Perineural Migration of Autologous Stem Cells and Their Role in The Functional Reparation of Injured Internal Organs
Introduction
It is paradoxical that the idea of perineural migration stem cell (PNMSCs) usage to initiate reparative processes in humans and animals [1-9] appeared in the article’s analysis of the pathological perineural invasion (PNI) mechanisms of cancer cells [10-13]. PNI is typical for various malignant tumors in the process of their manifestation [10-13]. Conditions for the implementation of PNI are pathological changes in the nerve cells and perineural matrix, as well as pathological viability, mobility and invasiveness of tumor cells, initiation of conditions for chemotactic involvement of tumor cells, activation of the adhesion processes of nerve and tumor cells, inhibition of autophagy, apoptosis and immunological surveillance of tumors by cells. The study of the PNI mechanism is important for blocking tumor progression and improving patient survival. Recent studies have demonstrated the critical role of nerves in tumor development [13]. The interaction of nerves with cancer cells is typical for various malignant tumors (stomach, pancreas, prostate, and brain cancer). Such a community of cancer and nerve cells is a kind of “black spot” for the patient, since it is accompanied by uncontrolled progress of the tumor process [13].
On the other hand, the development of cellular therapy inspired scientists and clinicians with the hope of improving the efficiency of reparative processes during the development of destructive processes in internal organs and tissues. The authors have gone through all stages of preclinical and clinical observations and officially conduct patient therapy in clinical hospitals of the Republic of Belarus. It is known [1,5,8,9,14] that practically all the internal organs of humans and animals contain stem cells, the reparative potential of which must be learned to use. In the early stages of the work, the authors of the article focused on experimental studies and clinical observations on diseases of the brain and heart [1-9]. Thus, in the heart of humans and mammals, due to the activation of endogenous heart stem cells, significant regeneration of cardiomyocytes is possible [7,8,14]. Introduction of autologous stem cells can lead to a significant recovery of the myocardium in heart diseases. The current tactics of clinicians are based on radical technologies, for example, heart transplantation, replacement of the heart in perspective with a portable artificial device, implantation of heart pacemakers, etc. There are objective reasons for choosing such tactics.
The heart of man and mammals is a highly differentiated organ, and so far, it has not been possible to determine the equivalent substitution of a heart transplant in evidence. Clinicians begin to activate the reparative potential of endogenous heart stem cells in the late stages of the development of pathological processes in the heart. Such tactics have little success, are financially costly, and will never cover the entire contingent of heart diseases in need of radical treatment. The axiom that the healing of myocardial infarction occurs through the formation of scar tissue. The progression of pathological myocardial remodeling in patients waiting for help is accompanied by the development of heart failure and sometimes fatal outcome before the start of radical therapy. Unfortunately, there is still an open question whether new scientific discoveries can provide a convincing rationale for extensive clinical trials of stem cell therapy for heart and vascular diseases. The authors of the article chose the method of perineural implantation of SCs for the purposeful migration of SCs to the area of internal organ damage (heart, lungs, liver, pancreas, stomach, spleen, kidneys). This therapy is advisable to carry out at the earliest stages of development of pathological processes in the internal organs.
Central and Peripheral Pathways of Perineural Stem Cell Migration
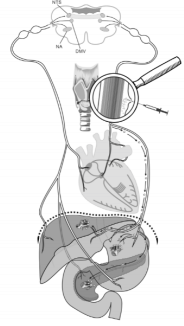
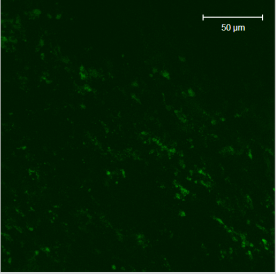
Cellular technologies with the use of autologous SCs open up new possibilities for the treatment of socially significant diseases in the early stages of their development. This tactic of treatment is preventive and is aimed at preventing the manifestation of fatal pathological processes. The clinical results of the application of cellular technologies, unfortunately, are not always sufficiently convincing. In this regard, the infusion of stem cells into the bloodstream for diseases of internal organs is still considered experimental and research [14]. The authors of the article focused attention in experiments on animals [1,2,4,6-9] and in observations in clinical conditions [3,5] on the potential of SCs with their perineural administration. In experiments on 3 adult male Wistar rats weighing 200-220g at the time of the experiments have been chosen. All surgery manipulations were performed under ketamine-xylazine-acepromazine anesthesia (55.6, 6.6 and 1.1mg/ kg, respectively, i/p) Figure 1. All rats received 10 thousand SCs in 10µl culture medium in perineural space of vagus nerve at the middle of the neck (Figure 1). SCs were marked with monoclonal antibodies to PKH67 Green Fluorescent Cell Linker. Immediately after the SCs were introduced into the perineural space, laparotomy was performed in the upper abdominal cavity. Gently using an electro coagulator, they touched the surface of one of the three internal organs in each animal: liver, stomach, and pancreas for one second. Figure 1 shows schematically the areas of damaged internal organs. If necessary, hemostasis was performed and then the abdominal cavity was subsequently sutured. All rats were decapitated in one week after surgery and horizontal serial every internal organ slices 8µm in thickness were prepared using Microm HM525 (Germany) cryostat. SCs distribution in damaged internal organs was visualized using Zeiss AxioVert 200M fluorescence microscope with Zeiss AxioCam HRm CCD camera. Figure 2 shows distribution of PKH67 Green Fluorescent Cell Linker labeled SCs in the damaged area of stomach.
Conclusion
Conservative therapy of pathological processes in the internal organs is often ineffective. For example, liver cirrhosis is the main cause of death in the development of pathological processes in the liver [15]. The most effective treatment is limited to liver transplantation, which is not available to all patients and is a very expensive method. In this regard, the use of stem cells to regenerate the liver appears to be a promising method [15,16]. The data obtained in the treatment of MSCs-conditioned medium confirmed the trophic effects of MSCs, such as increased proliferation and decrease in hepatocyte apoptosis after the activation of several anti-inflammatory and anti-fibrotic cytokines [15,16]. In addition to this, attempts have been made to treat patients with cirrhosis with induced pluripotent stem cells [15]. These attempts do not consider the negative side effects of using such cells, the most dangerous of which are teratogenic effects [15]. Most of the procedures for the introduction of SCs were intravenous [15,16], but there are references to the introduction into the hepatic artery [17], as well as the use of systemic application of SCs for cystitis [18], and the possibility of directed movement of SCs using physical factors [19]. The results of the perineural administration of SCs look more promising, especially since in experiments and in clinical conditions the methods of perineural delivery of SCs to different parts of the brain [1-8], as well as to the liver, stomach, pancreas [9], have already been positively tested.
Acknowledgement
This pooled analysis was funded by OOO “Synergy”, and by innovative fund of Brest Regional Executive Committee (2017- 2019), and by BRFFI B18P-227.
More BJSTR Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.