clay lattice, interstitial water, exchangeable cations hence the aflatoxin binding ability [14]. In addition, bentonites have been also reported to be efficient against a broad spectrum of mycotoxins making them more suitable for the most frequent cases of multi-contaminated feeds [104]. Using bentonite clays hence targets binding the aflatoxins and prevents them from being absorbed from the animal’s digestive tract, and then excreting them through the fecal matter [90,13]. Characterized by the ability to form stable complexes with aflatoxins at temperatures between 25 ºC and 37 ºC, bentonites clays are capable of adsorbing aflatoxins under the condition in the GIT [105] (Magnoli et al., ). As a result, certain bentonite at 0.5% inclusion levels was able to reduce aflatoxin bioavailability in broilers [21,23]. However, bentonite clays from several sources have been reported to improve pellet stability [11] and poultry performance through aflatoxin decontamination but with varying degrees of effectiveness [105]. This implies that the different bentonite deposits in the Albertine Graben region of Uganda can provide a potential solution to feed AF decontamination [105]. However, the variation in properties among bentonites warrants assessing the performance.
The Existing Knowledge Gap: The high affinity for aflatoxins by the bentonites justifies their utilization given the high levels of aflatoxin contamination in the poultry feeds [8]. However, the aflatoxin decontamination potential among bentonite clays is highly dependent on the geographical location and nature of the bentonite clay parent materials [105]. Consequently, there is inconsistent and insufficient information about the inclusion levels of the different bentonite clay in poultry diets [9]. In addition, none of the previous studies has compared commercial aflatoxin binders with other bentonite clays as well as establishing the optimum inclusion levels of Albertine bentonite clays. Yet, beyond certain optima, bentonite clays are hypothesized to hinder nutrient utilization alongside the negative effects of excess calcium for the case of calcium bentonite. Furthermore, due to the transfer of aflatoxins and their metabolites to poultry edible products and their effect on human health, efforts have been made to set contamination limits of 20 ppb. Therefore, studies towards the exploitation of this resource are necessary since Uganda is endowed with huge bentonite deposits in the Albertine region [9].
The authors systematic review of the available aflatoxicological studies in poultry whose products are the most widely consumed among livestock products demonstrates that the majority of the studies proved a significant effect of aflatoxicosis on commercial poultry performance, carryover in products, and hence human health. The relationship between egg production and aflatoxin decontamination indicates a great reduction in the laying performance of poultry layers due to chronic aflatoxicosis. The most effective approach to combating the effects of aflatoxicosis is the use of readily available innert adsorbents like bentonites. However, it may suggest that the inclusion of such adsorbents be informed by localized feeding trials.