Dental Pulp-Derived Stem Cells: A Promising Source for Regenerative Medicine
Introduction
Regenerative medicine has the potential to replace tissues and organs damaged by age, disease or trauma. The available therapies have a limited supply of donors and can generate serious immune responses. These obstacles can be potentially solved through strategies that use stem cells (SCs) and their derivatives [1]. SCs administration may induce therapeutic responses by direct means, such as differentiation, and indirect, such as secretion of growth factors and interaction with host cells. Transplanted SCs can also stabilize the injured environment, improving tissue regeneration. Positive effects of SCs therapy have already been observed [1,2]. It is known the limitations in the clinical use of the embryonic SCs and induced pluripotentstem cells (iPSCs), so the adult SCs have been more studied bringing new perspectives for regenerative medicine. SCs are present in various tissues of the adult organism and participate in the repair of damaged tissue. They are considered multipotent, since they have a lower differentiation and proliferation capacity compared to the embryonic stem cells, but are safer and easier to obtain for use in patients [3].
Mesenchymal stromal cells (MSCs) are adult cells, multipotent and functionally defined as having self-renewal capacity, differentiation capacity in several cell lines and extensive paracrine and immunomodulatory activity [4,5]. These cells were initially described as precursors of bone marrow fibroblasts [6]. MSCs have a perivascular and avascular localization, can be isolated, expanded, cultured and characterized in vitro [7-9]. Because of their location, MSCs can be obtained from various tissues of the body [10-12] such as: bone marrow [13], placenta, amnion, umbilical cord, cord blood [12], bone tissue [14], dental tissues (tooth pulp, ligament, gingiva) [15], skin [16], adipose tissue [17], among others. It has been described the presence of different types of MSCs populations in teeth, which, depending on the site of collection, are called dental pulp stromal cells (DPSCs), periodontal ligament stromal cells (PDLSCs), apical papilla stromal cells (SCAPs), dental follicle stromal cells (DFSCs), and gingival tissue stromal cells (GMSCs), although they are generically named dental stem cells. This set of stem cells is particularly interesting because although the tooth is small it is an abundant source of stem cells for therapeutic procedures [18,19].
Dental tissues-derived SCs are important sources of SC for cell therapy, they can easily be collected and presents a low risk for the patient besides the great availability of material. The example of this is the third molar (or wisdom teeth) of young individuals, who are daily extracted for orthodontic reasons and discarded as surgical waste [20]. DPSCs were for the first time isolated and characterized from dental pulp tissue by Gronthos et al. [15] in 2000. It has been shown that the MSCs present in the tooth pulp is a small population, less than 5% of cells [15,21]. These DPSCs have perivascular localization and differentiation potential in multiple lineages like MSCs obtained from the other tissues [19].
Dental Pulp-Derived Stromal Cells: Isolation Methods
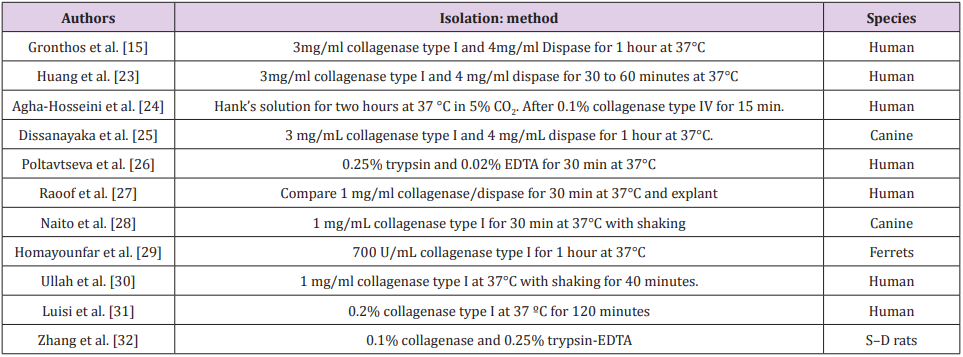
The use of MSCs on a large scale in the research depends on the quality of the cells that will promote the regeneration of an injured tissue. However, the lack of standardization of procedures makes it difficult to accurately characterize MSCs. An important aspect of standardization is the isolation method. This initial step of MSCs isolation from a specific tissue defines the population of cells that will be cultivated [22]. MSCs are generally isolated as a population of cells adhering to the plastic using simple procedures involving tissue maceration, enzymatic digestion and cell growth on a plastic surface. DPSC can be isolated using different methods such as explant and enzymatic digestion or the association of the two methods (Table 1).
Dental Pulp-Derived Stromal Cells: Characteristics
The isolated and cultivated DPSCs present fibroblast-like morphology and plastic adherence, according to the International Society for Cellular Therapy [4,15,24]. Several authors have already demonstrated that DPSCs present a positive immunophenotypic profile for CD73, CD90 and CD105, and reduced for CD14, CD19, CD34, CD45 and HLA-DR [24-33], markers suggested by ISCT. Studies have already demonstrated the presence of other positive markers in DPSCs such as CD29, CD44, CD146, CD166 and CD271 [34]. As is currently the case for MSCs, DPSCs does not seem to express a marker that exclusively identifies them [35,36]; however, some groups have proposed that DPSCs might have an immunophenotype difference from that previously written by the ISCT to MSCs [18]. Regarding to the differentiation in three lineages, according to ISCT guidelines, DPSCs have already demonstrated their potential for differentiation in osteoblasts [15,20,26,37] and chondrocytes [20,37], but the differentiation in adipocytes has controversial results. Studies have shown few cells with lipid vacuoles or dye precipitates which may be interpreted as sporadic labeling [20,38,39].
Some authors have proved the differentiation through the expression of genes expressed present in adipogenesis (fatty acid binding protein - FABP, peroxisome proliferator-activated receptor gamma - PPARG, lipoprotein lipase - LPL) [20,37]. Previous researches have stated that this differentiation can occur later in DPSCs, after 5 weeks [40,41]. Head and neck derived MSCs, such as DPSCs, derive from the ectoderm, more specifically from the neural crest. Neural crest cells migrate along specific pathways to reach their destination and generate various cell types such as neurons, glial cells, melanocytes, connective tissue, dermis, tendons and rigid tissues, such as cartilage, bone and dentin. [42,43] Especially within the dental pulp, approximately 90% of the cells originated from the neural crest. Markers expressed by neural crest cells are widely expressed in the tooth pulp tissue and cultured DPSCs. In addition, DPSCs has been shown to have self-renewing ability and can be differentiated into other mature cells derived from the neural crest (e.g., neurons and glial cells), suggesting that the pulp still maintains some characteristics of the neural crest [43,44].
DPSCs have the potential to differentiate into neurons and promote the survival of neuronal cells from the injured site. DPSCs from rats cultivated in vitro produced neurotrophic factors and promoted neuron survival, while fibroblasts did not provide similar results [43]. Several authors have demonstrated the ability of DPSCs to differentiate and present neuronal markers [19,28,38,45]. The high expression of certain neuronal markers and neurotransmitter receptors by DPSCs also suggests that these cells can actively respond to signals from the neural environment and effectively integrate into injured nerve tissues, promoting the reestablishment of functional nerve connectivity [46]. The characteristics (differentiation and surface markers) presented by DPSCs are very similar with SCs from other tissues, making the dental pulp an excellent source for MSCs. DPSCs are important because they originate from ectoderm, the same origin of nervous tissue, suggesting being more promising than MSCs from other sources for use in future studies in neurodegenerative diseases. However, it is necessary to standardize the isolation methodology of DPSCs to be used on a large scale in regenerative medicine.
More BJSTR Articles : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.