The Assessment of Short IVF Protocols: Clinical Status and Success Rates Among Women Treated in IVF Center in Prince Rashid Hospital, Jordan
Introduction
The main objective of conventional ovarian stimulation protocols regarding in vitro fertilization (IVF) is to obtain highest oocyte yields (Practice Committee of American Society for Reproductive Medicine, 2008). There are side effects associated with conventional protocols such as patient anxiety, ovarian hyperstimulation syndrome increased risk, and high financial expenses [1-3]. The idea of using mild stimulation protocols has recently been introduced and received acceptance [4]. In these protocols, low doses of exogenous gonadotrophins (<150 IU/day) are used. The objective of these protocols is to minimize the retrieved oocytes to be less than eight. It has been reported that pregnancy rate is lower in short protocols compared with long protocols [5]. During the past years, the standard hormonal treatment was based on the agonists of gonadotropin-releasing hormone (GnRH) agonists accompanied by stimulation of ovary using exogenous gonadotropins. This approach was implemented for treatment of women in need for assisted reproductive technologies (ART) [6]. There have been improvements in the outcome of pregnancy as a result of using GnRH agonist in cases of controlled ovarian hyperstimulation (COH) protocols. There is a lowered cycle cancellation by elimination of spontaneous LH surges as well as reduction of poor follicular development [7]. There are protocols for superovulation that can be categorized into three groups: ultra-short, the short and the long protocols [8]. The stimulation of follicles and their growth takes place through giving exogenous FSH. In short protocol, the initial stimulatory phase of GnRHa isused to improve the induction of follicles and keep a hyposecretion of endogenous gonadotropins to be involved in the follicular phase. Exogenous FSH is given to stimulate follicular growth [9].
Study Objectives
The main objectives of the present study were to assess the influence of follicle stimulating hormone (FSH) and Luteinizing Hormone (LH) in the number of oocytes and the number of embryos; and to investigate a possible relationship of these hormones with rates of IVF success.
Methods and Subjects:
Study Design: A retrospective design was conducted to collect data from files of female patients under treatment with IVF-short protocols.
Study Sample: A total of 50 files of women who underwent for this treatment were included in this study. Files with complete information were analyzed.
Study Variables: Study variables included demographic variables including age, hormone levels of FSH, and LH, the number of oocytes, and embryos, and the result of IVF.
Statistical Analysis: An excel sheet was used to enter the data for all included files. The data was further analyzed using SPSS version 21. Data was presented as means and standard deviations. One Way Anova was used to investigate the effect of age on study variables, and to investigate the effects of study variables on pregnancy result. Pearson correlation was used to compute the correlation between study variables. The significance was considered at p≤0.05.
Results
General Characteristics of Study Participants
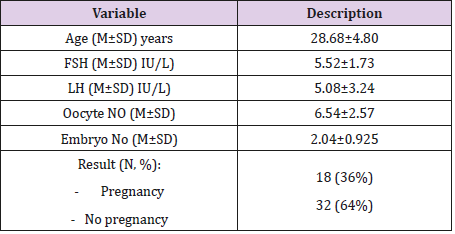
As demonstrated in Table 1, the mean age of women in this study is 28.68±4.80 years. The average of FSH is 5.52±1.73 IU/L, and the average of LH is 5.08±3.24 IU/L. the results also indicated that the average of Oocyte No is 6.54±2.57, while the average of embryo No is 2.04±0.925. The pregnancy success rate is 36%.
The Impact of Age on Study Variables
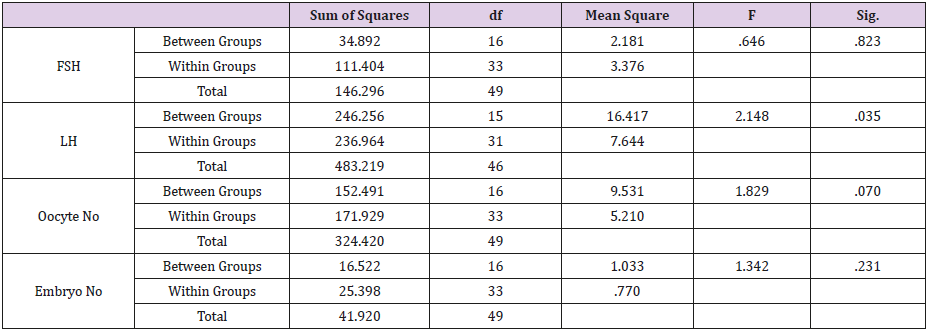
The impact of age on study variable was investigated using One Way Anova test. As shown in Table 2, the level of LH was only significantly associated with age (p=0.035). The other variables were not impacted significantly by age (P>0.05).
