Correlation between Parasitic Infections in HIV Patients Parasitic Infections in HIV Patients
Introduction
Human Immunodeficiency Virus (HIV) is a retrovirus of the Retroviridae family and the etiologic agent of Acquired Immunodeficiency Syndrome (AIDS). When first described in the United States, in 1970, this virus was observed mainly in male homosexuals, hemophiliacs and intravenous drug users [1,2]. Currently, other groups are infected with HIV, including the elderly and wives of men who have sex lives outside of marriage [3]. The genetic material of the HIV is RNA, double-stranded and enveloped. It has the ability to attach and invade mainly CD4+ lymphocytes because of CD4 receptor presence [4]. Other cells also may be invaded by HIV due to its ability to recognize other types of cellular receptors such as the CCR5 receptor present in dendritic cells, macrophages and T cells [5,6]. HIV transmission occurs through unprotected heterosexual and homosexual intercourse. Vertical transmission occurs when the virus breaks through the placental barrier during birth, or by breastfeeding [6].
Another method of transmission is the sharing of needles by drug users, the use of some cutting or perforating utensils containing HIV infected blood [7]. Patients with HIV/AIDS experience an asymptomatic phase followed by the appearance of symptoms. The symptomatic phase is characterized by severe expressions of immunodeficiency and general clinical complications. Significantly, at this point, the patient may develop some opportunistic infection [8]. Parasitic infections are responsible for significant morbidity as well as mortality worldwide [9]. In developing countries, they are considered a serious public health problem due to inadequate sanitation and lack of information, which makes the perpetuation of the life cycle of the parasites possible [10]. In these patients, parasitic infections, which are usually asymptomatic, become symptomatic and progress to serious disease, and causing death [11]. Helminths and protozoan, which affect humans and cause many symptoms, are usually associated with the gastrointestinal tract. These diseases are related to demographic, socioeconomic, physiological and immunological factors.
Thus, immunocompromised patients and/or those undergoing immunosuppressive therapy are more susceptible to contracting infections by these parasites and often with a higher degree of severity. Among the frequent intestinal parasites and related diarrhea in patients with HIV are: Entamoeba histolytica, Giardia lamblia, Ancylostomatidae, Ascaris lumbricoides, Strongyloides stercoralis and others [12,13]. People infected with HIV, enteric infections occur more frequently. Some cases are more likely to have severe recurrence and persistence. In most cases the microorganisms are not identified, although there are potential causes of diarrhea whose sources can be some form of parasitic infection [14]. Overall, these facts motivated the present research which aimed to determine the prevalence of parasitic infections in infected HIV/AIDS patients using medical records of patients who had been or were being assisted by the Joint Health Unit in Taguatinga, DF, during the period from 2005 to 2015.
Methodology
A program of transversal, quantitative and exploratory field research was carried out. The information was collected from medical records of patients with HIV/AIDS. Data were obtained from the Archival System of the Joint Health Unit of Taguatinga, DF. The data included follow-up patients and those who had been referred to be treated and monitored in other hospitals of the regional cities of Brasília, DF. The Ethics Committee of the Foundation of Teaching and Research in Health Sciences (FEPECS) approved the project (Process: 05163312.3.0000.5553 of 04/02/2013).
Target Population
Patients included those who had been diagnosed with HIV/ AIDS and who were or had been monitored and/or who were or had been in treatment at the Joint Health Unit, Taguatinga, DF, from January 2005 to July 2015. The survey was conducted at the Joint Health Unit in Taguatinga, DF, Brazil, and analyzed 502 medical records of these patients.
Criteria for Inclusion and Exclusion of Patients in the Sample
The records examined contained information regarding socioeconomic factors, gender, age, origin, profession, sexual preference, diagnostic tests performed, and medications administered, among other data. Records of patients who had not been diagnosed with HIV/AIDS, who were outside the established period or contained insufficient data to complete the questions, were excluded.
