Prediction of Fluid Responsiveness in Mechanically
Ventilated Critically Ill Patients with the Affection of
Positive End-expiratory Pressure
Previous studies have shown that in the process of fluid
resuscitation of septic shock and other critically ill patients, fluid
resuscitation deficiency and excess liquid load are related to
poor prognosis in patients [1,2]. To improve tissue perfusion, the
hemodynamic assessment of critically ill patients is an indispensable
treatment step. The factors that decide whether the amount of
liquid supplement is appropriate, not only refer to the capacity
of blood vessels, but also include the capacity responsiveness.
According to Frank-Starling’s law, in the curve ascending branch
(preload depending region), load increase will make the stroke
volume (stroke volume, SV) rise significantly. In the platform
stage (preload independent area), the changes of preload will not
affect the SV load and fluid increase will be harmful. Therefore,
determining the position of patients in the curve, i.e. determining
whether the patient has the capacity responsiveness is crucial.
Previous statistics have manifested that in the intensive care unit
(intensive care unit, ICU), the patients with sepsis and septic shock
showing reactive capacity only account for 43.5%, and blindly
expansion does not continuously improve the hemodynamic status
of patients [3].
The commonly used indexes such as central venous pressure
(central venous pressure, CVP) and other indexes are greatly
affected by the static capacity of cardiovascular fitness, myocardial
contractility, chest cavity pressure and other factors [4]. The value
of volume status assessment is not high [5,6]. And the numerical
value of preload cannot represent the capacity responsiveness
of the body [4]. Pulse-induced Contour Cardiac Output (Pulseinduced Contour Cardiac Output, PiCCO) can dynamically reflect
the changes of cardiac output (cardiac output, CO) and SV. Although
PiCCO is regarded as the “gold standard” to assess the capacity
responsiveness, the procedure of this method is cumbersome and
the materials are expensive [7]. Furthermore, the modern critical
care medicine attaches great importance to avoid unnecessary
catheter for the reason that it may directly or indirectly increase
the mortality through catheter-related bloodstream infection [8].
In the past two decades, critical care medicine has been gradually
turning from the traditional high risk of invasive monitoring to the
noninvasive monitoring.
Therefore, bedside ultrasound is well received by clinicians [9].
Another advantage of ultrasound is that, in a relatively short period
(usually less than 30 min), it can provide complete information
about blood vessels and hemodynamics. The index that bedside
ultrasound evaluates the capacity status of patients includes
static index and dynamic index. Many studies have confirmed that
ultrasound static index not only has the advantages of convenient,
noninvasive, but also can completely replace the invasive traditional
index. It has been reported that the aspect ratio of internal jugular
vein measured by ultrasound was less than 0.83 could predict
CVP < 8cmH2
O [10]. Other reports suggested that the diameter
of IVC was less than 2 cm could predict CVP < 10mmHg, and the
sensitivity and specificity reached 85% and 81% respectively [11].
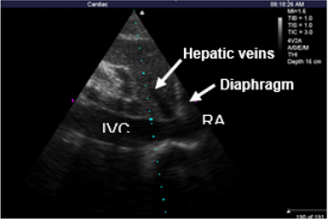
Additionally, for the patients whose breath were controlled by
mechanical ventilation, the IVC diameter of end expiratory which
was measured under short axis of the right atrium (The crosssectional view) using M model (M mode) of TTE and the right atrial
pressure measured by SVC catheter were linear correlation [12].
However, using the effect of static ECHO parameters to predict
fluid responsiveness in critically ill patients is poor unless the
patients obviously show hypovolemia [13]. But in the modern ICU
care level, patients with obvious hypovolemia are not common
[14,15]. In the current clinic, using heart’s reaction to mechanical
ventilation or spontaneous breathing cycle and the degree of
variation of respiratory under intrathoracic pressure change, i.e.
using “heart lung interaction” to observe SV changes of patients
after cardiac preload affected by pleural pressure, could determine
the capacity responsiveness of patients. These indexes include SVV
(Stroke Volume Variation, SVV) [16], PPV (Pulse Pressure Variation,
PPV) [3], artery VTI (velocity-time integral, VTI) [14], the variation
of SVC [17] and IVC [13,18] and other indexes. The treatment process
of the critically ill patients with respiratory failure hemodynamics
instability, is always needed to apply noninvasive positive pressure
mechanical ventilation. And positive end expiratory pressure
(positive end expiratory pressure, PEEP) is a commonly used
function in mechanical ventilation settings. But the existence of
PEEP can reduce the pressure gradient to decrease venous reflux
by increasing intrathoracic pressure and lung volume, which would
cause hemodynamic changes [19].