The impact of Study Variables on Pregnancy Result
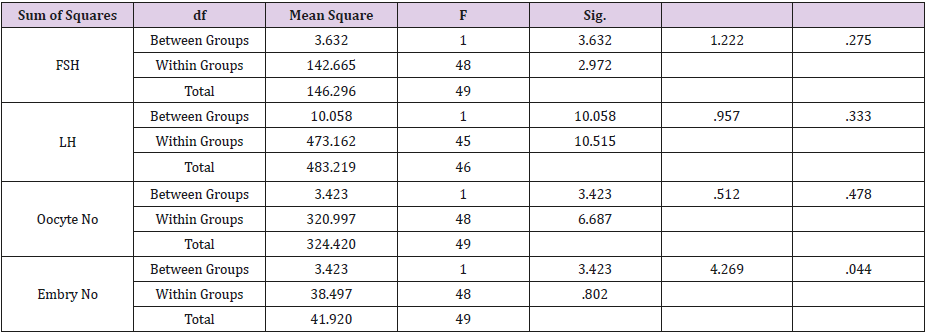
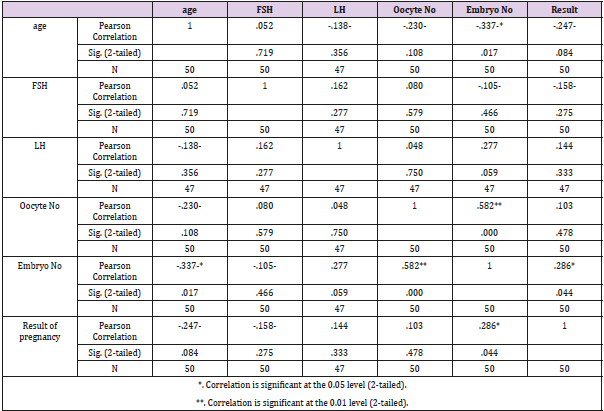
As shown in Table 3, the impact of study variables on pregnancy results was investigated through One Way Anova test. The only variable that was statistically significant on the pregnancy result was the Embryo No (p=0.044). The other variables were not statistically significantly associated with pregnancy result (p>0.05). Correlation between study variables. As shown in Table 4, the correlation between study variables was computed using Pearson correlation. Age was negatively and significantly associated with embryo No (r=-0.337, p=0.017). Another positively and significantly correlation was computed between Oocyte No and embryo No (r=0.582, p=0.000). Finally, a positively and significantly correlation was found between the result of pregnancy and embryo No (r=0.286, p=0.044).
Discussion
We conducted this study to assess the influence of follicle stimulating hormone (FSH) and Luteinizing Hormone (LH) in the number of oocytes and the number of embryos; and to investigate a possible relationship of these hormones with rates of IVF success. In this study, short protocols for IVF were followed. The results of this study showed that the success rate was 36%. The number of oocytes was about 7. These findings are in line with previous studies [10-13] that reported the oocyte number to be less than 8 and also indicated less pregnancy rates compared with conventional methods. The results of the present study showed that age was significantly associated LH (p=0.035). The other variables were not significantly with age (p>0.05). This finding agrees with other studies in which age >35 years may benefit from short protocols, but as patients become older, poor outcomes are expected [14- 16]. The study findings showed that the number of embryos was significantly associated with pregnancy outcome. These findings are plausible and imply that increased number of embryos may lead to success rates of pregnancy; this is in agreement with previous studies [16,17].
Correlation analysis showed that age was negatively and significantly correlated with the number of embryos (r=-0.337, p=0.017). With increased age, the chance for IVF success becomes less. This is in agreement with other studies [18]. A positive and significantly correlation was found between oocyte number and embryo number (r=0.582, p=0.000). This finding implies that the number of oocyte (6.54±2.57) was a significant factor for embryo increased number and as a consequent increased success rate of pregnancy. This is in line with some previous studies [19,20]. A positive and significantly correlation was found between pregnancy results and embryo number (r=0.286, p=0.044). As the number of embryo increases, it is more likely for the pregnancy to take place. This result is logic and in agreement with other studies [21].
Conclusion
The present study showed the success pregnancy rate was 36% following short IVF protocol. Success rate depended on the number of embryos.
For more Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.