Variable Selection
Data were collected from patient charts, available in Archival System of the Joint Health Unit Taguatinga, DF. The variables chosen for the study were selected from the data included in the charts.
Biosecurity Standards
The study involved no invasive methods. For this reason, the Biosecurity Standards did not apply. The research was, however, in compliance with the recommendations of Resolution No. 196/96 of the National Health Council, maintaining the anonymity of the information that could identify patients with HIV/AIDS.
Sharing of Results
The survey results were passed on to the local group of professionals in this research area. It is very important to identify and differentiate the microorganisms that cause opportunistic infections in immunocompromised patients. For these patients the manifestation of diseases is usually more severe. Furthermore, to bring the situation under control, information and awareness are necessary. The health professionals, who deal with these issues, have the opportunity to inform patients about the necessary precautions to avoid contamination with opportunistic pathogens such as bacteria, fungi, protozoa, helminths and other pathogens.
Statistical Analysis
Data were organized in tables and graphs. The statistical analyses were conducted using Chi Square (X2 ) with the INSTAT 3 statistical program. Correlations were considered statistically significant at p <.0.5
Results
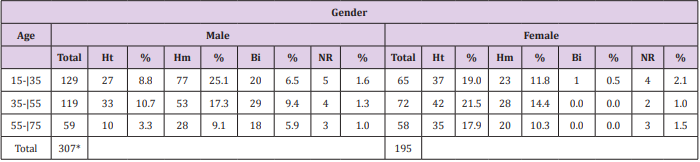
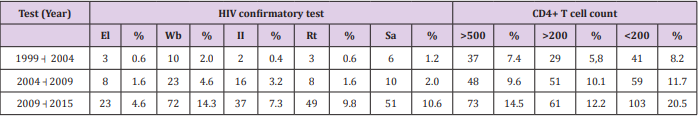
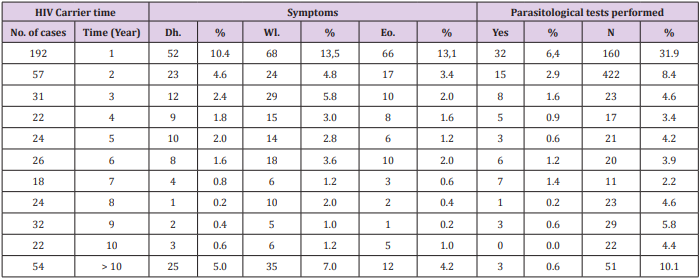
The distribution of the HIV-positive patients of the sample, by age group, gender and sexual orientation, is shown in Table 1. Most patients had been subjected to more than one test to confirm HIV. During the period from 1999 to 2004, three patients had undergone Elisa, 10 had been tested using Western blotting, two had been diagnosed using indirect immunofluorescence, three had had rapid tests and six had been examined by antibody Screening Anti-HIV 1 and 2. The distribution of HIV-positive patients, compared by the year of diagnosis and confirmatory tests performed, as well as the CD4+ cell counts, are presented in Table 2. Correlations between the diagnosis of HIV infection based on symptoms such as eosinophilia and parasitological test results of the patients of the sample, as well as the common symptoms reported that could be indicative of infection by parasites, helminths and protozoa, are shown in Table 3.
Table 1: Distribution of HIV-positive patients by age group, gender and sexual orientation, treated at the Joint Health Unit Taguatinga, Federal District, during the period 2005-2015.
Note: M: Male; F: Female; Ht: Heterosexual; Hm: Homosexual; Bi: Bisexual; NR: not reported; %: Percentage; * Significative difference.
Table 2: Distribution of HIV-positive patients at the Joint Health Unit Taguatinga-DF, by year of diagnosis, confirmatory tests and CD4+ cell count, Federal District, during the period 2005-2015.
Note: El: Elisa; Wb: Western blotting; II: Indirect Imunofluorescence; Rt: Rapid test; Sa: Screening antibodies Anti-HIV 1 and 2.
