Electroanatomical Voltage Mapping Endomyocardial Biopsy-Guided Diagnosis and Therapy of Erythroparvovirus Myocarditis Presenting with Ventricular Arrhythmias: Case Series and Review of the Literature
Introduction
Myocarditis is an inflammation of the cardiac muscle caused by infiltration of immunogenic cells following different kinds of cardiac injury. It most commonly results from a viral illness; however, it can also be due to non-infectious etiologies. Given its variable clinical presentation, the diagnosis is frequently missed, making it difficult to quantify the true incidence of acute myocarditis. Infectious causes include a large number of viruses, as well as bacteria, protozoa and fungi; among these pathogens viruses are the most frequent cause of the myocardial inflammatory process. The most common forms of cardiotropic viruses found in endomyocardial biopsies (EMB) are erythroparvovirus B19 (B19V) and human herpes virus 6 (HHV6) and most recently Coronavirus (COVID19) [1-4]. We will now present two cases of 3 Dimensional electroanatomical mapping (3D-EAM) guided endomyocardial biopsy for the diagnosis and therapy of B19V myocarditis presenting with ventricular arrhythmias.
Case 1
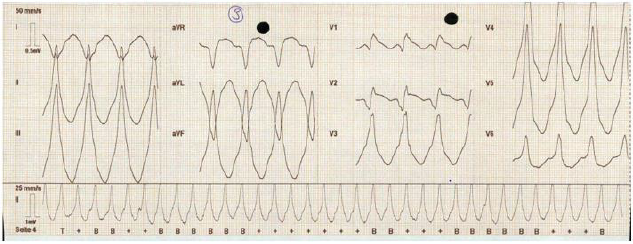
A 54-year-old woman presented to our emergency departement
with a sustained monomorphic ventricular tachycardias
(VTs) (inferior axis, RBBB, Figure 1), which, due to evolving
haemodynamic instability, had to be cardioverted externally. She
had no other known diseases except for a MTHFR mutation without
clinical relevance and did not take any medications. On her arrival
and after the external cardioversion she had no complaints. She
had a normal blood work with no signs of an active infection and
only a slightly elevated Troponin without elevation of CK as well
as CKMB. Her ECG in sinus rhythm showed a minimal diffuse STelevation
and relatively low voltages in the praecordial leads.
The patient underwent a coronary-angiography, with no signs of
coronary disease, an echocardiography which showed a normal
left ventricular function with a slightly enlarged and dyskinetic
right ventricle and finally a cardiac MRI (c-MRI) with evidence
of preserved LV function and a RV dyskinesia as well as multiple
RV aneurysms and areas of edema as well as multisegmental
transmural late gadolinium enhancement on both ventricles, setting
a differential diagnosis between sarcoidosis and myocarditis.
The patient underwent a PET-CT which ruled out the sarcoidosis. We performed a 3DEAM-guided EMB to target areas of edema and fibrosis on the interventricular septum and avoid false negative results, which showed signs of an inflammatory cardiomyopathy with B19V with active replication and started the patient on a therapy with interferon Beta which is a well-tolerated and safe treatment option, leading to effective virus clearance or reduction of the virus load in patients with chronic viral cardiomyopathy [5]. After two months of therapy, we repeated a c-MRI which showed an almost complete resolution of the edema with persistence of late enhancement as scarred myocardial tissue. The patient underwent a secondary prophylactic implantation of an ICD and is stable ever since, without having experienced any new arrhythmias.
Figure 1: ECG: sustained monomorphic ventricular tachycardia with an inferior axis and a right bundle branch block, rhythm
of presentation of the patient in case1.
Case 2
A 66-year-old woman was sent to our cardiology Department
after a secondary prophylactic implantation of an ICD, due to
sustained slow ventricular arrhythmias (LSB, inferior axis) after
a probatory therapy with amiodarone as well as with sotalol. The
echocardiography showed a mildly reduced EF (41%) with a diffuse
hypocontractility, more evident in the basal segments. There were
no echocardiographic signs for a dilated cardiomyopathy or for a
hypetrophic cardiomyopathy and a coronaroangiography made
in the first hospital had already ruled out any ischaemic cause of
the reduced EF or the VTs. As the VTs were of incessant nature the
patient underwent an emergency VT ablation of the RVOT-septal
focus. Even if the procedure had an acute success with termination
of the ventricular arrhythmias, one day after the ablation the VTs
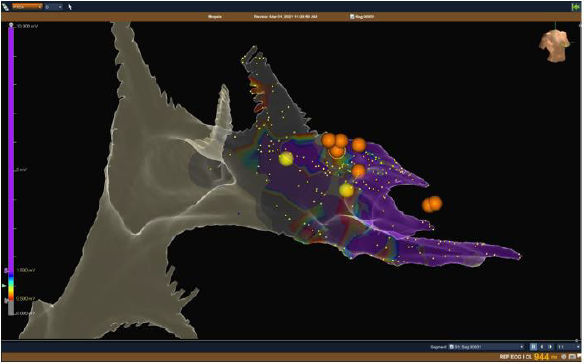
started again, and the patient was put on Mexiletine (Table 1).
