Genetic Testing and Counselling for Cancer: Evolution, Future and Psychological Impact
The field of cancer screening and testing has come a long way;
its evolution from basic biochemical tests screening for particular
analytes [1] to the use of gene-based testing and screening models
is a definitive example of the evolution of our understanding of
cancer syndromes and their underlying genetic basis. Identification
of people with cancer predisposition syndromes and germ line
pathogenic variants [2] has become easier with the advent
and utilization of genome-wide gene sequencing panels [3,4]
chromosomal arrays, and whole exome/genome sequencing
and, somatic tumor testing (especially for childhood cancers),
emphasizing the increasing necessity for both cancer predisposition
testing and genetic counselling programs specializing in the testing,
management and care of cancer [5].
Genetic counsellors are uniquely qualified to address
cancer risk, interpretation of genetic results, and the inevitable
complications of the subsequent ethical [6], legal and psychosocial
issues that are encountered by individuals dealing with this malady
[7,8]. Obtaining informed consent [5,6] from both minors and
adults, ascertaining the timing for a genetics referral, providing
periodic counselling and the associated aid overtime (especially
in the smooth transition of younger patients to adult/ geriatric
care) [8,9] and the dearth of childhood cancer predisposition
syndromes are some of the unique challenges that plague us today
[10]. Incidental findings due to the prevalence of genetic testing are
associated with their own set of psychological implications [11].
In countries like India, where there is enormous disparity
between socio-economic classes, a genetic counsellor will
encounter additional problems including the lack of awareness
and education amongst the under-privileged classes, genderand
religion-associated disparity in terms of cancer treatment,
management and the reality of the influence of political agendas
over government health policies.
Entry to Genetic Counselling
Referral to a genetic counselling clinic for cancer evaluation can
occur due to the prevalence of cancer syndromes within the family
(family history) [12], ethnicity [13,14], phenotypic expressions,
high-risk tumour types, non-oncological findings, like the lippigmentation
and greater the characteristic macules associated
with Peutz-Jeghers syndrome and neurofibromatosis type1 (and
bi-allelic mismatch repair) respectively and incidental findings
(variances in predisposition genes on chromosomal microarrays
and secondary findings detected by exome sequencing) [9]. Family
history alone, however, is not a reliable factor when accounting
for the necessity of a referral as cancer predisposition has been
reported in many cases of absence of said history [10], This can
be due to the formation de novo variants, parental germ line
mosaicism [15], increasing incidence of smaller nuclear families,
low penetrance and recessive inheritance masking an inherited
syndrome. Hence, a combination of the aforementioned factors
should be taken into account when making a genetics’ referral.
Moreover, the future holds the possibility population based genetic
testing for cancer predisposition syndromes.
Oncologists are confronted with the possibilities of identifying
whether reported variants are indicative of somatic changes or
inherent germ line susceptibility [16] and thus subsequent referral
to a genetics’ clinic for their particular expertise becomes necessary.
Timing of Genetic Counselling Initiation
The optimal timing of the first genetic counselling session is at the time of tumor diagnosis or after the initiation of treatment in cases of poor prognosis, to ensure that the possibility of prophylactic surgery is considered. The genetic counsellor is qualified to advise the patient on many issues associated with the patient prognosis, associated treatment plans and psychological developments [17,18]. In the case of poor prognosis, DNA banking should be administered, and genetic testing organized in a timely manner in order to assess and counsel their relatives to minimize the economic and psychological burden of post-mortem testing.
