Osseointegration of Zirconium Dioxide Implants With Microrough Surface Topography Compared to Titanium Implants - A Histological Study on Sheep
Introduction
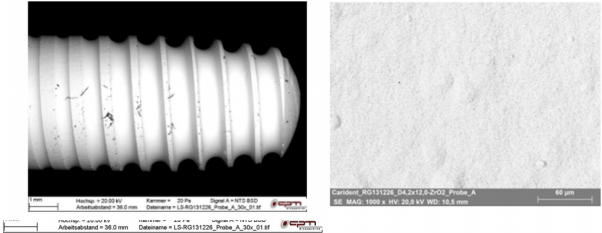
Dental implantology has established as an important treatment method in dental, oral and maxillofacial medicine. In addition to aesthetic and functional rehabilitation, the main function of implant dentistry is the prevention of peri-implant bone resorption as the main cause of peri-implant inflammation. The aim of this sheep study was to investigate the bony healing of zirconium dioxide implants with a special microrough surface using our currently developed lower jaw sheep model, see reviews [1,2]. As comparative samples were used titanium implants with acid-etched surfaces (OsteoActive®), which currently represent the “gold standard” in dental implantology. The K3 Pro Implant System® (Argon Medical, Germany™) is a titanium implant system with optimal surface micro roughness and surface topography and is characterized by a bacteria-proof connection on crestal and subcrestal level (Figure 2). The rough surface topography, the OsteoActive surface, results from acid etching. The ceramic implants (Carident AG™, Switzerland) used are showing in Figure 2. The qualitative surface examinations were performed with a Zeiss EVO MA15 scanning electron microscope in high vacuum (15kV / 30pA).
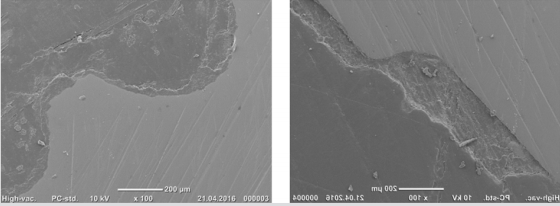
A BRUKER X-Flash 5010 EDX detector was used for elemental analysis of the sample surface. For the animal experiment 6 clinically healthy sheep (Stavropol Sheep) were used. The animals were 18 months old at the time of implantation and had a body weight between 60 and 67 kg (Committee of Stavropol State Medical University, AZ 98/4, 10/03/2011). The bone-to-implant interface was investigated by qualitative histological analyses using REM analysis (Figure 3). For this, the sheep lower jaw segments were histologically processed using Technovit 9100 New (PMMA), were embedded as described previously [3] and the osseointegration was qualitatively assessed. In addition, a TRAP analysis was performed to evaluate the cellular peri-implant bone regeneration process. The implants were distributed according to a randomized basic scheme, whereby 3 titanium and 3ZrO2 test specimens were used for each animal (“split-mouth design”). The 6-month bone healing time was chosen analogously to previous studies [4] which considered this time frame sufficiently for bony regeneration of the edentulous jaw sections in sheep. The histological evaluation of peri-implant bone formation was based on PMMA sections stained with toluidine Blu and polarization-optical images (Figure 4).
Figure 4: Peri-implant new bone formation around the ti-implants. In particular, the polarization-optical image (top left) shows the dense bone attachment to the Ti thread surfaces.
Using TRAP staining we evaluate the quality of cellular bone formation (Figure 5). Direct bone attachment to the implant surfaces was observed both in areas with trabecular bone components and along zones consisting mainly of bone marrow. Physiological bone remodeling around the inserted implants was observed in both trial groups in cortical areas without differences. This is also confirmed by the REM examinations performed in parallel (Figure 3). The newly formed peri-implant bone is dense and more osteons were found in direct contact with the implant surfaces. In conclusion, the histological examinations show direct bone attachment to the implant surfaces for both zirconium dioxide and titanium. An intermediate layer of loose connective tissue could not be detected [4]. These results support the conclusion that zirconium di-oxide implants have a comparable osseointegrative capacity as titanium implants with acid-etched surfaces.
Figure 5: Peri-implant new bone formation around the ceramic implant (trephane biopsy) with low inflammatory cell infiltration, TRAP and toluidine Blu staining.






No comments:
Post a Comment
Note: Only a member of this blog may post a comment.