However, the effect of PEEP on the dispensability index of
the inferior vena cava (the dispensability index of the inferior
vena cava, dIVC), inferior vena cava diameter (IVCdmax) and other
respiratory variability indexes of patients measured by ultrasound
has not been reported until now. In this study, SVV, dIVC dynamic
indexes and IVCdmax static index of the same group of critically ill
patients were measured by monitoring the PPV and ultrasound, to
further explore the application value of the above indexes in the
capacity responsiveness evaluation of patients with mechanical
ventilation, and to analyse the effect of PEEP on the mechanical
ventilation index and common clinical capacity evaluation index
including the above indexes.
The Research Object
The Research Object: 42 patients needed mechanical
ventilation in department of ICU of the Second Affiliated Hospital
of Anhui Medical University from February to November in
2014 (20 male and 22 female aged from 22 to 72 years, average
age: 47.45±13.28). Acute physiology and chronic health
evaluationⅡ(APACHⅡ): 13.48±3.53. The 42 patients are including
17 septic shock patients with perforation of colon resulting in diffuse
peritonitis, 10 severe pneumonia patients, 6 severe acute
pancreatitis patients, 6 liver and spleen rupture complicated
hemorrhagic shock, and 3 upper gastrointestinal hemorrhage.
Inclusion Criteria:
a) Patients had invasive mechanical ventilation; vasoactive
agent wasn’t used or had been evacuate
b) sinus rhythm.
Exclusion Criteria:
a. Existing fluid infusion test contraindication (acute
coronary syndrome, cardiogenic shock and evidence showing
overload fluid)
b. being obvious right ventricular dysfunction, right heart
failure and tricuspid regurgitation
c. being younger than 18 years of age
d. being gestation
e. being intra-abdominal hypertension, bladder pressure
measured by catheter >16cmH2O
f. existing pneumothorax or pulmonary bulla Without
drainage.
Conforming to the standards of medical ethics, this study
was approved by hospital ethics committees. All treatments and
inspections had informed consent of the patients or their families.
Research Methods
Mechanical Ventilation Mode and Parameter Setting: Using
midazolam and/or propofol gave patients sedation. Breathing
machine (PB840) of Nellcor Puritan Bennett (America) was used in
invasive mechanical ventilation, Assist/Control mode, VT: 6~8ml/
Kg, keeping breathing frequency: PaCO2
=35~45mmHg. From right
subclavian or jugular vein into central venous catheters, imbedding
arterial puncture tube from radial artery puncture, all connecting
Intellivue MP60 monitor (Phillips, Germany) monitoring HR, ABP,
CVP, ECG and SpO2
. Initial setting PEEP=0, recording PIP and Pmean;
ultrasonic measured and recorded each index in the meantime.
Then fluid responsiveness test was conducted, after which each
index was recorded again. Hereafter PEEP was increased to 5,
10, 15 cmH2
O respectively for 5min, then PIP and Pmean were
recorded again, with each indexes being measured and recorded
by ultrasound. During the above steps, test would be stopped if the
indexes showed Pmean>35mmHg or PIP> 45mmHg.