Pre-Test Genetic Counselling
Informed consent should be obtained from the patient before they undergo any genetic testing procedure. This involves complete discussion of all aspects related to the test and consequent implications, including information regarding tests most suitable to the patient (based on the various factors that have prompted the referral), the surveillance protocol that may follow (especially in cases of transition from childhood to adulthood), psychosocial [11], ethical and privacy concerns, which all vary in accordance with the laws of different countries, and plans for disclosing results to at-risk relatives [6,19]. Adults are required to provide verbal and written assent towards the procedure; minors should be guided through these discussions in an age-appropriate manner and adolescents should provide verbal and written consent in conjunction with their parents or primary guardians [9]. This allows older children to become involved with and more accustomed to their unique situation and have any fears or misconceptions addressed. The basic tenet of genetic counselling is to give patients the tools required for them to make informed autonomous decisions [20] regarding the testing and management options available to them based on factual (stratified) risk information [21-25]. Despite concerns of exacerbating patients’ anxiety, genetic testing in the absence of prior genetic counselling is linked with negative outcomes including the violation of ethical standards, ordering of unnecessary, perhaps costly, genetic tests, misinterpretation of these results and adverse effects on the patients’ psyche.
Genetic Testing
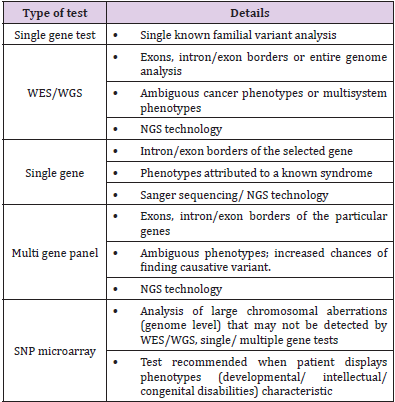
The invention of Next Generation Sequencing (NGS) technology is the biggest advancement in genetic testing seen in recent years wherein analysis is performed at a multiple gene level, or even whole transcriptomic, genomic and exomic levels, at a relatively lower cost, especially when the increased sensitivity and efficiency of obtaining results are taken into account [16]. A test should be ordered after consultation with a genetic counsellor and the choice of laboratory should be based on the type of test, its level of analysis, methodology and their variant interpretation techniques, expenses involved, time factors and their policies on privacy and ethics. The variants are reported in accordance with the five-tier classification proposed by The American College of Medical Genetics and Genomics (ACMG), namely, pathogenic, likely pathogenic, variant of uncertain significance, likely benign and benign [9,26]. Despite the succinctness of this model, further interpretation by an expert is important especially when deciding the significance/ level of pathogenicity of variants (Table 1).
Table 1: Genetic tests for cancer gene mutation.
Note: {WES – Whole Exome Sequencing; WGS – Whole Genome Sequencing, NGS – Next Generation Sequencing, SNP – Single Nucleotide Polymorphism}
The sensitivity of these tests for identification of pathogenicity varies from greater than 95% to less than 50% and thus, a genetic counsellor must provide counsel on risk perception and management options based on empirical data and in conjunction with the oncologist. Identification of variants without certain significance tailors the advised management options to include surveillance protocols and the possibility of family variant tracking. Relatives can be tested for these only when consent is provided by the patient [6]. The inheritance patterns associated with the identified pathogenic variant determine the relatives who are atrisk. For example, if a syndrome follows an autosomal dominant pattern of inheritance, there is a 50% risk of inheriting a pathogenic variant, and its associated risks, to first-degree relatives of the proband [16,27].
Post- Test Genetic Counselling
For those individuals with a positive diagnosis, post-test counselling involves specific treatment/ management options and the necessity of periodic evaluation. In cases of childhood diagnosis of a hereditary cancer syndrome, reproductive and psychological implications especially, change over increasing age. Hence, lifelong risk management, and understanding of the options for reproductive (post- and pre-natal) counselling [28], testing post-birth, adoption, and/or utilizing donors is disseminated with increasing age of the patient in an appropriate manner suited to the child’s developmental stage8,9. Surveillance options [29] and information regarding the advent of new testing options can only be provided for at-risk individuals/ families if periodic follow-up with the genetic counsellor is maintained.
