Influenza Surveillance Among Hospitalized Children in Shenzhen Children’s Hospital, 2012-2016
Introduction
Influenza is an acute respiratory tract infection caused by an influenza virus. Highly contagious, it spreads rapidly and widely and exhibits seasonal changes in infection rates. The influenza virus is one of the major causes of acute respiratory tract infection in the world. In non-pandemic situations, annual flu epidemics are not only serious threats to susceptible people, but also have important effects on public health [1]. Children are the most susceptible group and the most likely to spread the infection. During annual flu seasons, the illness mainly occurs in children, especially schoolchildren aged 5-17 [2]. Since the 2009 H1N1 pandemic, there have been a large number of influenza A (H1N1)-related deaths reported [3-6]. China is recognized as a flu-prone country. Herein, influenza surveillance among Chinese pediatric patients will contribute not only to the understanding of the trends of influenza in China but also to the understanding of the clinical characteristics of children with flu infection. Importantly, it will provides scientific evidence to support further studies. Current surveillance projects in China focus mainly on outpatients with mild flu-like symptoms, and there is a dearth of data on severe and critically ill hospitalized children. Since January 2012, we have conducted a routine 2009 H1N1 influenza A testing on children hospitalized in Shenzhen Children’s Hospital for lower respiratory tract infection.
Materials and Methods
Case Cohort
A total of 28,883 children were selected from 2012-2016. They were hospitalized in Shenzhen Children’s Hospital due to lower respiratory tract infections. 18,216 were male and 10,667 female. They ranged in age from 1 month to 14 years.
Methods
After admission, a throat swab specimen was collected from each child and sent to the virus laboratory for influenza A virus antigen detection. The colloidal gold test was used per the manufacturer’s instructions. A color change in a specific zone was considered positive. All deaths were tested for influenza A nucleic acid.
Statistical Analysis
SPSS 16.0 software was used for data analysis. Descriptive statistics were used to analyze influenza epidemic data. Age distribution was analyzed. Count data are expressed in (%). Intergroup comparison was performed using Chi-square test (χ2) and P<0.05 was considered statistically significant.
Results
Detection of Respiratory Tract Influenza A Virus
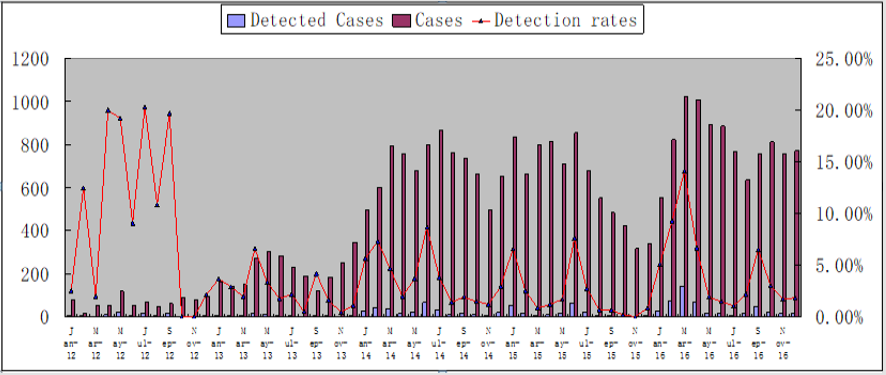
From January 2012 to December 2016, a total of 28,883 specimens were tested and 1117 (3.87%) were found to be positive. The detection rates in different seasons (spring, summer, autumn, and winter) were 4.76%, 3.53%, 2.28%, and 4.63% respectively. The positive detection rates in 2012, 2013, 2014, 2015, and 2016 were 9.50%, 2.47%, 3.75%, 2.62%, and 4.84% respectively.
Time Distribution
From January 2012 to December 2016, the positive detection rate of influenza virus in Shenzhen Children’s Hospital peaked twice. The first peak occurred in March-August 2012, and the second in March 2016. Sporadic cases were observed in April 2013, February 2014, June 2014, January 2015, and June 2015 (Figure 1).
Gender Distribution
Among the positive cases, 750 were male (750/18216, 4.12%) and 367 were female (367/10667, 3.44%). The chi-square test (χ2=8.287, P=0.004) showed the male group to have a significantly higher positive rate than the female group.
Age Distribution
The following were the detection rates for different age groups: 3.48% (179/5143) for age 0-6 months, 3.25% (308/9473) for 6-12 months, 4.48% (321/7167) for 1-3 years, 4.79% (233/4868) for 4-6 years and 3.41% (76/2232) for 7-14 years. The 4-6-yearold group had a significantly higher detection rate than the 0-6 months, 6-12 months, or 7-14-year-old groups (chi-square values and P values were 10.8, P=0.001; 20.8, P=0.000, and 8.47, P=0.004, respectively).
