Colonic Diverticular Bleeding: A Case Report and Review of the Literature
Introduction
In Japan, colonic diverticular bleeding has been increasing due to the prevalence of colonic diverticula has increased [1,2]. However, it is uncommon to treat patients with colonic diverticular bleeding in China. Colonic diverticular bleeding is an acute illness, they often recur and necessitate colectomy when endoscopic treatment failed, which makes this disease of great importance in clinical settings. The management of diverticular bleeding differs between China and Western countries. Computed tomography (CT) tends to be the first option at Chinese hospitals, so urgent CT may be selected as the first diagnostic procedure for suspected diverticular infection or bleeding. Novel treatment methods such as endoscopic clipping or band ligation have been introduced as hemostatic techniques for colonic diverticular bleeding [3,4]. Therefore, endoscopic clipping or band ligation may be preferred as the first endoscopic procedure for diverticular bleeding in western countries. Here, we report a case of colonic diverticular bleeding caused by diverticular infection in a 56-year-old male who finally underwent endoscopic treatment after administration of antibiotics could not relieve his symptoms.
Case Presentation
A 56-year-old man, presented with pain in his right side along with hematochezia seven times in half day, he was admitted at Emergency Department. The result of vital signs was normal. The physical examination showed tenderness and rebound tenderness in the right abdomen. Digital rectal examination (DRE) result was positive. Blood test revealed white blood cell (WBC): 6.53*10^9/L, percentage of neutrophils: 54.2%, Hemoglobin (HB): 145g/L, platelet (PLT): 303*10^9/L. An urgent abdominal CT scan revealed multiple diverticulum with suspicious infection were found at the ileocecal junction. Patient reported the medical history of hemorrhoids, atrial fibrillation, colon polyps and diverticulum. He denied the history of hypertension, diabetes and HIV infection. The first day of hospitalization, blood test showed white blood cell (WBC): 6.46*10^9/L, neutrophils: 60.6%, Hemoglobin (HB): 159g/L, platelet (PLT): 311*10^9/L, hematocrit (HCT): 46.9%. The result of fecal occult blood test (FOBT) was positive.
Doctor prescribed fasting and given intravenous nutrition support. Meanwhile, use proton pump inhibitors (PPIs) and antibiotics as part of the treatment. Gradually, the symptom of abdominal pain relieved and no hematochezia existed. On the second day of hospitalization, the condition of this patient was stable, better than the first day and no hematochezia. He began to fluid diet and continued to the previous therapy. However, on the third day at hospital, massive hematochezia occurred again together with right lower abdominal tenderness. The emergency colonoscopy showed bright red blood and multiple diverticula in the ileocecal junction. After profuse water irrigation, active arterial bleeding from a diverticulum was identified near the vermiform appendix. The bleeding was treated by a combination of adrenaline injection followed by hemostatic clips. Hemostasis was rapidly achieved and no rebleeding or hematochezia had occurred. The patient recovered well and was discharged 5 days after the surgery. No discomfort has been reported by a 30-day follow-up visit (Figure 1).
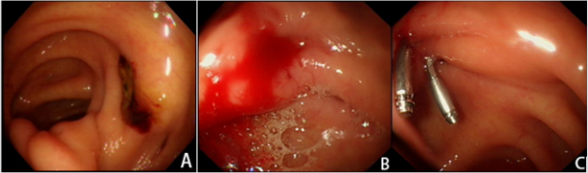
Figure 1: Endoscopic images of the patient.
(A) SRH of a diverticulum was observed under colonoscopy, which can be used as a diagnostic marker of definitive colonic diverticular bleeding.
(B) After profuse water irrigation, active arterial bleeding from a diverticulum was identified near the vermiform appendix.
(C) Endoscopic clipping was conducted as endoscopic treatment for diverticular bleeding, the image showed cessation of active bleeding.
Abbreviations: SRH: Stigmata of Recent Hemorrhage.
Discussion
Typically, gastrointestinal bleeding (GIB) was divided into two categories: upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB) [5]. LGIB is less common than UGIB, with an annual incidence of hospitalization of approximately 36/100,000 population. While approximately 67/100,000 population for the UGIB [6,7]. Due to the aging of the population and with the application of antithrombotic agents, acute LGIB is becoming more common in the elderly men than elderly women [5,8], with mortality rates of 2.5%-3.9% during hospitalization [9,10] and rebleeding rates of 13%-19% after 1 year [11,12]. Hospitalization rate of diverticulum hemorrhage and diverticulitis in Japan has been increased in recent years [1,2]. Some serious complications, including bleeding, perforation and acute abdominal pain, are life-threatening. However, diverticular bleeding is a rare condition. For the diagnosis of acute LGIB patients caused by colonic diverticulosis, abdominal CT and colonoscopy are preferred. Several studies have focused on the association between extravasation on CT and definitive diverticular bleeding on colonoscopy [13,14]. The detection rate of diverticular bleeding is significantly higher in patients with extravasation on CT than in those without (60%- 76% vs 18%-31%) [14,15], which means extravasation on CT is a useful test for colonoscopy to detect SRH. However, prospective studies of diverticular bleeding demonstrated that the positive rate of extravasation is low (15%-25%).