Psychological and Sociological Implications
Negative effects on the psyche of a patient with a positive
diagnosis are primarily concerned with surveillance protocols
and the reality of a life-long economic burden8. Invasive medical
procedures [30], procedures requiring sedation or general
anesthesia, false positive results, incidental findings are implicated
by various studies in causing psychological distress to the patient
and their families. There arises a general frustration with lack of
positive results when it comes to therapies advised, inconclusive
outcomes of tests and the delivery of false-positive results
(increased in whole-body MRIs) [31], impaired quality of life,
reduced satisfaction with care, and worse overall survival. Patients
undergoing surveillance may experience anxiety with regards to
scanning, referred to as “scanxiety”, and children especially may feel
adversely towards repeated blood draws and the claustrophobic
confinement experienced during MRI scans [9]. Young adults
face an ever-increasing economic burden as they are as of yet not
financially secure enough, and may not even possess insurance
cover [20], to support life- long management programs.
On the contrary, proactive surveillance and psychological
support, from say, cancer survivor groups, may empower the
patient and are viable avenues to lead a more well-adjusted life. The
patient relies on the care team in such scenarios due to generation
of trust and confidence in their counsel [32,33]. Cancer genetic
counselling in India. In India, there are about a million cases of
cancer diagnosed yearly. When the population of the subcontinent
is taken into account, these rates of incidence and mortality, match
those seen in high-income countries [34]. These elucidate the lack
of early-detection strategies and positive results of treatments
within the medical landscape of the country [35].
Studies show that breast, lung, oral, cervical, gastric and
colorectal cancers [36] have the highest incidence rates in India. It
is evident that most causative agents implicated in cancer in the
Indian population are avoidable (tobacco and alcohol consumption,
lack of education with respect to female hygiene) [34,37]. There is
a general lack of education and support for the low-income, socially
underprivileged families owing to the fallacies of an increasingly
capitalist state of government [38-40]. Even governmental policies
regarding general health are found to be inadequate in the face of
growing mortality due to cancer. It is the second-leading cause of
death amongst the Indian population.
A patriarchal society has also generated the spread of female
reproductive cancers as the importance of feminine hygiene is not
acknowledged by many; additionally, a greater economic burden to
finance health care is placed on women [41]. In conjunction with
the lack of resources and such a mind-set, most evidently seen in
under-privileged communities, the incidence of cervical cancers
has witnessed an increase over the past 5-10 years. In India, the
age of onset of the female reproductive cancers is around a decade
earlier than that of developed nations (45-50 years in the former,
compared to >60 years of the latter) [42]. Moreover, oncofertility
can be improved by developing management, treatment strategies
that comprise of professionals from multiple specialties, say a
counselling team that includes a reproductive endocrinologist [43]
apart from an oncologist, psychologist and the geneticist. Hence,
advancement of cancer-associated clinical programs with respect
to diagnosis, screening, management/ treatment particular to the
Indian race [44] are a necessity in the mission to better the state of
women’s health in India [42,45].
Conclusion
Cancer testing and management is an ever-growing field
primarily due to our increasing understanding of unknown
syndromes and their underlying genetics, and the expansion of
available information of known cancer syndromes. In accordance
with these basic developments, there should be a correlating
evolution in the various genetic testing and counselling practices
available for the same. These take the form of improved access
to aforementioned resources and formulations of government
policies that tackle health care from this perspective [45]. One
such advancement can be the necessitation of population-based
genetic screening [46,47] and testing for common pathogenic
variants of the most abundantly found cancer syndromes, e.g. BRCA
1 and 2 testing for breast cancer [4,42,48]. This type of policy can
hold many implications in reducing the burden of cancer in many
developing economies, like India. In the same vein, there have been
discussions on the use of e-health interventions [49] like psychoeducational
interventions delivered via web-based environments
with auxiliary methods of communication, which includes support
with professionals and peers, offer improved awareness and
access to the required support for informed, autonomous decisionmaking.
Personalized medicine is an avenue of modern medicine
gaining quick popularity as it is tailored to an individual and their
needs. Corroborating advancements in cancer genetic testing and
counselling to personalized care will initiate the incidence of more
positive outcomes as it pertains to lifelong care and management
practices [5,11,18,50,51].
For more Articles on : https://biomedres01.blogspot.com/


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.