Is Obstructive Sleep Apnea A Risk Factor for Severe Acute Respiratory Syndrome Coronavirus 2 Infection?
Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARSCoV-
2) has emerged as public health crises first in the city of Wuhan,
Hubei province in China in December 2019, and has subsequently
turned out to be a global problem. Coronavirus Disease 2019
(COVID-19) may present in a wide spectrum of clinical forms ranging
from mild symptoms such as fever, cough, or fatigue to severe
pneumonia, septic shock, organ failure, or death. Understanding
risk factors for disease susceptibility and severity is essential to
prioritize target populations and patients that are at most risk.
Which factors predict the susceptibility to COVID-19 and the
severity of the infection have been studied earlier. Diabetes mellitus
(DM), hypertension, respiratory and cardiovascular disorders are
among the factors with high consistency of association to lifethreatening
outcomes [1]. COVID-19 and obstructive sleep apnea
(OSA) share many demographic characteristics and comorbidities
such as advanced age, male gender, obesity, hypertension, cardiac
complications, and DM. Both OSA and COVID 19 are associated with
pro-inflammatory mediators. Coronavirus-2 enters the cell with
the help of the Angiotensin-Converting Enzyme-2 (ACE-2) receptor.
The number of ACE-2 receptors in adipose tissue increases in obesity [2]. Hypoxemia in OSA may affect the coagulation cascade
and enhance the tendency to coagulation caused by COVID 19
[3]. Taken together, sharing the mentioned putative risk factors
in common, is OSA risk and poor prognostic factor for COVID-19
infection?
There are several studies focused on the frequency of OSA in COVID-19 patients and the effect of OSA on the prognosis of COVID-19 [4,5]. However, there are not enough data in the literature regarding the prevalence of COVID-19 in the population with OSA. In our study, we aimed to evaluate the prevalence of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection in patients diagnosed with OSA and the effect of OSA on the severity of the infection in these patients.
Material and Methods
We conducted a retrospective observational study in the OSA
population diagnosed by polysomnography (PSG) in our clinic.
The records of consecutive patients who underwent PSG between
March 2015 and March 2020 in our clinic were reviewed. OSA
was diagnosed using overnight PSG. The standard overnight PSG
included electroencephalography, electrooculography, submental
and bilateral leg electromyography, and electrocardiography
recordings. We measured airflow with a nasal pressure transducer
and an oronasal thermistor, respiratory effort via respiratory
inductance plethysmography, and arterial oxyhemoglobin
saturation via a finger pulse oximeter. Experienced technicians
collected and digitalized all signals using computerized PSG
systems (Comet Grass: Astro-Med, Inc., West Warwick, Rhode
Island, United States, and Viasys Cephalo-Pro, SomnoStar: VIASYS
Healthcare, Hochberg, Germany) following established standards
[6]. Certified sleep specialists, experienced in sleep medicine,
scored sleep stages using the American Academy of Sleep Medicine
(AASM) scoring system [7,8]. Grading of the apnea-hypopnea index
(AHI) followed AASM’s 1999 criteria as follows: an AHI less than 5
was normal, an AHI higher than 5 but less than 15 was mild, an AHI
higher than 15 but less than 30 was moderate and an AHI higher
than 30 was severe [9].
The electronic medical records of the Public Health Management
System were queried for the results of the SARS-CoV-2 polymerasechain-
reaction (PCR) tests for all these subjects with PSG confirmed
sleep disorders. Whether the subjects have been tested for SARSCoV-
2 with PCR and the test results were recorded. For patients
with positive tests, the demographic data, results, and diagnoses of
the sleep study were recorded. Comorbidities were ascertained by
ICD-10-CM coding and medical record data. A case of Covid-19 was
defined by a positive result on a PCR assay of a specimen collected
on a nasopharyngeal swab. The clinical findings, laboratory and
radiological data, outpatient/inpatient treatment status, and the
course of the COVID-19 of the patients with positive PCR tests were
recorded.
The Study Protocol was Approved by the Local Ethics Committee
All statistical analyses were performed using SPSS software (version 17.0). For baseline characteristics, mean (standard deviation) for continuous variables and number and percentages for categorical variables were calculated. Given that this is a descriptive study, no analysis for statistical significance was performed.
