The Use of Immunomicelles to Treat Ovarian Cancer
Introduction
The use of nannocarriers in general for the delivery of cytotoxic agents to solid tumors is ideal as they have been shown to improve the overall pharmacological properties of otherwise low-molecular weight “free drugs”, or unencapsulated cytotoxic agents by altering drug pharmacokinetics and biodistribution/bioavailability [1]. There are numerous types of nanocarriers available for such delivery to include dendrimers, liposomes, nanoparticles made of various materials (i.e. ceramic nanoparticles), as well as micelles to name a few. While all of these nanocarriers have been used with varying levels of success in the past, micelles are particularly attractive for use as a drug delivery system for a number of reasons. For example, micelles used for this purpose are by definition selfaggregates of biocompatible surfactant molecules dispersed in a liquid colloid containing a hydrophobic core (Figure 1, upper left). Thus, they are ideal for the encapsulation of hydrophobic drugs, which most chemotherapeutics tend to be, thereby eliminating the need for potentially toxic solubilizing agents such as Cremophor EL during intravenous (i.v.) administration [2].
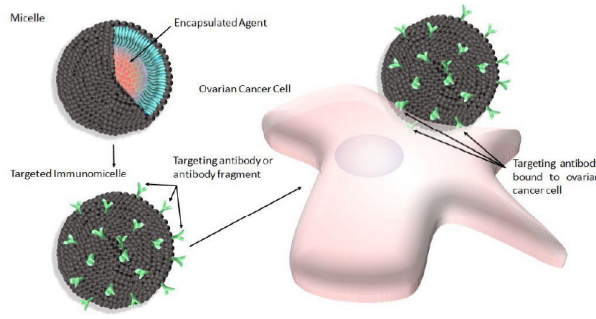
Figure 1: Shematic depicting micelles (upper left) modified with antibody or antibody fragments to produce targeted immunomicelles (lower left) intended to target and bind specific overexpressed cell surface receptors present on ovarian cancer cells (right).
Furthermore, the clinical success of drugs such as GenexolPM, which is produced by the Samyang Company in South Korea and is clinically approved in that country [3,4], proves that these nanocarriers can in fact be very effective in the treatment of solid tumors. This micellar-based drug formulation contains the hydrophobic mitotic inhibitor cytotoxic agent paclitaxel. It should be noted however, that clinically-approved micellar-based drugs such as Genexol-PM delivers encapsulated cytotoxic agents to solid tumors based on a “passive” form of delivery facilitated by the enhanced permeability and retention (EPR) effect [5,6], and future work intended to improve the overall efficacy of micellar-based drugs involve “active” delivery of encapsulated drugs. Generally, this latter type of delivery involves the addition of a targeting ligand to the drug formulation that is specific to certain identified upregulated cell surface receptors known to be present on various cancer cells in order to improve drug/cancer cell colocalization.
An additional distinct advantage of using nanocarriers such as micelles for this type of delivery is the ease with which they can be surface-modified to accommodate such targeting ligands, thereby eliminating the need for direct conjugation between the targeting ligand and the drug, which can potentially negatively alter the cytotoxicity of the drug [7,8]. Various targeting ligands have been used in order to confer targeting capabilities to micelles, and have recently been reported with varying levels of success. For example, small molecules including vitamins, carbohydrates, peptides and proteins have all been used to generate targeted micelles intended to treat various types of cancers [9-12]. However, due to the fact that specificity between the targeting ligand and intended upregulated cell surface receptor is a very important consideration when selecting a targeting ligand, many groups have elected to use antibodies or antibody fragments to generate immunomicelles (Figure 1, lower left). Furthermore, ovarian cancer in particular has specifically been the focus of many recent studies involving immunomicelles as the clinically approved micellar-based drug Genexol-PM contains encapsulated paclitaxel [13], which is known to be a standard chemotherapeutic front-line agent for the treatment of ovarian cancer [14,15]. Furthermore, paclitaxel, along with other drugs such as the antineoplastic drug doxorubicin which is also a front-line agent used in the treatment of ovarian cancer [16], are drugs that are very commonly-used in micellar based formulations. Additionally, as previously mentioned, ovarian cancer is the most common cause of gynecological cancerrelated death and one of the leading overall causes of cancerassociated mortalities amongst women worldwide [17,18], and therefore much more efficacious drugs are desperately needed with respect to this type of cancer. These future drugs may in fact involve immunomicelles, and while we recognize that it is not possible to present every immunomicellar-based drug preparation intended for the treatment of ovarian cancer considering this large and rapidly growing field, rather here we present some of the more recently reported promising formulations.