Influenza-associated Deaths in Critically ILL Children
From 2012-2016, a total of 8 children were admitted to the intensive care unit due to the flu infection, and 7 of them died. These children ranged in age from 10 months to 4.3 years. 4 were male and 3 were female. The main clinical manifestations included fever, cough, shortness of breath, and progressive dyspnea. Three cases had convulsions, persistent seizures, coma, or other neurological manifestations. One death occurred in May 2012, a 3-year-old boy who died from influenza A-related encephalopathy, brain herniation and pneumonia. The other 6 deaths occurred in March and May 2016. Three of these patients developed influenza-associated acute necrotizing encephalopathy. Three cases had underlying diseases, 1 each of acute lymphoblastic leukemia (with chemotherapy-induced myelosuppression), familial necrotizing encephalopathy (with an autosome dominant form), and nephrotic syndrome. The other two cases without underlying disease developed a complication of flu: severe sepsis caused by invasive streptococcus pneumoniae. All deaths had been infected by 2009 H1N1 influenza A virus.
Discussion
H1N1 influenza A virus is still a common cause of respiratory tract infection that seriously threatens child health. Most children have mild illness and only show flu-like symptoms such as fever and cough. Some children, however, are more likely to develop flu complications, such as severe pneumonia and neurological complications, which could be fatal [7]. Because influenza surveillance in China has mainly focused on outpatients at sentinel hospitals, it is difficult to extract data on critical illness and influenza-related death. Therefore, it is necessary to conduct flu surveillance among hospitalized children, especially critically ill children. According to the data of positive detection rate and season distribution, H1N1 influenza A viruses are most common during spring and summer. After flu season peaked (spring, summer and autumn) in 2012, flu activity started to drop although there were still sporadic cases observed in spring and summer. Since October 2012, the rate of H1N1 influenza A infection has decreased significantly. One reason for this decline could be that the majority of people have gained protective antibodies to H1N1 after their infection in 2009 H1N1 pandemic. Another important reason could be the flu vaccines recommended for susceptible people including preschool and schoolchildren [8-9].
Previous studies have shown that the flu in northern China mainly occurs in winter, but the flu in the south has no seasonality and can last a whole year. There could be 2-3 flu peaks each year, one in winter and spring, and the other in summer and autumn. However, the flu activity peaked mainly in spring during our 5-year surveillance. Based on the data in our hospital, H1N1 influenza A positive rate was highest among children 4-6 years old. A similar age distribution has been observed among children in Hebei Province, which showed the highest detection rate in the 4-6 and the 7-14-year-old groups. Children in these age groups are mainly preschool and school-age children. They lack immunity to influenza and tendency to stay in crowded places for long periods of time are two main factors that cause the flu to spread among these high-risk population. Therefore, it is of great significance to develop strategies for the prevention and control of influenza. Schoolteachers and staff need to increase their knowledge and awareness of importance of flu prevention and improve their abilities to deal with emergency situations. Parents also need to be educated about preventing the spread of the flu.
Pneumonia is the most common complication of influenza. It can be primary viral pneumonia or secondary bacterial infection. A few severe cases can quickly deteriorate in a short term, with respiratory failure, respiratory distress syndrome and even neurological complications such as encephalitis or encephalopathy. These severe complications are the main causes of influenzainduced death [10-12]. Based on the data from multi-center studies in China, 49 (6%) hospitalized children developed encephalopathy and encephalitis as the complications of 2009 H1N1 Influenza and 13 deaths (13/49, 26.5%) occurred. It has been suggested that H1N1 flu-induced encephalopathy or encephalitis is also one of the major causes of child deaths in our country [13]. Of the 7 deaths observed in our surveillance, 3 were children who died from acute necrotizing encephalopathy and 2 cases died from secondary bacterial infection, which is basically consistent with domestic report. It is suggested that H1N1 flu can cause serious harm during both pandemic and non-endemic periods and herein should be given more attention.
Early recognized risk factors for influenza complications are: children under 5 years of age and the elderly over 65 years of age, obesity, pregnant women and perinatal women, previous underlying disease. Subsequent studies have shown that nosocomial influenza a virus infection, delayed treatment, and admission to the PICU were independent risk factors for influenza death [14-15].A recent meta-analysis indicated that the previously recognized risk factors for influenza-related complications, including pregnancy and ethnicity, had a low level of evidence and could not be confirmed as high risk factors, requiring further confirmation and research [16]. In the current study, 3 out of the 7 deaths were associated with underlying diseases, which suggested that patients with chronic diseases or cancers were more likely develop critical illness. In addition, 6 out of the 7 deaths in this study occurred in the spring of 2016. Given the cyclical nature of influenza epidemics, six years after 2009 H1N1 pandemic, H1N1 flu activity peaked once again in Shenzhen, causing recorded fatalities. The number of deaths reported in current study is consistent with the number from 2009. Currently, the exact timing and area of flu epidemics are not predictable. Therefore, better understanding of the cyclical trends of the flu epidemic has become very important for disease prediction.
Conclusion
In Shenzhen, the high incidence of influenza is identified in the spring. After the global pandemic of influenza A H1N1, the flu remains an important cause of childhood hospitalization and death. The main causes of death in children are influenza-associated acute necrotizing encephalopathy and secondary severe bacterial infection.
Acknowledgement
This work was supported by Sanming Project of Medicine in Shenzhen (SZSM201512030),Key Medical Disciplines Building Project of Shenzhen (SZXJ2017005), and Shenzhen public service platform for clinical drug trials (20151964).
More BJSTR Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.