Results
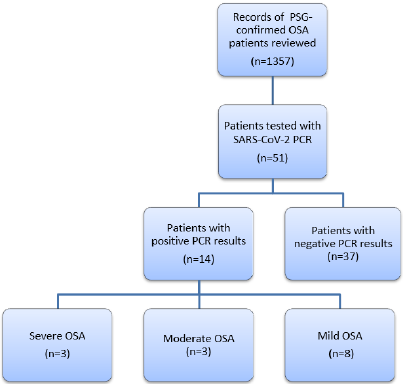
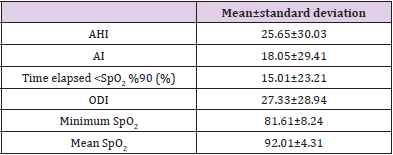
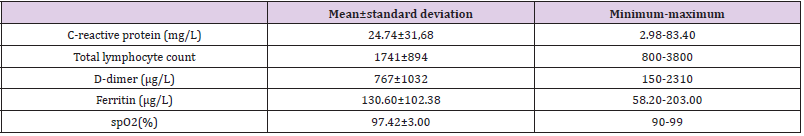
Our analysis included 1317 OSA patients diagnosed by PSG. A review of the medical records demonstrated that 51 patients have been tested for SARS-CoV-2 with PCR. The reasons for testing were suspicion of infection, contact tracing, scanning before hospital admission or interventional procedures, or screening for travel. We identified 14 patients with positive PCR results for SARSCoV- 2 (Figure 1). The mean age of the 14 patients was 48.9 ± 12.1 years. The majority of the patients were male (n=13, 93%). The mean BMI was 29.7 ± 2.4 kg/m2. The polysomnographic data is demonstrated in Table 1. Eight (57%) cases had mild OSA, three (21%) had moderate OSA, and three (21%) had severe OSA. Three cases were asymptomatic. Main complaints were chest pain (n=6, 43%), fever (n=5, 36%), fatigue (n=3, 21%), cough (n=3, 21%), shortness of breath (n=3, 21%), loss of taste and smell (n=2, 14%), and diarrhea (n=1, 7 %). Two patients (14%) had DM and two (14%) had hypertension. Two patients (14%) did not need radiological evaluation. Others underwent computed tomography (CT) scanning; normal CT findings was observed in six cases (43%); involvement was unilateral in three cases (21%) and bilateral in three (21%) cases. The mean percentage of oxygen saturation was 97.4±3.0(90-99) on initial evaluation. The laboratory data of COVID-19 patients is demonstrated in Table 2. All the patients underwent outpatient treatment and no hospital or intensive care unit (ICU) admission, progression to respiratory failure or mortality was observed.
Table 1: The polysomnographic data of OSA patients with COVID-19.
saturation
AHI: apnea–hypopnea index (events per hour); AI: apnea index (events per hour); ODI: oxygen desaturation index (events per hour); spO2: Arterial oxygen three(21%) had moderate OSA, and three(21%) had severe OSA.
Discussion
We have observed that the prevalence of COVID-19, the need
for hospitalization, and progression to respiratory failure, namely
severe infection did not seem to increase in OSA patients. In our
large OSA population, no hospital admission or death occurred
due to COVID-19. Recognition of conditions substantially
associated with significant morbidity and mortality is essential
to offer prudent preventive measures to vulnerable populations.
Theoretically, OSA patients should have increased susceptibility
and severity for SARS-CoV-2 infection as they share essentially
identical risk factors. Due to overlapping predisposing factors, OSA
patients are thought to show a heightened risk of poor outcomes
in the case of COVID-19. Our findings are contradictory to this fact.
Several studies including a small population of severe COVID-19
patients have shown that 21-28% of patients had OSA (10,11) A
recent study on the relationship between OSA and risk of COVID-19
infection has revealed that the risk for COVID-19 infection was
about 8-fold greater in OSA patients. The authors stated that the
risk of hospitalization and respiratory failure increased, as well
[12]. Obesity predisposes to OSA [13]. Links between obesity and
COVID-19 have been investigated. In a recent analysis, obesity has
been reported as an independent risk factor for invasive mechanical
ventilation in COVID-19 patients [14].
Up through January 22, 2021, a total of 28.195.901 tests have
been applied and 2.418.472 people had tested positive for the new
SARS-CoV-2 coronavirus in Turkey. The total number of deaths
is 24789 [15]. These data reveal that about 3% of the Turkish
population has been infected with SARS-CoV-2. Concerning these
data, the prevalence of COVID-19 in our selected population does
not seem to be higher than the general population. One possible
explanation is the fact that this specific cohort, as well as their
families are aware of the increased risk of morbidity and mortality
from Covid-19, due to their comorbid medical conditions, such as
obesity, hypertension, diabetes, and thus, they were extra cautious about exposures. One major problem with treatment in OSA is
nonadherence to CPAP treatment. CPAP adherence has been
shown to improve significantly during the COVID-19 lockdown
[16]. Staying at home, travel restrictions, and the fear of having a
poor prognosis, and the probability of being hospitalized might
have been motivating factors in better CPAP adherence [16]. This
may be considered as a protective factor for OSA patients. The
current study has several limitations. Coding and recording of
data may be imprecise and missing. Still, the administrative data
we based our investigation on is very reliable. Our data reflect OSA
as it is diagnosed by PSG. However, OSA is widely underdiagnosed,
therefore the true prevalence is probably higher. It may be argued
that some OSA patients might have PCR negative COVID-19
infection, on the other hand, the same argument may be true for
all the population. In the population we reviewed, all OSA patients
who had negative PCR results have been on basis of screening. They
had no infection symptoms or signs.