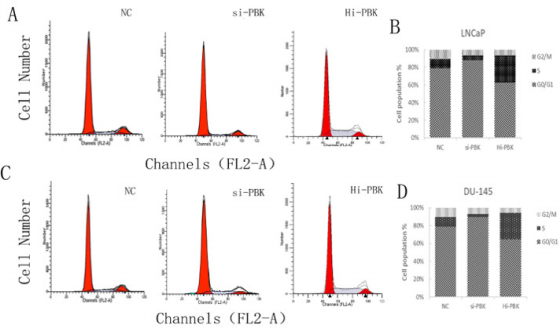
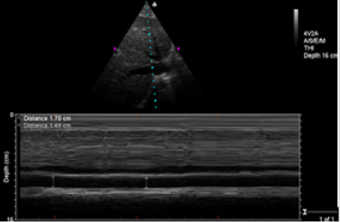
Ultrasonic Testing and PPV Monitoring Method: In complete
mechanical ventilation control mode, below indexes were measured
by M-Turbo bedside portable ultrasonic apparatus of SonoSite
(America): ①CO (cardiac output) ②measuring SV and recording
SVV %=(SVmax﹣Svmin)/SVmean, SVmax and SVmin being the
mean value of 4 values in 30s, SVmean being the mean value of
all values. ③Measurements of IVCdmax , IVCdmin and dIVC were
performed from long-axis 2-dimensional subxiphoid views using M
mode (Figure1), All measurements were made within 2 cm of the RA
origin of the IVC(Figure2), dIVC= (IVCdmax − IVCdmin)/0.5(IVCdmax +
IVCdmin) [13]. Ultrasonic testing were respectively conducted
by an experienced ultrasound diagnostics doctor and a trained ICU
doctor. Each observation indicator was took the average after being
measured three times. During mechanical ventilation, the arterial
pressure waveform was drawn from invasive arterial pressure
monitor, recording PPmax and PPmin, PPV(%)=( PPmax-PPmin)
/[(PPmax+PPmin)/2]×100%[20].
The Positive Criteria of Volume Expansion Test: After
intravenous drip 500ml normal saline (NS) in 20min, Patients were
classified as responders to fluid loading if their CO increased under
TTE by at least 15%[4]. The test would be stopped if patients
had overload clinical manifestations (shortness of breath obviously,
lung moist rale increasing or aggravated myocardial ischemia
indicated by electrocardiogram).
Main Outcome Measures: ①The threshold value, sensitivity
and specificity of PPV, SVV, IVCdmax and dIVC to predict fluid
responsiveness in ventilated critically ill patients; ②The effects of
increasing PEEP on indexes of Pmean, PIP, CO, CVP, PPV, SVV, IVCdmax
and dIVC during ventilation in fluid responsiveness positive and
negative groups separately.
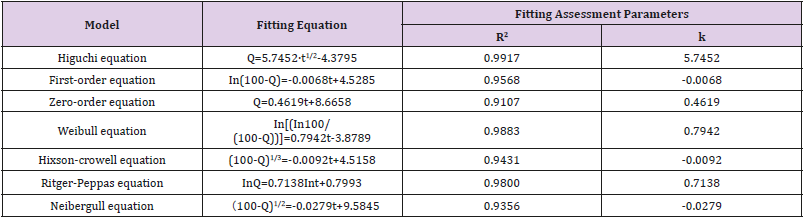
Statistic: By SPSS 17.0, Measurement data being recorded in
( ±s), pair T test, independent-samples T test; Receiver operator
characteristic curve (ROC) was be used in analyzing the value of SVV,
PPV, IVCdmax and dIVC predicting fluid responsiveness showed by
area under the curve (AUC) (95%CI); Kappa consistency check the
consistency of SVV, PPV and dIVC predicting fluid responsiveness;
Between-Subjects factors were compared by variance analysis and
linear trend test; pairwise comparison was conducted by dunnet-t;
variable correlation was analyzed by spearman correlation analysis;
P<0.05 was regarded as statistical significance.
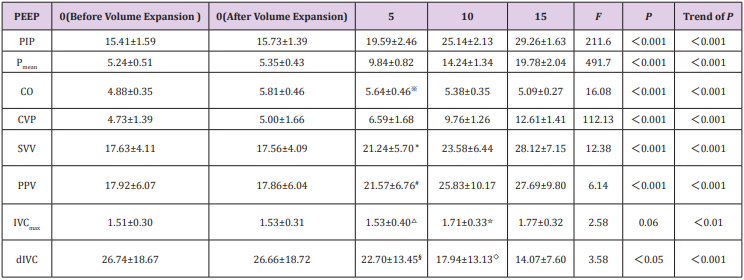
Basic Information
In the 42 Volume Expansion Tests, 2 Cases were Stopped
because of Volume Overload: As a result, 22 of the finally
volume load tests were positive and 18 were negative. With PEEP
increasing, pneumothorax and other complications didn’t happen.
