Compromised Health and Constrained Human Life in COVID-19 Pandemic, and Concurrent Healthcare Transformation
The SARS-CoV-2 Infection and COVID-19 Pandemic
The current ongoing pandemic of COVID-19 caused by SARSCoV-
2, is associated with high morbidity and mortality in several
countries across the globe. A prompt and effective detection of the
disease is crucial to identify those infected, to monitor the infection
from epidemiological perspective, and to take measures for its
containment. On the other hand, the early diagnosis and efficient
treatment of COVID-19 including newer therapeutic modalities
such as monoclonal antibodies against SARS-CoV-2, may contribute
to the individual clinical improvement and limit the morbidity and
mortality in the society at large. The likely course of COVID-19
pandemic not certain, and the pandemic being considered a major
health hazard, may continue in the foreseeable future or may
with low or moderate level of transmission become endemic. The
COVID-19 vaccines bear hope to bring COVID-19 pandemic under
control, paving a way for its endemicity [1]. In this respect, the
WHO in a recent communique indicated that COVID-19 in various
countries including India may be entering some kind of stage of
endemicity with low or moderate level of transmission [2].
The effects and fallouts of COVID-19 pandemic are striking as it
has impacted the social, economic, political, and healthcare aspects
of human life. The pandemic is being considered a major health
hazard that may continue to afflict human life in the foreseeable
future. The transformation of life, thus, at the individual level as
well as at the community and collective levels, seems inevitable.
Another aspect of the COVID-19 pandemic is the unprecedented
levels of misinformation, rumours, and conspiracy theories related
to COVID-19 relayed and reproduced by lay and social media,
dubbed ‘infodemic’ by the WHO, which are counterproductive to
the fight against the pandemic in the short and long term. There
are concerns about low to middle income countries (LMICs) related
to the COVID-19 preparedness, knowledge sharing, intellectual
property rights, and environmental health together with the
serious constraints regarding readiness of health care systems to
respond to the pandemic. In fact, the spread of COVID-19 presents
an extraordinary ethical dilemma for resource constrained nations
with poorly developed health and research systems.
In the current crisis, sharing of scientific knowledge and
technology has an important role to play. In addition, emergency
preparedness is a shared responsibility of all countries with a moral
obligation to support each other [3]. The ongoing pandemic has led
to a situation in which the scale of emergency is similar to WWII,
requiring decisiveness and commitment. In LMICs, the greatest
challenge is to design strategy for early response to COVID-19
outbreaks. South Asia holds a quarter of the world’s population
with currently COVID-19 affected countries including Afghanistan,
Pakistan, India, Nepal, Bangladesh, and Sri Lanka which may have severe constraints in management of the pandemic. In fact, the
current low number of reported cases from these areas is likely
to be due to less testing with limited resources in these countries.
The resource allocation should be rational, transparent, and based
on scientific evidence as the current COVID-19 crisis presents
challenges that are beyond and above the earlier outbreaks.
Efforts for developing and supplying medical devices, diagnostic
tools, vaccines, therapeutics, and other medical technologies for
COVID-19 pandemic should be tackled judiciously.
Restricted Human Life and Compromised Health
The SARS-CoV-2 Infection control measures are recommended
to prevent exposure as well as reduce transmission of the infection
include the personal preventive measures at individual level
such as mask-wearing, diligent hand washing, particularly after
touching surfaces in public, respiratory hygiene (covering the
cough or sneeze), avoiding touching the face (in particular eyes,
nose, and mouth), cleaning and disinfecting objects and surfaces,
and ensure adequate ventilation of indoor spaces. Apart from the
mask-wearing decreasing exposure to the infection, has also been
hypothesized to reduce the viral load when exposed, and hence to
reduce the risk of severe illness [4]. There are other public health
measures apart from personal preventive measures for infection
transmission reduction focused for source control and containment
of infection and include social/physical distancing, stay-at-home
orders, school, venue, and nonessential business closure, bans on
public gatherings, and travel restrictions with exit and/or entry
screening.
The preventive measures are supplemented with aggressive
case identification and isolation and contact tracing and quarantine.
In the containment areas, the residents are encouraged to stay alert
for symptoms and practice appropriate measures to reduce further
transmission. The widespread testing and quarantine strategies
are imposed to quickly identify secondary infections in an exposed
individual and reduce the risk of exposure to others. There are
strategies involving self-quarantine at home, with maintenance
of at least six feet (two meters) distance from others at all times.
