Breast CA Prevention with 5th Generation Mastopexy Augmentation Technique
Abstract
In 2008 we published a premonitory article for Spanish language
readers; almost 5 years later we provide the knowledge and the follow-up
of
this amazing and gratifying technique [1]. This paper is based in the
primary authors after First World War 1914, to date: Weinzenberguer,
Thoreck,
Passot, Strombeck, Aufricht, Noel, Mckissock, Goulian, Regnault, Perras,
Hinderer, Arie, Pitanguy, Peixoto, Ribeiro, Pontes, Fellicio, Benelli,
and many
other important modern authors like Ceydelli, Graef, Gasperoni, Gulyas,
Puckett, Sampaio, Goes, Tariki, etc. Upper areolar incision has always
been
considered taboo due to fear of areola enhancement, disruption and
widening. This super areolar approach has been dismissed [2]. At this
time, we
present more than 90 evolved cases to date with successful results and
grateful standpoints for both patient and surgeon.
EBM Level II
The main objective for writing this paper is to highlight an
important difference: not only this technique provides a better shape,
avoids
numbness, and ugly scars, but it is also a preventative method against
breast cancer by partially re-sectioning upper external breast-quadrants
[3].
Keywords: Widening; Hammock; Plastma; Soft Silicon Fasteners
Introduction
There have been great improvements in the last few decades
over breast reconstruction [4] (Figures 1 & 2). As you know breast
cancer hits primarily in women around the 30 -40 range of age
(Figures 3 & 4). And at 40 % at superoexternal quadrant, 30% at
superointernal quadrant, 10 to 12% at retroareolar sites, so one of
our main proposals in this paper is to assess if being a little more
aggressive just in cases of direct inherently predisposition, such as
direct line relatives with breast cancer like mother, aunts, sisters,
etc., could be attacked, before the cancer is present in order to
avoid mutilating surgery [5-8]. That motion could be an invaluable
point of sight, from our international society to each promotion of
yearly prevention campaign for each national health institution in
the fight against breasts cancer. You will note the benefits of the
technique [9-12].
Figure 1: Normally Preoperatory Fixed Marcks Bones-Soft Tissues Relationship.
Materials and Methods
94 female patients were operated for this reason from 2004
to 2018. The ages were from 19 to 61 y.o. All of the extracted
tissue was sent to pathology in separate ways- right, left and
edges. Surprisingly 98% of pathological results showed cystic and
micro fibroadenomes, and only in one case, multiple intraductal
papilomatosis [13]. Finally, oral or IV anti-coagulation therapy
is provided if needed (Figure 5). Mastography was chosen only
when the patient had 40 y.o or more, and exceptionally in younger
women when direct relatives had been diagnosed with BREAST CA
[14]. The key point in these cases is to draw and mark the thoracic
key points with patients always standing up, but not sitting down,
and previous preparation for this kind of surgery supplying oral
ferrum and vit K 50 mgrs ingestion( if needed), 1 week before and
after surgery, and besides getting intra operatory at least 3 cc of
fresh autoplastma to apply at the end of the surgery, behind and
inferiorly of suprareolar incision, and also behind both areolar
tissues previously reduced in diameter with the technique that you
are going to see on the following explanation, in order to improve
quality and speed of wound healing [16-20]. Also of paramount
importance is the use of the “soft silicon fastener” around the areola
and incision, in order to have the whole new weight and pressure
of complex breast-implants, rest over this and not over the wounds
(Figures 6 & 7).
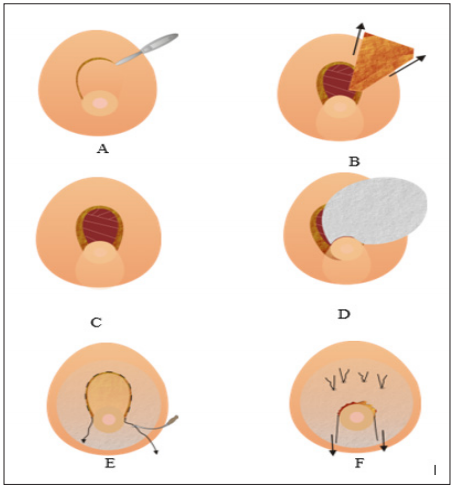
Figure 5: Stages of Surgical Access and Technique
A. Hemi moon cutting borders depitelization and. Backing down this dermical flap. To get access. To upper quadrants.
B. Dermis flap. Backing down to areola and resecting a triangle of upper external and uppermedial piece. If necessary
taking also retro areolar breast tissue.
C. A hole resulting. To remove the tissues and doing the sub facial cavity for next.
Implantation; taking care to leave bath upper lateral pilar breasts tissues to completely cover the breast over the implants.
D. Try always to put 5th generation implant (smaller, lighter, narrow west but with great projection 5 - 6)
E. Tobacco –string purse closing with Straight 2 - 0 prolene needle.
F. Backing up the dermal flap to upper position the pressure
tic-over upper wound is avoided tightening the pressure
points of soft. External silicone pieces over the dermis flap. Behind
the trough 3 - 4 ties. Than let uppers kin free of tension the
wound closure.
Technique
It should be a triangle where our complex areola- nipple is
going to be in a short future, following the vertical lines projections
over the middle clavicles points to nipples [21]. Leaving a 5 cm thick
distance from nipples to this last cut, in order to respect principal
galactophorus ducts, after that we dissect always sub-facially the
cavity for preparation to introduce an also 5th generation implant
[22-26]. In order to keep the empty breasts filled and looks
fine (Figure 8). Each extirpated breast-tissue should be sent to
pathology in different receptacles with very clear marking of the
side and position it is from [27].
Complications
At first cases were getting one partial disruption, two elongated
complex areola nipples, some infections, 2 prosthesis reported
broken after 4 years later detected trough a tomography, some
recurrence, two thick and wider upper areolar scars, some partial
or total numbness but to this date from several few years ago none
of these previously described complications have occurred [38].
Summary
The importance given to this new technique, prevents breast
cancer because we eliminate ¾ of upper breasts tissue where
normally hits 60% of breast cancer, versatility, security and with
excellent results solves at the same time a.-ptosis, b.-flatness,
prevents cancer, avoids widening recurrence, and the possibility to
execute one or two other procedures at the same time, improves
self-confidence, the breasts stay in good position and wonderful
shape in young women feeding babies is preserved because we do
not touch the principal galactophorus conducts. Besides areolar
numbness is avoided by upper incisions rejecting the lateral
nerves’ entrance to areolar zones and that is quite important for
sexuality [39-40]. It is important to take always into account that
most women would not wish big breast implants when they have
had a size c before, but it results quite important to explain that
it will result in much better shape with a small, 5th generation
implant with less volume, less weight and higher projection 5 to 6,
and it is only to avoid looking empty or flat after mastopexy [41].
In other words, we are not looking for volume or weight , we are
looking for projection with a 200 cc vol (Figures 11 & 12). any 5th
generation implants will surely look and feel like 300 cup c by the
high projection with a lower weight.
Canonical Correlation Analysis to Study
the Impacts of Different Social Factors on Awareness of Health Hazard of
Tobacco Smoking and Smoking Habit - https://biomedres01.blogspot.com/2020/02/canonical-correlation-analysis-to-study.html
More BJSTR Articles : https://biomedres01.blogspot.com




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.