There were no statistically differences of PIP, Pmean, CVP, SVV, PPV,
IVCdmax and dIVC between before and after volume expansion tests.
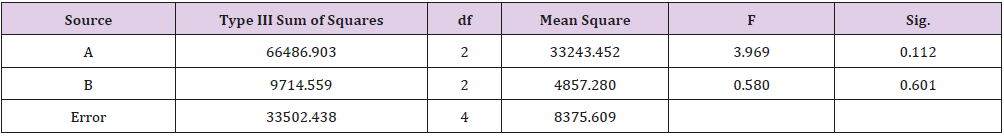
However, CO increased significantly (P=0.00). With different PEEP,
TTE indexes of positive group and negative group were showed in
Table 1 and Table 2.
F
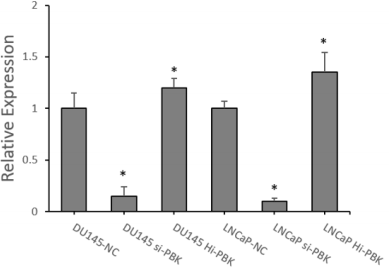
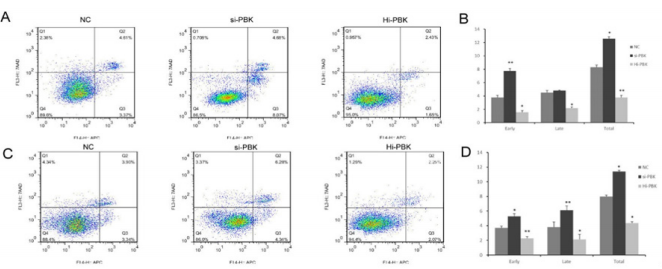
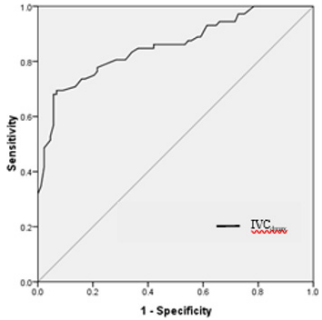
SVV, PPV, IVCdmax and dIVC Predicting Fluid Responsiveness
Analyzed by ROC Curve: The area under ROC curve (AUC) for
PPV predicting fluid responsiveness was 0.94 (95%CI: 0.89~0.98,
P<0.001). The PPV threshold value of 13.5% before volume
expansion had the sensitivity of 94.3% and the specificity was 84.7
% for prediction of fluid responsiveness. The AUC for SVV predicting
fluid responsiveness was 0.98 (95%CI: 0.97~1.00, P<0.001). The
SVV threshold value of 13.2% before volume expansion had the
sensitivity of 98.9% and specificity of 88.9% for prediction of fluid
responsiveness. The AUC for dIVC predicting fluid responsiveness
was 0.95(95%CI: 0.91~0.98,P<0.001). The dIVC threshold value
of 12.40% before volume expansion had the sensitivity of 80.7%
and specificity of 98.6% for prediction of fluid responsiveness.
(Figure 3). The AUC for IVCdmax predicting fluid responsiveness
was 0.85(95%CI: 0.79~0.91,P<0.001), the IVCdmax threshold
value of 2.03 before volume expansion had the sensitivity of 68.1%
and specificity of 94. 3% for prediction of fluid responsiveness
(Figure 4).
Kappa Test Consistency Analysis of SVV, PPV and dIVC
Predicting Fluid Responsiveness: According to ROC results,
taking SVV > 13.2, PPV>13.5 and dIVC>12.4 as the cutoff value of
fluid responsiveness to consistently analyze the results, showing
that the Kappa coefficient of SVV and PPV was 0.729,P<0.001;
The Kappa coefficient of SVV and dIVC was 0.607, P<0.001; The
Kappa coefficient of PPV and dIVC was 0.607, P<0.001.