There are variations about preventive and quarantine measures for
vaccinated and unvaccinated individuals, and those with a recent
history of SARS-CoV-2 infection. All these measures restrict human
interactions and social and economic activities. The COVID-19
pandemic has thus imposed multiple restrictions on human life,
with added risks to unprecedented morbidity and mortality,
compromising the global human health, in general [5].
The COVID-19 pandemic has profoundly changed the human
life, caused tremendous human suffering, and challenged the basic
foundations of socioeconomic well-being, beyond the immediate
impacts on health. The short and long-term impacts are likely to be
severe for the disadvantaged groups such as older people, children,
and women in LMICs. The COVID-19 outbreak poses significant
challenges for the elderly, who have high risks for serious
complications which can significantly deteriorate their functioning,
health status, and social connections. The closure of schools and
home confinement during health pandemics has enduring effects
on child and adolescent psychological well-being. In today’s
increasingly urban world, the cities may be better equipped than
the rural areas to respond to the COVID-19 crisis as the latter vastly
lack health care facilities. The COVID-19 will, thus, have a negative
impact on various dimensions of human life and the potential for
deeper effects with GDP and average household income falling by
over 10%, unemployment rising by 5 percentage points and life
expectancy dropping by half a year.
The Evolving Healthcare Options and Innovations
The COVID-19 pandemic has been a reality check for various
provisions of healthcare available in different countries, including
the preventive and therapeutic, outdoor consult as well as indoor
and intensive care. Whereas in China, the totalitarian regime
was able to deal with the pandemic with an iron hand, fully
bifurcate COVID-19 healthcare from that for non-COVID-19, and
ably carry out preventive measures and vaccination program, in
other countries situation has been different. The public health
surveillance programs and available infrastructures were shown
as not consistently optimal. Additionally, the existing healthcare
facilities were unable to cope with the sudden surge and manage
intense pressure on their workload especially in the settings of
acute care. Even with contingency plans well laid out, healthcare
systems were incapable to cope with the abrupt surge in demand
and needed to be transformed. The COVID-19 pandemic, thus, has
acted as a transformation catalyst, accelerating the implementation
and adoption of changes in healthcare. The emerging prototypes
of healthcare delivery appear to put more emphasis on preventive
measures, remote care, and utilization of innovative digital
technologies.
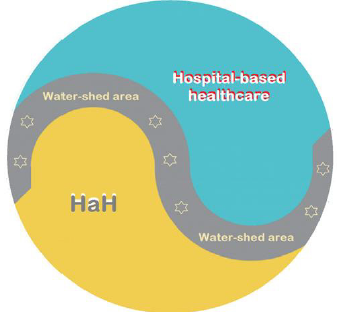
The Hospital-at-Home (HaH) concept was already making
inroads in the conventional hospital-based healthcare approach
for a large number of diseases, with the hospice service being a
surrogate example. In fact, it is being dubbed as the next frontier in
the healthcare delivery and our experience with the pandemic has
fast accelerated the HaH programs. The emerging HaH programs
have advantage of lower costs and readmission rate, while
maintaining quality and safety levels, and better patient experience.
Build on the HaH concepts, the conditions can be identified and
progressively dispensed with home-based primary and secondary
care (Figure 1).
Figure 1: The conventional hospital-based healthcare, the HaH and the water-shed area for intermediate health conditions.
Similar to the scenario in various sectors, the health services
and healthcare too have had profound impact owing to COVID-19
pandemic. The COVID-19 pandemic has brought home the
realization that a significant proportion of healthcare activities can
be tendered remotely equally effectively through technologically
empowered approach. As related to the healthcare, there are
certain salient aspects likely to emerge in the post-COVID-19 era.
1. There is shifting of large number of patients to remote care.
The telehealth services have already been used in emergencies
and during crises in the past. With possibility of quality
transfer of data, audio and video communications during the
COVID-19 pandemic, their utilization has widely accelerated.
The pandemic has become a catalyst for swift implementation
of online consult and therapy, replacing the clinician/patient
face-to-face outdoor consultations.
2. In the hospital setting, the remote care is now being widely
used for screening prior to the visit and triage assessment,
for the indoor and ICU monitoring and supervising of patients
in hospital by off-site experts. This trend is likely to persist to
large extent in the post-COVID-19 period, as it provides higher
convenience both for clinicians as well as patients.