Immunomicelles Intended to Target Ovarian Cancer
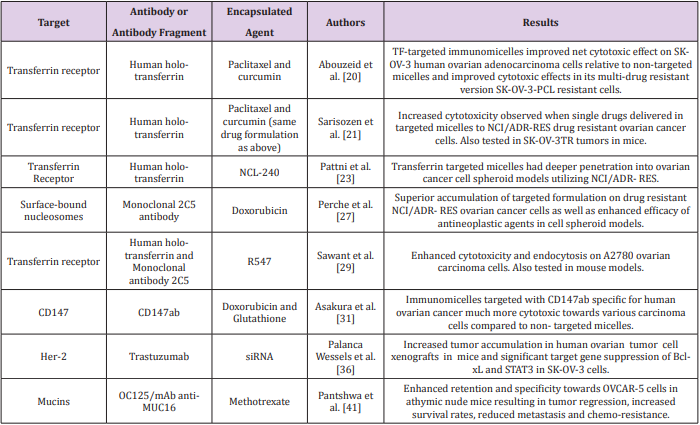
In general, antibodies would seem to be ideal targeting ligands due to their highly specific nature. However, there are several complications associated with the use of full antibodies as targeting ligands in drug formulations to include immunogenicity resulting in rapid elimination and low circulation times in vivo [19]. Therefore in some cases, antibody fragments are used instead of full antibodies in order to generate a less immunogenic drug formulation. In any event, the advantage of using antibodies or antibody fragments as targeting ligands to generate immunomicelles specific for ovarian cancer (Figure 1, right) can clearly be seen in the literature, and many recent reports seem to be very promising (Table 1). For example, Abouzeid et al. [20,21] have recently reported a drug formulation involving holo-transferrin-immunomicelles containing encapsulated paclitaxel and curcumin, which are specific for the overexpressed transferrin receptor [20].
In this study, immunomicelles decorated with CD147ab proved to be much more cytotoxic towards various carcinoma cell lines compared to non-targeted micelles. Human epidermal growth factor receptor 2 (HER2) is yet another known potential target for targeted chemotherapeutics due to its overexpression in various types of cancers, resulting in increased tumor aggressiveness and a relatively poor prognosis [33,34]. However, the frequency of positive HER2 overexpression in ovarian cancer is quite variable [35], and therefore it is unclear as to how widely used HER2 targeted drugs would be amongst ovarian cancer patients in particular. Nonetheless, such a drug formulation would potentially be of great benefit to ovarian cancer patients with positive HER2 overexpression. In fact, Palanca Wessels et al. [36] have recently reported immunomicelles decorated with trastuzumab, which is a targeting ligand specific for HER2, containing encapsulated short interfering RNA (siRNA) [36].
Increased tumor accumulation in human ovarian tumor cell xenographs in mice and significant target gene suppression of Bcl-xL and STAT3 in SK-OV-3 ovarian cancer cells was observed when the targeted formulation was used compared to its nontargeted counterpart. These two genes in particular were chosen in this study as Bcl-xL gene expression allows cancer cells to escape apoptotic signals resulting from treatment, and STAT3 mediates the expression of various genes involved in cellular survival function [37,38]. Interestingly, STAT3 can be activated by MUC16, which is a transmembrane glycoprotein mucin that has been shown to be overexpressed in ovarian cancer, and therefore it is also a potential target in targeted drug delivery [39,40]. In fact, Pantshwa et al. [41] have recently reported a drug formulation involving mAb antiMUC16 immunomicelles containing encapsulated methotrexate to treat ovarian cancer cells [41]. In this study, the targeted formulation resulted in tumor regression, increased survival rates, reduced metastasis, and reduced chemoresistance compared to the non-targeted system when tested in mice.
Conclusion
While there are many types of targeting ligands that can in theory be used along with micellar-based drugs, antibodies or antibody fragments are particularly attractive due in part to their specificity for the various known upregulated/overexpressed cell surface receptors present on ovarian cancer cells. This combination of using micelles decorated with antibodies or antibody fragments to form immunomicelles, designed to treat ovarian cancer specifically in this case, have been shown to be quite promising and many recently reported drug formulations have been described here. While it is not possible to describe every immunomicellarbased drug formulation intended for the treatment of ovarian cancer, rather here we report some promising drug formulations involving immunomicelles based in part on the encouraging results recently reported in the literature.
Acknowledgement
This work was supported by funds generously provided by the Welch Foundation (grant # AE-0025), the Ross Wilson Organization, as well as the Killgore Research Center through the Research Enhancement and Killgore Research grant program at West Texas A&M University.
More BJSTR Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.