The influence of PEEP on airway pressure and TTE indices
a) In fluid responsiveness positive group, with PEEP
increasing, there are overall differences among groups about PIP,
Pmean, CVP, CO, SVV, PPV and dIVC (P<0.05). IVCdmax increased
with PEEP, there are no significant differences in comparison
among groups (P>0.05), while there are significant differences
in linear trend (P<0.01). After pairwise comparison between
PEEP5
, PEEP10, PEEP15 and PEEP0
(after volume expansion test,
the following are the same) respectively by Dunnet-t, there were
significant differences of IVCdmax and dIVC between PEEP15 and
PEEP0
, while there were significant differences of CO, SVV and PPV
between PEEP10, 15 and PEEP0
. There were significant differences of
CVP between PEEP5
, 10, 15 and PEEP0
(Table 1).
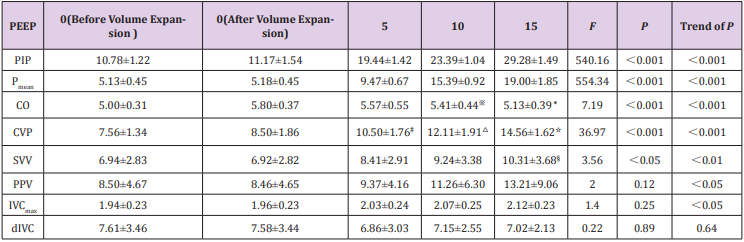
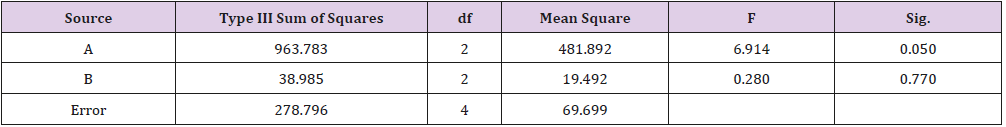
b) In fluid responsiveness negative group, with PEEP
increasing, there are overall differences among groups about PIP,
Pmean, CVP, CO and SVV(P<0.05). PPV and IVCdmax increased
with PEEP, there are no significant differences in comparison
among groups (P>0.05), while there are no significant differences
linear trend (P<0.05). dIVC increased with PEEP, there are no
significant differences in comparison among groups and linear
trend (P>0.05). After between PEEP5
, PEEP10, PEEP15 and PEEP0
respectively by Dunnet-t, there were no significant differences
between PEEP5
, 10, 15 and PEEP0
respectively about IVCdmax, dIVC and
PPV; there were significant differences between PEEP15 and PEEP0
about SVV. There were significant differences between of PEEP10, 15
and PEEP0
respectively about CO. There were significant differences
between PEEP5
, 10, 15 and PEEP0
respectively about CVP (Table 2).
c) Spearman Variable Correlation Analysis: In fluid
responsiveness positive group, There are positive correlation
between the SVV(r=0.58,P=0.000), PPV(r=0.50,P=0.000
), IVCdmax(r=0.35,P=0.001)and PEEP respectively. There
are negative correlation between the CO(r=-0.60,P=0.000
), dIVC(r=-0.59,P=0.000)and PEEP respectively. In fluid
responsiveness negative group, there are positive correlation
between the SVV(r=0.35,P=0.003)、PPV(r=0.40,P=0.000
), IVCmax (r=0.28,P=0.019)and PEEP respectively. There are
negative correlation between the CO and PEEP(r=-0.54,P=0.000
); it had no correlation between dIVC and PEEP (r=-0.04
,P=0.771).
The Value of SVV, PPV, dIVC and IVCdmax Evaluating
Fluid Responsiveness
Using three dynamic indicators (SVV, PPV and dIVC) in our study,
we selected 13.2%, 13.5% and 12.4% as cut-off values respectively
to evaluate fluid responsiveness. They all have sensibility and
specificity. Kappa consistency test analysis suggested that the
results had consistency. When positive pressure ventilation patients
are in inspiratory phase, many factors lead to the increase of SV
and PV, including transpulmonary pressure increase compresses
the pulmonary vasculature, left ventricular preload increase and
pleural pressure increase., aortic vascular transmural pressure
decrease, left ventricular afterload decrease, right atrial filling
decrease, ventricular septal shift right inducing left ventricular
filling increase, while the right ventricular RV pressure decrease
reducing the pericardium, left ventricular to pulmonary venous
factors venous return. Whereas exhale opposite [21]. Therefore, the
sensitivity of the two indicators is very high, reaching 98.9% and
94.3% respectively. Researches by the Feissel [13] have indicated
that the sensitivity and specificity are 93% and 92% respectively
when 12% as a cut-off value to predict the volume responsiveness.