Because of the unclear diagnosis of the origin of the ventricular
arrhythmias, their persistence after ablation, and the impossibility
to run a c-MRI because of the implanted ICD, we decided to perform
a 3DEAM-guided EMB which showed an active B19V replication.
We then began an immunomodulating therapy with interferonbeta,
under which a cessation of the ventricular arrhythmias was
documented. At the follow-up, after six months of interferonbeta
there were no sustained VTs anymore in the ICD-memory.
No control MRI could be performed because of the device in situ
(Figures 1 & 2).
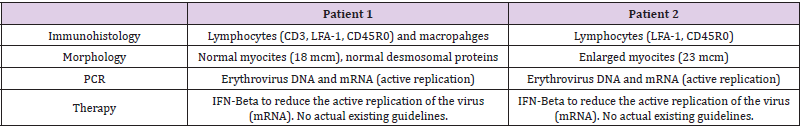
Figure 2: NavX Ensite Precision™ Image : bipolar voltage
mapping of the right ventricle showing healthy ventricular tissue in
purple (bipolar voltage > 1,5 mV) and scar ventricular tissue (grey,
< 0,5 mV) with pathological area identified with the color
coded scale. Right anterior oblique view with NavX Ensite Precision™
system. The yellow dots show the His Bundle
And the right fascicle
While the orange dots show the site in which the endomyocardial biopsy
has been made, targetting the fibrotic or edematous
tissue on the septal right ventricular wall.
Discussion
Even though for many years the medical research has failed
to show a causative role of B19V in the genesis of heart failure
confirming only an association [5-7], some more recent works
have reported that chronic viral infections of the heart can be
one antecedent event leading to progressive dysfunction of the
myocardium, often with an impaired prognosis due to a virus- or
immune-mediated myocardial injury [6]. Moreover, even if it is
known that myocarditis can lead to cardiac dysfunction and to
ventricular arrhythmias through the development of scars and
therefore reentry circuits [8] no direct association between B19V
persistence and those clinical pictures has been described.
As the diagnosis of viral myocarditis can be problematic and
the presentation can mimic other diseases such as sarcoidosis,
arrhythmogenic cardiomyopathy as well as an evolution in dilated
cardyomyopathy, the gold standard for the diagnosis and guide of the
therapy is the EMB, an invasive but safe diagnostic tool that allows
the quantification and identification of immune cell infiltrates, the
quantification of viral loads and confirmation of virus subtypes
via sequencing [9-14]. Hystorically, the EMB was performed under
fluoroscopy guidance and was associated with potentially critical
complications such as a cardiac tamponade. In the last years,
there has been an evolving and promising use of EMB guided by
3D-electroanatomic voltage mapping, which could confere a higher
specificity and sensitivity in targeting the involved tissue and in
reducing false negative results, could reduce the radiation exposure
of patients and operators in such procedures and present a higher
safety profile compared with the mono-dimensional fluoroscopy
images [15].
We described how two patients presenting with ventricular
tachycardias of unknown cause could be successfully managed after
a diagnostic 3D-EAM guided EMB after ruling out the most common
causes of ventricular tachycardia. In our patients a subacute viral
myocarditis caused by persistent erythroparvovirus, having
sustained ventricular tachycardias as clinical presentation and
demonstrating active replication of the virus, an immunomodulating
therapy with interferon Beta was able to stabilize and resolve the
ventricular arrhythmias. The 3D EAM guided EMB either combined
with cMRI or not, can help to improve specificity and sensitivity in
targeting the involved my-ocardial tissue and avoid false negative
results, without increasing risks for the patients, as already shown
in the literature [15,16].
Conclusion
To our knowledge this is the first case series described in
the literature. Even if we will need a greater number of patients
to confirm our observations, we hypothesize that B19V active
replication could have a pivotal role in some forms of myocarditis
which show an arrhythmogenic clinical presentation and that
diagnosing and treating B19V in patients with a subacute
myocarditis and ventricular arrhythmias could be determinant in
solving the arrhythmias as well as the myocardial inflammation,
although is not curative of the areas where the myocarditis
has already produced a myocardial scar. We also described the
emerging role of 3DEAM-guided endomyocardial biopsy in order to
target the involved myocardial tissue and reduce complications as
well as false negative results.
For more Articles on : https://biomedres01.blogspot.com/


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.