25-OH Vitamin D Levels in Patients with Pituitary Adenoma
Introduction
Pituitary adenomas are most common in the 3rd decade and constitute 10 percent of all intracranial neoplasms [1-3]. Pituitary adenomas are classified according to the size and function of the cell in which they originate [4]. Functional pituitary adenomas may be disorders affecting bone metabolism. This condition has been described in cushing’s disease. Vitamin D has an important clinical role due to its relationship with calcium balance and bone metabolism. This degree of vitamin D deficiency may contribute to the development of osteoporosis and the risk of fracture and fall [5]. The aim of this study was to evaluate vitamin D levels in pituitary adenomas.
Materials and Methods
The study included 88 patients (60 females, 28 males) who were followed for pituitary adenoma between the years of 20016- 2018. Patients’ physical examination, pituitary MR results, FSH, LH, estradiol, Testosterone, ACTH, cortisol, Growth hormone, Igf-1, prolactin and 25-OH vitamin D levels results were recorded. 1 mg dexamethasone test was performed in appropriate patients.
Results
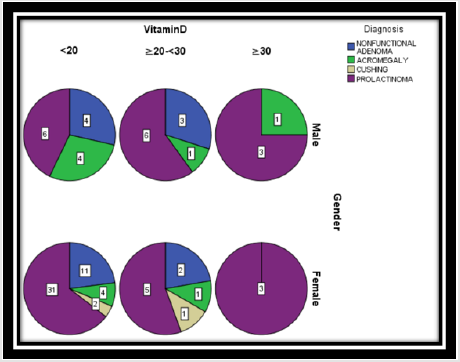
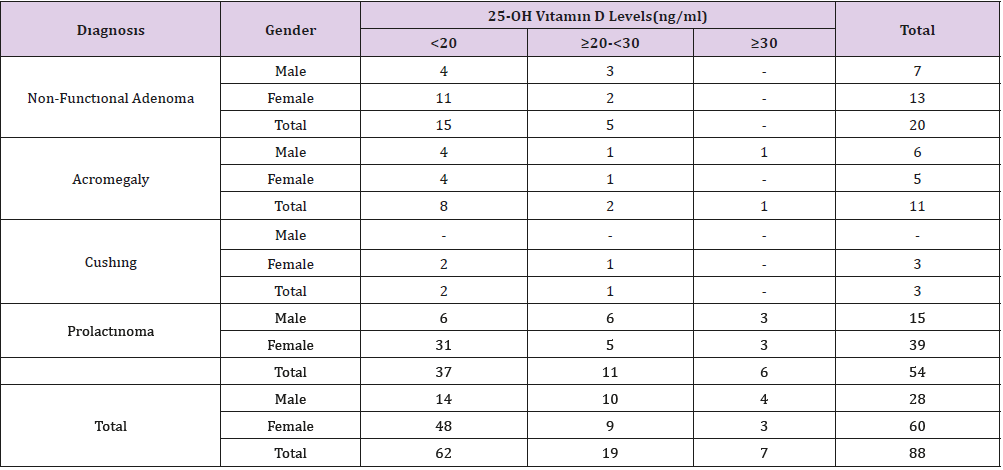
Of the 88 patients with pituitary adenoma, 62 (70.4%) had vitamin D deficiency, and 19 (21.6%) had vitamin D insufficiency. Only 7 patients (8%) had vitamin D levels above 30 ng / dl and were adequate. The mean age of the patients with non-functional adenoma was 41.7 years (min: 18-max: 68); 7 (33.3%) were males and 13 (61.9%) were females. In 15 patients, vit D was < 20, while 6 patients had vit D value of ≥20-<30. The mean age of patients with acromegaly was 46.1 years (min: 33-max: 64); 6 (54.5%) were males and 5 (45.5%) were females. In 8 patients, vit D was <20, while 2 patients had vit D value of ≥20-<30. The mean age of the 3 female patients with Cushing disease was 33.3 years (min: 18-max: 48). In 2 patients, vit D was <20, while 1 patient had vit D value of ≥20-<30. The mean age of patients with prolactinoma was 32.3 years (min: 19-max: 60); 15 (33.3%) were males and 39 (61.9%) were females. In 37 patients, vit D was <20, while 11 patients had vit D value of ≥20-<30. Only 25 of the 88 patients had 25 OH vitamin D levels above 30 ng / dl. One of them was acromegaly, the other six patients with prolactinoma (Figure 1).
Discussion
Vitamin D is a secosteroid hormone. Serum 25 hydroxy (OH) vitamin D levels are measured, and their adequacy is evaluated. (> 30 ng/ml: adequate, 20-30 ng/ml: insufficiency, <20 ng/ml: deficiency, <10 ng/ml: severe deficiency) [6]. Vitamin D deficiency is associated with osteoporosis, possibly fractures and risk of falling [6,7]. Osteoblasts have prolactin (PRL) receptors. Prolactin has an adverse effect on bone metabolism by inhibiting osteoblast proliferation and increasing osteolytic activity. Prolactin also causes an increase in RANKL and osteoprotogerin. As a result, bone loss is observed. In women with prolactinoma, approximately 25% of the vertebrae are lost due to hypogonadism. Treatment with bone density increases but may not return to the old level. In men with prolactinoma, osteopenia / osteoporosis occurs due to low testosterone levels [8-12] (Table 1).
The pathogenesis of osteoporosis in patients with Cushing’s disease, decreased osteoblast function, decreased calcium absorption from the bowel, calcium excretion from kidneys decreased gonadal steroid synthesis, decreased muscle mass and strength, growth hormone secretion and decreased effectIn cushing’s disease, osteoporosis was found in 50% of the patients. Even in these patients, non-traumatic fractures or osteoporosis incompatible with age are detected [13-16]. In acromegalic patients, growth hormone stimulates the carboxylation of osteocalcin on the one hand and stimulates the production of RANKL and osteoprotoger. Growth hormone and IGF-1 stimulate the 1-alpha hydroxylase enzyme in the kidney to increase the synthesis of 1,25 dihydroxycholecalciferol. Even if osteoporosis does not increase in acromegalic patients, the risk of bone fracture has increased [17- 20]. Vitamin D deficiency and / or insufficiency were found in all patients in this study. In addition to existing pathophysiological conditions, we think that vitamin D deficiency increases the risk of osteoporosis and / or bone fracture in these patients.
Conclusion
Vitamin D deficiency should be considered and treated in these patients with high risk of osteoporosis or high risk of bone fractures when treating these patients.
For more Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.