It is similar to the results of this study. The sensitivity of dIVC
is 80.7%, lower than the other two. Considering that IVC locates
in the abdominal cavity, the diameter of the respiratory variability
is not only affected by the heart-lung interaction, but also relevant
to the venous external pressure produced by the movement of
diaphragmatic with the respiratory changes of thoracic abdominal
cavity and right atrial pressure (RAP) gradient. Nevertheless, the
sensitivity of dIVC is still much lower than previous report (93%)
[13]. It considers that many patients after abdominal operation
in this group influence the measurement of IVC by TTE. IVCdmax
is a static volume indicator. When positive pressure ventilation
patients are in inspiratory phase, the diaphragm decrease, intraabdominal pressure increase, RAP gradient increase, the inferior
vena cava filling and the effect is largest to end inspiration [22]. The
ROC curve analysis results by TTE to measure IVCdmax to evaluate
capacity responsiveness in this study show that using IVCdmax 2.03
as the threshold value before fluid load to predict the sensiti
fluid responsiveness is 68.1%, the specificity is 94.3%.
By comparing IVC diameter, CVP [4,11,23] and RAP [12] through
the TTE, previous research considers that it has a good correlation
between them. This study also suggests that although IVCdmax is a
static volume indicator, it still shows the value of better prediction
of fluid responsiveness to a certain degree. This may be related
to these reasons such as there are mostly surgical patients in this
group, the average age is less than 50 years, previous heart-lung
function better, less complication, less factors effect on static volume
indicator. But the area under ROC curve of IVCdmax is significantly
lower than SVV, PPV and dIVC, suggesting that the value of dynamic
volume indicator is better than the static volume indicator.
The Effect of PIP, Pmean, CO and CVP on PEEP
The optimal PEEP can dilate small airway throughout the
respiratory cycle and maintain the end expiratory alveolar open,
increase functional residual capacity (FRC), improve the chest wall
compliance, reduce the elasticity resistance of respiratory system.
The setting of PEEP increases transpulmonary pressure and pleural
cavity pressure, thereby increasing the airway pressure when
positive pressure ventilation. This study finds that the values of
PIP and Pmean in all patients of the volume expansion test (+) and
(-) group significantly rise with the increase of PEEP, P value and P
value trend are both less than 0.001 between groups. This result
indirectly suggests that high PEEP setting may lead to excessive
overexpansion of the lungs and produce lung injury. With the
increase of PEEP, CO of both groups decreases. This is also related
to the decline of cavity venous return induced by intrathoracic
pressure increase caused by PEEP, the reduction of right ventricular
preload, eventually the decline of left ventricular stroke volume. But
there are no statistical differences comparing PEEP5
and PEEP0 of
CO in two groups, suggesting that the body can play a compensatory
function to a certain extent to offset the adverse effects on the
circulation after a slight increase in PEEP. As a traditional volume
evaluation indicator, CVP has extensive application in clinic. But
as a static pressure marker, it is influenced by cardiac function of
patients, compliance of thorax and many other factors. The changes
of pleural pressure that caused by PEEP becomes the important
factor of the pressure changes of the superior venous located
at thorax. The data also indicates when PEEP reaches 5 cmH2
O,
volume expansion test (+) and (-) group show statistical difference
comparing with PEEP0
.
