Choroidal Neovascularization Associated with Angioid Streaks in a Patient with Pseudoxanthoma Elasticum
Abstract
Pseudoxanthoma elasticum (PXE) is a rare, multisystemic, genetic
disorder and it is characterized by mineralization and fragmentation of
elastic fibers. PXE is associated with many complications in various
organs especially the skin, eyes, and vascular system. Angioid streaks
(AS) are the frequent ocular findings in PXE. AS with PXE is also known
as Gronblad-Strandberg syndrome. In fact, the most important
complication of PXE in ophthalmology is the development of choroidal
neovascularization. CNV is the main reason for visual impairment. In
this case report, it was aimed to share the ocular manifestations in a
patient with PXE.
Abbreviations: PXE: Pseudoxanthoma Elasticum; AS: Angioid Streaks; CNV: Choroidal Neovascularization; OCT: Optical Coherence Tomography
Introduction
Pseudoxanthoma elasticum (PXE) is a rare genetic, multisystemic
disease which affects primarily the skin, the eyes, and the vascular
system. The prevalence of PXE is approximately 1:50000-200000 [1]. PXE
is characterized by progressive calcification and degeneration in
elastic fibrils [2]. It is known that the cause of PXE is associated
with the mutation in the gene encoding the ABCC6 (MRP6) transmembrane
transport protein [3]. Ocular abnormalities or complications which are
angioid streaks (AS), peau d'orange appearance, comet lesions, and
choroidal neovascularization (CNV) develop in vast majority of patients
with PXE [4]. In PXE, the earliest fundus finding is peau d'orange
appearance and the most common ocular manifestation is as [5]. CNV occur
less than AS but CNV may lead to serious visual impairment [6]. In this
paper, we report the case of a 45-year- old PXE patient whose visual
acuity was decreased due to CNV secondary to AS.
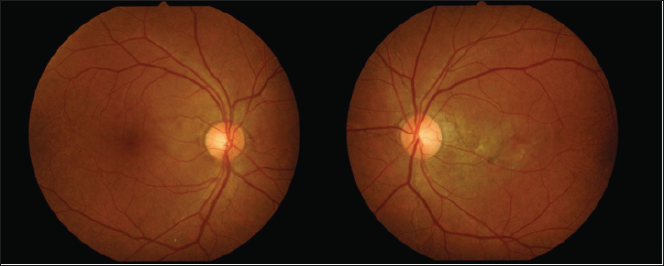
Figure 1: Fundus photography of the patient revealed peau d�orange appearance and peripapillary angioid streaks in both eyes.
Case Report
A 45-year-old man with no history of any systemic diseases presented
to our clinic complaining of visual impairment in his left eye for
approximately a year. He had previously applied to some other clinics
but could not be diagnosed correctly. Best corrected visual acuity was
20/20 OD and 16/20 OS. The anterior segment of both eyes showed no
abnormalities and intraocular pressure was 16 mmHg in both eyes. Dilated
funduscopic examination revealed peau d'orange appearance in the
temporal parts of the retina and AS extending radially from the optic
disc in both eyes (Figure 1). AS were more distinct in the left eye and
extended to near the fovea. Optical coherence tomography (OCT) revealed
CNV and intraretinal fluid in the left eye (Figure 2). Asymptomatic,
cutaneous signs such as small (1-5 millimeters), yellowish or
skin-colored papules were also observed in his back of the neck (Figure
3). When his medical history questioned again it was learned that he had
gastrointestinal bleeding before. Therefore, the patient was consulted
with the department of dermatology, internal medicine and cardiology.
Indeed, biopsy of skin lesions confirmed PXE and intravitreal anti- VEGF
injections were performed to the patient s left eye for the CNV
secondary to AS.
Figure 2: Choroidal neovascularization and intraretinal fluid observed in the left eye of the patient by optical coherence
tomography.
Discussion
Generally, the first signs of PXE are the asymptomatic cutaneous
features and AS are the most frequent ocular findings of PXE [3]. AS are
gray-white lines with rupture of the thickened elastic fibers of
Bruch's membrane extending radially from the optic disc [1]. AS occur in
80% of patients with PXE [7]. However, AS are not the pathognomonic
sign of PXE and may occur due to Paget's disease, Marfan syndrome,
Ehler-Danlos syndrom, sickle-cell anemia, and beta thalassemia [8-10].
AS most often present in both eyes and do not exist at birth. They
usually develop at third or fourth decades of life. AS mostly do not
threat visual acuity if they are not extending to the fovea. The
development of CNV near to fovea is the major cause of visual
impairment. CNV occurs in approximately 42-84% of patients with PXE [6].
The knowledge of pathogenesis and the nature of this complication
remains limited but probably, CNV may occur due to fibrovascular scar
after subretinal hemorrhages [11,12]. Besides ocular complications, some
serious and life- threatening complications associated with PXE has
been reported previously [4]. These are heart failure, sudden cardiac
death, gastrointestinal and intracerebral hemorrhages [1].
Indeed, our patient had gastrointestinal bleeding previously but no
serious problems were reported. To date, there is no effective treatment
for PXE or specific therapies for the systemic complications of this
disease. Nevertheless, intravitreal anti-VEGF injections have been
performed to increase visual acuity in PXE complicated with CNV [12]. In
conclusion, PXE is a multisystemic disorder and eye is one of the
affected organs. CNV is the most serious complication which may reduce
visual acuity but it should be kept in mind that other systemic
complications may be fatal.
Ultrastructural Pathology of Plasma and Endoplasmic Reticulum Membranes of Nerve and Glial Cells: A Review - https://biomedres01.blogspot.com/p/blog-page_5.html
More BJSTR Articles : https://biomedres01.blogspot.com




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.