Therefore, not all cases are suitable for CT [14,16]. Furthermore, Colonoscopy is the initial procedure for most patients presenting with acute LGIB, not only for its diagnostic but also therapeutic utility [17]. Before the operation of colonoscopy, bowel preparation is a critical factor to identify the source of bleeding and make an accurate diagnosis. However, when is the optimal time to conduct colonoscopy remains controversial. Early colonoscopy in most studies was within 24h of hospitalization, and the concept in some prospective trials was within 6-12h [18,19]. Early colonoscopy had more possibilities of improving identification of the bleeding source, and the rate of endoscopic intervention. Under colonoscopy, discover stigmata of recent hemorrhage (SRH), including active bleeding, a non-bleeding visible vessel, and an adherent clot, is one of meaningful findings in the diagnosis of acute LGIB [20,21]. Except for early colonoscopy and adequate colon preparation, previous studies have demonstrated that an expert endoscopist, using a cap or a water-jet scope can help to improve the detection rate of SRH [22]. For the treatment of acute LGIB patients caused by colonic diverticulosis. In the initial clinical evaluation, evaluate vital signs such as state of consciousness, blood pressure, and heart rate and stabilize hemodynamics are of great importance.
At the same time, evaluating accompanying symptoms, comorbidities, medical history, and blood tests[23]. Endoscopic hemostasis is the first-line treatment for colonic diverticular bleeding. Due to recent advances in endoscopy and improved outcomes in arterial embolization, colectomy is no longer the first line of treatment for colonic hemorrhage [23,24]. Unfortunately, if endoscopic treatment failed or severe colonic hemorrhage reoccurred after arterial embolization, colectomy is highly recommended. If the bleeding site is recognized before surgery, a partial colectomy is an optimal surgical plan; otherwise, a subtotal colectomy is needed. In addition to that, barium impaction therapy for diverticular bleeding has been reported. However, although the evidence is stem from case report or case series, barium impaction therapy could be potential treatment for patients with uncontrolled or recurrent presumptive diverticular bleeding [25]. The effectiveness of barium impaction therapy for long-term prevention of rebleeding has been demonstrated in RCT. The hazard ratio (HR) of rebleeding in the barium group was 0.34 (95% CI: 0.12-0.98), compared with conservative treatment after spontaneous cessation of diverticulum hemorrhage [26].
Introduction
In Japan, colonic diverticular bleeding has been increasing due to the prevalence of colonic diverticula has increased [1,2]. However, it is uncommon to treat patients with colonic diverticular bleeding in China. Colonic diverticular bleeding is an acute illness, they often recur and necessitate colectomy when endoscopic treatment failed, which makes this disease of great importance in clinical settings. The management of diverticular bleeding differs between China and Western countries. Computed tomography (CT) tends to be the first option at Chinese hospitals, so urgent CT may be selected as the first diagnostic procedure for suspected diverticular infection or bleeding. Novel treatment methods such as endoscopic clipping or band ligation have been introduced as hemostatic techniques for colonic diverticular bleeding [3,4]. Therefore, endoscopic clipping or band ligation may be preferred as the first endoscopic procedure for diverticular bleeding in western countries. Here, we report a case of colonic diverticular bleeding caused by diverticular infection in a 56-year-old male who finally underwent endoscopic treatment after administration of antibiotics could not relieve his symptoms.
Case Presentation
A 56-year-old man, presented with pain in his right side along with hematochezia seven times in half day, he was admitted at Emergency Department. The result of vital signs was normal. The physical examination showed tenderness and rebound tenderness in the right abdomen. Digital rectal examination (DRE) result was positive. Blood test revealed white blood cell (WBC): 6.53*10^9/L, percentage of neutrophils: 54.2%, Hemoglobin (HB): 145g/L, platelet (PLT): 303*10^9/L. An urgent abdominal CT scan revealed multiple diverticulum with suspicious infection were found at the ileocecal junction. Patient reported the medical history of hemorrhoids, atrial fibrillation, colon polyps and diverticulum. He denied the history of hypertension, diabetes and HIV infection. The first day of hospitalization, blood test showed white blood cell (WBC): 6.46*10^9/L, neutrophils: 60.6%, Hemoglobin (HB): 159g/L, platelet (PLT): 311*10^9/L, hematocrit (HCT): 46.9%. The result of fecal occult blood test (FOBT) was positive.