Table 3: Correlations between the diagnosis of infection with HIV, time period of clinical symptoms and parasitological examination results of patients at the Joint Health Unit Taguatinga, Federal District, during the period 2005-2015.
Note: No: Number; %: Percentage; Dh: Diarrhea; Wl; Weight loss; Eo: Eosiniphilia.
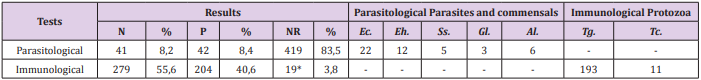
A total of 149 patients were diagnosed with diarrhea, 230 had weight loss and 140 were eosinophilia. Of the patients with diarrhea, 37 tested positive for intestinal parasites or commensals: 19 for Entamoeba coli, nine for E. histolytica, three for S. stercoralis, one for G. lamblia and five for A. lumbricoides. Of the patients who had weight loss, 11 were positive for intestinal parasites or commensals: five for E. coli, two for E. histolytica, one for S. stercoralis, and three for A. lumbricoides. In addition, of those with eosinophilia: 34 were positive for enteroparasites or commensals: 18 for E. coli, eight for E. histolytica, two for S. stercoralis, one for G. lamblia and five for A. lumbricoides. The frequency of parasites and/or commensals diagnosed in HIV-positive patients using parasitological and immunological methods is shown in Table 4. Of the total of 502 patients, 83 had undergone parasitological tests and of these 42 were positive. The most common commensal was E. coli with 22 cases. Of 483 patients who underwent immunological tests, 193 cases were positive for toxoplasmosis, and 11were positive for Chagas disease.
Table 4: Parasitological and immunological test results and species of parasites and commensals found in HIV-positive patients, the Joint Health Unit Taguatinga, Federal District, during the period 2005-2015.
Note: N: Negative; P: Positive: NR: Not performed*; %: Percentage: Ec: Entamoeba coli; Eh: Entamoeba histolytica; Ss: Strongyloides stercoralis; Gl: Giardia lamblia; Al: Ascaris lumbricoides; Tg: Toxoplasma gondii; Tc: Trypanosoma cruzi
Discussion
The age group most affected by HIV a few years ago was 20 to 40 years and men were more prevalent than women [15]. The results found in the present study corroborate these findings. The most affected patients were men (61.2%), then women (38.8%). The most infected age group was between 15-35 years of age for males. Women were most affected between 35-55 years of age. These data show that women are contracting the virus at a younger age and the number of infected women has grown over the years [16,17]. HIV/AIDS primarily affects homosexuals and drug users [1,18]. In asymptomatic homosexuals, an increase of cytotoxic T lymphocytes and suppressor T lymphocytes was observed. In terms of sexual behavior, more men aged 15-35 years were affected by HIV. Of these, 8.8% were heterosexual, 25.1% homosexual, 6.5% bisexual and 1.6% did not report sexual preference. Among women, the most prevalent age group affected by HIV was between 35-55 years, with 21.5% heterosexual, 14.4% homosexual, no cases of bisexuals and 2% did not report sexual preference. The findings confirm results reported in the literature: the male age group with the highest rates of HIV is the homosexuals and among women it is the heterosexuals [19].
The first reported cases of HIV described clinical changes related to the gastrointestinal tract. Most cases noted diarrheal conditions associated with parasitosis [19]. In a study conducted at the University Hospital of Rio de Janeiro, the parasite most often observed was A. lumbricoides [20]. In another study conducted in Rio Grande do Sul, the most common intestinal parasites were T. trichiura, G. lamblia and A. lumbricoides [21]. In the present study, intestinal parasites and commensals diagnosed in parasitological stool tests were: E. coli (most frequent, with 22 cases), E. histolytica, S. stercoralis, G. lamblia and A. lumbricoides. E. histolytica causes amoebiasis. Protozoan infections usually occur in regions where sanitary conditions are poor and typically spread by fecal-oral contamination [22]. In patients with HIV/AIDS, E. histolytica deserves special attention because it can cause fulminant amoebic dysentery [23,24].