In contrary to previous reports suggesting an increased risk
of COVID-19 in OSA patients, our study represents novel data on
the incidence of COVID-19 in population with confirmed OSA. To
our knowledge, this is the first study to claim that susceptibility,
severity, and mortality are not increased in COVID-19 patients with
sleep disorders.
Conclusion
Our results provide some initial data regarding COVID-19
risk in a large OSA population. We demonstrated that OSA cannot
be considered as one of the underlying medical conditions
predisposing to increased risk or poor outcome in COVID-19. Poor
COVID-19 related prognosis, if exists, may be attributed to other
risk factors or comorbidities accompanying OSA. We have observed
that the prevalence of COVID-19, the need for hospitalization, and
progression to respiratory failure, namely severe infection did not
seem to increase in OSA patients. In our large OSA population,
no hospital admission or death occurred due to COVID-19.
Recognition of conditions substantially associated with significant
morbidity and mortality is essential to offer prudent preventive
measures to vulnerable populations. Theoretically, OSA patients
should have increased susceptibility and severity for SARS-CoV-2
infection as they share essentially identical risk factors. Due to
overlapping predisposing factors, OSA patients are thought to show
a heightened risk of poor outcomes in the case of COVID-19. Our
findings are contradictory to this fact. Several studies including a
small population of severe COVID-19 patients have shown that 21-
28% of patients had OSA [10,11] A recent study on the relationship
between OSA and risk of COVID-19 infection has revealed that
the risk for COVID-19 infection was about 8-fold greater in OSA
patients.
The authors stated that the risk of hospitalization and
respiratory failure increased, as well [12]. Obesity predisposes
to OSA [13]. Links between obesity and COVID-19 have been
investigated. In a recent analysis, obesity has been reported as
an independent risk factor for invasive mechanical ventilation
in COVID-19 patients [14]. Up through January 22, 2021, a total
of 28.195.901 tests have been applied and 2.418.472 people had
tested positive for the new SARS-CoV-2 coronavirus in Turkey. The
total number of deaths is 24789 [15]. These data reveal that about
3% of the Turkish population has been infected with SARS-CoV-2.
Concerning these data, the prevalence of COVID-19 in our selected
population does not seem to be higher than the general population.
One major problem with treatment in OSA is nonadherence to
CPAP treatment. CPAP adherence has been shown to improve
significantly during the COVID-19 lockdown [16]. Staying at home,
travel restrictions, and the fear of having a poor prognosis, and
the probability of being hospitalized might have been motivating
factors in better CPAP adherence [16]. This may be considered
as a protective factor for OSA patients. The current study has
several limitations. The study does not include a control group
to determine the prevalence of hospitalization or severe disease
in a cohort without OSA. Still, we have the prevalances from the
total population to compare the prevalence of the cohort. Coding
and recording of data may be imprecise and missing. Still, the
administrative data we based our investigation on is very reliable.
Our data reflect OSA as it is diagnosed by PSG. However, OSA is
widely underdiagnosed, therefore the true prevalence is probably
higher. It may be argued that some OSA patients might have PCR
negative COVID-19 infection, on the other hand, the same argument
may be true for all the population. In the population we reviewed,
all OSA patients who had negative PCR results have been on basis of
screening. They had no infection symptoms or signs.
In contrary to previous reports suggesting an increased risk
of COVID-19 in OSA patients, our study represents novel data on
the incidence of COVID-19 in population with confirmed OSA. To
our knowledge, this is the first study to claim that susceptibility,
severity, and mortality are not increased in COVID-19 patients
with sleep disorders. In conclusion, our results provide some
initial data regarding COVID-19 risk in a large OSA population.
We demonstrated that OSA cannot be considered as one of the
underlying medical conditions predisposing to increased risk or
poor outcome in COVID-19. Poor COVID-19 related prognosis,
if exists, may be attributed to other risk factors or comorbidities
accompanying OSA.
For more Articles on : https://biomedres01.blogspot.com/

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.