3. In the mental healthcare, too, the remote consultation is
proving helpful. It is likely that once mental healthcare
institutions have developed the capabilities of serving their
patients through digital technologies, a blended approach in
future would emerge, where e-mental-health solutions cover
an increasingly greater part of routine services.
4. The remote care system in form of HaH is likely to serve further
as an adjunct for the gradual adoption of newer and advanced
technologies, such as, the use of drones as delivery vehicles
for critical supplies, robotics, the widespread 3D-printing of
healthcare-related items, and smartphone-enabled monitoring
of patients’ adherence to treatments.
The Healthcare Transformation - Evolution of HaH
As related to the public health, with the availability of the
mobile-enabled technologies, there is an improved operation
of surveillance systems and data analysis. The mobile-enabled
technologies can be deployed en-masse to monitor quarantined
individuals and trace exposed individuals with temporal and
geographical correlates. The new tools are likely to move further
into the public health domain and support the interconnected and
hypercomplex global situations in real-time. On the other hand, the
healthcare, in general, is needed to be people centred and integrated.
The patient centred services include diagnosis and treatment
and other supportive aspects of healthcare, whereas integrated
healthcare involves adequate provision and efficient delivery of
safe and quality health services. The people-oriented approach,
on the other hand, implies planning the healthcare services by
assessing the needs and expectations of community and applying
them in a methodological and efficient way. The integration of
modern technologies including telemedicine in healthcare services
will improve the quality of healthcare.
The COVID-19 pandemic has led to realization about the
limitations of existing healthcare systems and their capacity to
respond to healthcare emergencies including infectious disease
epidemics. It has underlined the inadequate health literacy among
general population to grasp the healthcare recommendations and
their outcomes [6]. It has also served as a reminder for proactive
planning and preparedness. In addition, it has highlighted the necessity for technologically oriented solutions for healthcare
provision and the need for significant healthcare transformation.
On the other hand, it has opened the pathways to evolution and
expansion of the concept of HaH incorporating communication
technology-based approach as a major step to deliver healthcare
at home or closer to home with all necessary steps to safeguard the
safety and privacy of the participants.
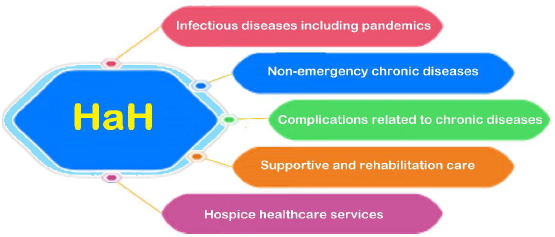
In fact, the healthcare at home (HaH) can be modelled on
lines of the hospice care as a multidisciplinary team approach,
generally home-based and sometimes providing services through
freestanding facilities, in nursing homes, or within hospitals for
handling potentially treatable conditions such as pneumonia, heart
failure, and alike, with brief hospital stays if necessary (Figure 2).
The HaH describes a delivery paradigm where the entirety of the hospital-based inpatient care modality is substituted with intensive at-home treatment approach enabled by digital technologies, multidisciplinary teams, and ancillary services [7]. The potential spectrum of HaH can incorporate the hospice care. But as compared to the latter, apart from providing healthcare services for the terminally ill and elderly in form of hospice care, the HaH can be also useful for all those patients who need intense medical care and treatment but can be managed with help of technological monitoring and remote supervision by healthcare professionals at their homes with possible access to a nearby medical facility or hospital. HaH can make possible for people to receive a variety of medical services in their homes and can satisfactorily deal with various health conditions, as it incorporates therapeutic and nursing care, and medical assistance. In fact, the HaH is being envisaged as an alternate attractive model for accommodating increased demand for inpatient health care and as we prepare for the post-COVID-19 pandemic era, there are evolving salient features of HaH potentially promising to maximize the benefits of transformed health care [8].