Doctor prescribed fasting and given intravenous nutrition support. Meanwhile, use proton pump inhibitors (PPIs) and antibiotics as part of the treatment. Gradually, the symptom of abdominal pain relieved and no hematochezia existed. On the second day of hospitalization, the condition of this patient was stable, better than the first day and no hematochezia. He began to fluid diet and continued to the previous therapy. However, on the third day at hospital, massive hematochezia occurred again together with right lower abdominal tenderness. The emergency colonoscopy showed bright red blood and multiple diverticula in the ileocecal junction. After profuse water irrigation, active arterial bleeding from a diverticulum was identified near the vermiform appendix. The bleeding was treated by a combination of adrenaline injection followed by hemostatic clips. Hemostasis was rapidly achieved and no rebleeding or hematochezia had occurred. The patient recovered well and was discharged 5 days after the surgery. No discomfort has been reported by a 30-day follow-up visit (Figure 1).
Figure 1: Endoscopic images of the patient.
(A) SRH of a diverticulum was observed under colonoscopy, which can be used as a diagnostic marker of definitive colonic diverticular bleeding.
(B) After profuse water irrigation, active arterial bleeding from a diverticulum was identified near the vermiform appendix.
(C) Endoscopic clipping was conducted as endoscopic treatment for diverticular bleeding, the image showed cessation of active bleeding.
Abbreviations: SRH: Stigmata of Recent Hemorrhage.
Discussion
Typically, gastrointestinal bleeding (GIB) was divided into two categories: upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB) [5]. LGIB is less common than UGIB, with an annual incidence of hospitalization of approximately 36/100,000 population. While approximately 67/100,000 population for the UGIB [6,7]. Due to the aging of the population and with the application of antithrombotic agents, acute LGIB is becoming more common in the elderly men than elderly women [5,8], with mortality rates of 2.5%-3.9% during hospitalization [9,10] and rebleeding rates of 13%-19% after 1 year [11,12]. Hospitalization rate of diverticulum hemorrhage and diverticulitis in Japan has been increased in recent years [1,2]. Some serious complications, including bleeding, perforation and acute abdominal pain, are life-threatening. However, diverticular bleeding is a rare condition. For the diagnosis of acute LGIB patients caused by colonic diverticulosis, abdominal CT and colonoscopy are preferred. Several studies have focused on the association between extravasation on CT and definitive diverticular bleeding on colonoscopy [13,14]. The detection rate of diverticular bleeding is significantly higher in patients with extravasation on CT than in those without (60%- 76% vs 18%-31%) [14,15], which means extravasation on CT is a useful test for colonoscopy to detect SRH. However, prospective studies of diverticular bleeding demonstrated that the positive rate of extravasation is low (15%-25%).
Therefore, not all cases are suitable for CT [14,16]. Furthermore, Colonoscopy is the initial procedure for most patients presenting with acute LGIB, not only for its diagnostic but also therapeutic utility [17]. Before the operation of colonoscopy, bowel preparation is a critical factor to identify the source of bleeding and make an accurate diagnosis. However, when is the optimal time to conduct colonoscopy remains controversial. Early colonoscopy in most studies was within 24h of hospitalization, and the concept in some prospective trials was within 6-12h [18,19]. Early colonoscopy had more possibilities of improving identification of the bleeding source, and the rate of endoscopic intervention. Under colonoscopy, discover stigmata of recent hemorrhage (SRH), including active bleeding, a non-bleeding visible vessel, and an adherent clot, is one of meaningful findings in the diagnosis of acute LGIB [20,21]. Except for early colonoscopy and adequate colon preparation, previous studies have demonstrated that an expert endoscopist, using a cap or a water-jet scope can help to improve the detection rate of SRH [22]. For the treatment of acute LGIB patients caused by colonic diverticulosis. In the initial clinical evaluation, evaluate vital signs such as state of consciousness, blood pressure, and heart rate and stabilize hemodynamics are of great importance.
At the same time, evaluating accompanying symptoms, comorbidities, medical history, and blood tests[23]. Endoscopic hemostasis is the first-line treatment for colonic diverticular bleeding. Due to recent advances in endoscopy and improved outcomes in arterial embolization, colectomy is no longer the first line of treatment for colonic hemorrhage [23,24]. Unfortunately, if endoscopic treatment failed or severe colonic hemorrhage reoccurred after arterial embolization, colectomy is highly recommended. If the bleeding site is recognized before surgery, a partial colectomy is an optimal surgical plan; otherwise, a subtotal colectomy is needed. In addition to that, barium impaction therapy for diverticular bleeding has been reported. However, although the evidence is stem from case report or case series, barium impaction therapy could be potential treatment for patients with uncontrolled or recurrent presumptive diverticular bleeding [25]. The effectiveness of barium impaction therapy for long-term prevention of rebleeding has been demonstrated in RCT. The hazard ratio (HR) of rebleeding in the barium group was 0.34 (95% CI: 0.12-0.98), compared with conservative treatment after spontaneous cessation of diverticulum hemorrhage [26].
For more Articles on : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.