G. lamblia is common both worldwide and in the Brazilian population [24]. It infects individuals of all ages, genders, races and social conditions [12]. The frequency of giardiasis in the present study (three cases) was low compared to other research [20,25]. This may be related to the age factor, since all individuals examined were adults and possibly the personal hygiene conditions were adequate, or because the water used by the population had been treated or filtered. It may also be related to the small number of samples analyzed. E. coli is a commensal, usually acquired by ingestion of contaminated food [26], as reported in patients with HIV [16]. The amount of E. coli found (22 cases) in the present study was relatively low, but it corroborate with the literature that show the frequency this commensals in patients HIV positive [27]. A. lumbricoides is the most common intestinal parasite in the world [28]. This disease can affect physical and mental well-being, hinder learning in children and adolescents and is even more complicated for patients with serious diseases such as HIV/AIDS [29]. The frequency of A. lumbricoides (six cases) in the present study was similar to the studies reported in the literature [21,27].
Strongyloidiasis is a parasitic disease caused by S. stercoralis and occurs in tropical and subtropical countries [12,30]. One possible means of transmission is by homosexual relationships. The biological cycle is made possible by internal and external autoinfection, by which large amounts of infective larvae are produced and can complete the autoinfection cycle and spread in the body, causing death in patients with HIV/AIDS [31]. Thus, strongyloidiasis can be considered an opportunistic infection with an AIDS-related agent [32]. The depression of cellular immunity is the conditioning factor for spread of strongyloidiasis [33,34]. Results of the present study were similar to previous studies, with low prevalence of S. stercoralis (five cases) [20,21]. Among the patients who had had immunological tests, 193 cases tested positive for reagents of T. gondii (toxoplasmosis). T. gondii is the causative agent of toxoplasmosis, it has a complex life cycle with two hosts, and several modes of transmission including blood transfusions, and transplants [35]. In Brazil, toxoplasmosis infection among those with the human immunodeficiency virus is of great importance since it is the major infectious disease found in pregnant women [36]. Toxoplasmosis is, therefore, of great medical importance as a frequent cause of death, especially in infants [37,38].
In the present study, T. gondii was the most frequent protozoan (193 cases) diagnosed by the immunological tests. Eleven patients of the study were seropositive for T. cruzi infection, or Chagas’ disease. The correlation of the disease with HIV is worrisome because the literature has shown that the reactivation of Chagas disease in immunosuppressed patients is high and associated with many cases of death [39]. Infection with T. cruzi occurs mainly through diet and blood transfusion [40]. Opportunistic infections are frequent characteristics of HIV patients and often occur due to the depletion of CD4+ T cells in number and function. But these infections can also infect and alter macrophages, Langerhans cells, dendritic cells, and CD8+ lymphocytes. It is for this reason that HIV patients are more susceptible to secondary infections [16]. In a study conducted in São Paulo, 53.6% of patients with HIV had CD4+ cell counts of less than 200/mm3 [27]. In the present study, the CD4+ cell counts of less than 200/mm were found among 8.2% of the patients studied from 1999 to 2004; from 2004 to 2009 it increased to 11.7% and from 2009 to 2015 it was 20.5 %.
Conclusion
In conclusion, it is very important to monitor the evolution of AIDS in patients in Brasília since parasitic infections caused by helminths, protozoa are frequent, and many deaths can be avoided if these pathogens are correctly diagnosed and treated. However, for such treatments to be administered in time it is necessary that serological and parasitological examinations become routine for these patients. This procedure is totally dependent on the request for the examinations by the health care professionals who provide care to these individuals.
More BJSTR Articles : https://biomedres01.blogspot.com/

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.