The Management and Delivery of Healthcare at Home
During the COVID-19 pandemic, there has been a decline in
emergency department visits and hospital admission rates in
various countries [9]. It seems that in addition to a shift to virtual
healthcare, COVID-19 also influenced emergency department visits
and hospital admissions unrelated to COVID-19 itself. The studies
from both Spain and Italy have shown a reduction in admissions
and procedures related to conditions like myocardial infarction and
acute coronary syndrome [10,11]. A recent study from Thailand
demonstrated that during a national lockdown for COVID-19, there
was a significant reduction in daily emergency department visits
[12]. Similarly, a study from Melbourne, Australia documented
that during times of COVID-19 restrictions there was a significant
reduction in ED visits [13]. According to a survey by Canadian
Home Care Association, there has been a decline of around 72%
in emergency department visits, in turn resulting in the reduction
of hospital admission rates [14]. These reductions in outpatient
service and admissions underline the need to develop an alternative
modality of healthcare for patients still requiring inpatient
management for their acute and chronic medical conditions.
The integration of modern technologies like electronic health
record (EHR) and telemedicine in healthcare services will save time
and resources and provide better healthcare to the users. There
are five major technologies which are likely to reform home-based
healthcare, and include use of various biosensors, GPS, remote
monitoring tools, electronic data and analysis, and telehealth.
The e-Prescriptions generated are easy to be transmitted and
compatible with the EHR.
In general, the HaH comprises of the following benefits:
1. With the primary focus of HaH, people get medical support at
home rather than spending time in a medical facility. Further,
it allows people to stay comfortably at their residential
facility rather than at hospitals, having lower cost and various
psychological advantages.
2. Activities of daily living are not altered and supported in-home
in usual ways while maintaining a good quality of life for them
in the known and perceptive atmosphere.
3. With the home care provided to patients with chronic health
issues such as diabetes and respiratory disease, clinical trials
have shown fewer complications and better health outcomes.
The personalized and skilled care improves the overall
response to the treatment.
4. With the real-time monitoring with technological equipment,
the patients are seen and followed in real-time. Along with the
AI and automation, the HaH aims to streamline the processes
such as scheduling appointment, data collection, maintaining
EHR, e-prescriptions, and scheduling and providing other
health-related services as and when needed to improve the
overall patient care at home.
The Covid-19 pandemic has amplified interest in HaH in the
United States, European countries, and elsewhere as an alternative
care model for both COVID-19 and non-COVID-19 patients, who
can be remotely managed aided by current regulatory flexibilities
(15). In fact, the HaH is being envisaged as an attractive model
for accommodating unprecedented demand for inpatient capacity
created by Covid-19. As we prepare for the health care for the postpandemic
era, there are salient issues to be solved to maximize the
benefits of HaH -
1. The HaH models must encompass the provision of healthcare
of analogous intensity to hospital inpatient standards, and
have a specified geographic catchment area, with properly
defined correlates.
2. As the HaH is supposed to create the acute hospital care at
home and to enable health systems to provide intensive care at
home for patients with various acute and chronic conditions,
this may lead to a remarkable expansion of HaH.
3. There is a unique opportunity to extend and expand HaH in
current times, which can become a new vehicle for integrating
non-medical services into healthcare as the patients may
require further support due to complexity of their illness.
4. With the advances in digital technologies and their increased
utilization by patients and healthcare providers, there is taking
place transformation of the home environment into a preferred
healthcare delivery site.
5. As the health awareness and rising cost of healthcare services
may lead to increase in demand of HaH, managing and
delivering HaH with technological backup should be affordable
and providing quality service.
6. Further, a regulatory and policy implementation roadmap is
required for provision of HaH, which should be accompanied by
monitoring tools, such as, public reporting, patient registries,
and maintenance of reliable database.
Conclusion - The Healthcare Solutions for the
Future
With the COVID-19 pandemic having impact on almost every
aspect of human life, the lessons have been learned relating to
provision of healthcare. The telemedicine and virtual online
consultations have been helpful in dealing with sudden surge and
demand for healthcare both outdoor consult as well as emergency
visits, and indoor and ICU care. During the COVID-19 and now in post-
COVID-19 phase the alterations in provision of healthcare and its
transformation have been enormous. The conventional healthcare
encompassing outdoor consult and hospital-based care is being
increasingly replaced by tele- and video- consultations, remote
technologically assisted indoor care, and HaH. While the hospitalbased
care cannot be fully dispensed with, a large proportion of it
being increasingly assigned to HaH. The technologically assisted
remote healthcare, outdoor as well as indoor, with its availability
and acceptability, and associated challenges and benefits, is the
new reality of current times.
For more Articles on : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.