The Effect of PEEP on SVV, PPV, dIVC and IVCdmax of Volume
Expansion Test (+) Group
This research discuses that the effect of PEEP on the dynamic
capacity indicators such as SVV, PPV and dIVC in volume expansion
test (+) and (-) group. The results show when PEEP reaches 10
cmH2
O, SVV and PPV both have statistical differences comparing
with PEEP0
in volume expansion test (+) group. However, dIVC
shows statistical difference comparing with PEEP0
when PEEP
reaches 15 cmH2
O, suggesting that dIVC is slight affected by
PEEP in a certain range. This is consistent with the result of the
high specificity of evaluation capacity reaction of dIVC as stated
above. Spearman variate relativity analysis shows that SVV and
PPV are positive correlation with PEEP, as confirmed by previous
researchers [24]. In positive pressure ventilation patients on the
basis of LVSV increase with inspiratory phase, PEEP may make the
lung expansion and left ventricle extrusion, and further intensify
SV of the inspiratory phase. However, PEEP increases intrathoracic
pressure, leads to further decrease LVSV with expiratory phase,
and make SVV and PPV increase. With the increase of PEEP, intraabdominal pressure further increases, and RAP gradient increases
[25]. This study shows that IVCdmax gradually increases in the volume expansion test (+) group and P value between groups is less
than 0.01. The IVCdmax values of PEEP15 and PEEP0
have statistical
differences.
This result is consistent with the research by Schefold [23]. With
the increase of PEEP, dIVC of the volume expansion test (+) group
gradually decreases, P value between groups is less than 0.05, and
the trend of P value is less than 0.001. The dIVC values of PEEP15
and PEEP0
have statistical differences. Spearman variate relativity
analysis shows that dIVC is negative correlation with PEEP. The
reason of above results may be that the setting of PEEP leads to
IVC diameter increases in end inspiration, IVC diameter increases
in end expiration and increases more than end inspiration, thus
make dIVC decrease. Kircher [26] thinks that collapsibility index
less than 50% is effective indicator to evaluate right atrium more
than 10 mmHg, using inferior vena cava collapsibility index (IVCCI) to evaluate right atrium pressure of autonomous respiration
patients. It also suggests that higher right atrium pressure, less
breath variety of IVC. The animal model test of Duperret S1 [27]
demonstrates that abdominal cavity pressure increasing leads
to breath variety of IVC decrease, especially hypovolemia. These
results indirectly verify our conclusion.
The effect of PEEP on SVV, PPV, dIVC and IVCdmax of Volume
Expansion Test (-) Group
In volume expansion test (-) group, SVV and PPV are positive
correlation with PEEP increase. SVV shows statistical difference
comparing with PEEP0 when PEEP reaches 15 cmH2
O. With the
increase of PEEP, the trend of P value of IVCdmax is less than 0.001.
But there are no statistical differences between increase groups and
PEEP0
. P value the trend of P value of dIVC between groups is more
than 0.05. Spearman variate relativity analysis shows that PEEP
has no correlation with dIVC. The research about SVV by Michard
et al. [19] reports that the positive correlation between PEEP and
SVV is related to preload state. Our study about volume expansion
test (+) and (-) group comparison indicates that the effect of
PEEP on dynamic capacity responsiveness evaluation indicator is
related to the location at starling curve of patients. This effect is
more significant when locating on the steep rather than on the flat
portion of the Frank-Starling curve. In the condition of full preload,
the self-regulating mechanism of patients work, dynamic capacity
responsiveness evaluation indicator is less influenced by PEEP.
This study selects various cases including many related
diseases and the different pathophysiological states may affect
the results. For example, although the IAP > 16 cmH2O intraabdominal hypertension patients have been ruled out in this group,
but some patients experienced abdominal operation, abdominal
wall compliance decrease causing by abdominal postoperative
may influence the results of this study [28]. The effect of PEEP
settings on respiratory mechanics in patients not only reflects on
the changes of the intrathoracic pressure and transpulmonary
pressure, but also the increase functional residual capacity and/
or a decrease pulmonary vasoconstriction induced by hypoxia to
change the heart load [19]. Thus, it has an impact on the dynamic
volume responsiveness evaluation. This study is according to
the classic volume load test standard [4], using 500 ml saline to
carry out volume load test (+). Although there are no significant
differences between parameters of the (+) groups before and after
the load test, but it cannot avoid the interference of observing
PEEP influence caused by preload increase. These need to design
more strict animal experiments and clinical studies in the future to
further elucidate the internal relationship.
This work was supported by the Scientific and technological
project of Anhui Province (Grant No. 1301042206). Anhui
Provincial Natural Science Foundation (Grant No. 1508085QC49),
and the doctoral research fund project of the Second Affiliated
Hospital of Anhui Medical University (Grant No.2014BKJ034).
For more Articles: https://biomedres01.blogspot.com/