How COVID-19 Pandemic Indirectly Affected Orthopedic Patients: A Case Report of a Rescue Treatment For a Proximal Humerus Nonunion
Introduction
Humeral fractures account for 5% to 8% of all fractures, whereas proximal humerus fractures represent the seventh most frequent fractures in adults [1,2]. Nonunion is a complication that occurs in 15% of all the humeral fractures [3] and its incidence increases in case of proximal humerus fracture [4]. Risk factors are advanced age, osteoporosis, obesity, smoking, alcoholism, and infection. Comminution and impaction of fractures and loss of fixation also contribute to the develop of nonunion [5,6]. This condition results in pain and loss of shoulder function. The management of proximal humerus nonunion is challenging and often the results are disappointing. Treatment of these kind of complications include open reduction and internal fixation with bone grafting but often it is an unsuccessful treatment resulting in bad clinical outcomes and further surgery is required. Other options are fixation with tension wires or with intramedullary nail [7].
These are optimal options for bone of good quality such as in young patients and with no signs of gleno-humeral arthritis. Shoulder arthroplasty is a reasonable option in case of proximal humerus nonunion associated with a rotator cuff damage and osteoporosis [8]. This case-report describes a proximal humeral nonunion in a 69-year-old woman who was first treated with an external fixation before the advent of COVID-19 pandemic. After removing the external fixator (EF), she was lost at follow-up because of the closure of our department during the Italian lockdown. She came back after seven months with pain and functional limitation. X-Ray reported a nonunion of proximal humerus. In the end she underwent to reverse shoulder arthroplasty, recovering with a good result.
Case Report
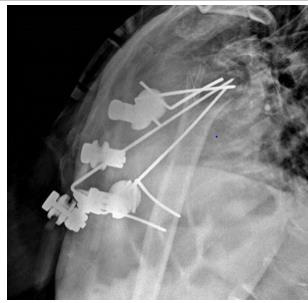
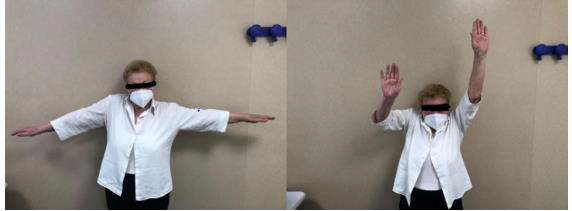
A 69-year-old woman came to ER of Poliambulanza of Brescia in October 2019. X-rays were obtained. Fracture involved proximal humerus of the right, dominant, upper arm. The fracture was 11C3.1 according to AO classification. At first, the fracture was treated with an external. fixation using a Galaxy EF in the first twenty-four hours. The EF was removed after one month because of the loss of reduction with displacement of the fracture. Physio- kinesitherapy was indicated but she was unable to underwent to treatment. She was lost at follow -up for several months due to COVID-19 pandemic and the social limitations that resulted. After 7 months, Xrays showed a dislocated nonunion of proximal humerus with necrosis of the head. She complained shoulder pain with passive elevation of 40° and scapular dyskinesia. In March 2021 she was listed for a reverse shoulder arthroplasty. During the surgery, Synovasure test and white blood cell count were performed: both tested negatives. A cemented trauma stem “Equinoxe” by Exactech number 8 mm was applied with a standard baseplate fixed with three screws of 26, 18, 18 mm. External rotators were reinserted, and range of motion (ROM) was good at three months follow-up.
Discussion
The impact of COVID-19-related restrictions has resulted in changes in patients’ healthcare and follow-up. During the pandemic, injured patients have experienced difficulties in receiving medical assistance, due to the lack of healthcare personnel and fear of contagion. Lombardy was the most affected region of Italy and orthopedic surgeons were involved in the emergency as other specialists [9,10]. Our level-2-trauma center in Brescia (Lombardy) went on admitting injured patients unceasingly, since several domestic accidents happened during that time, despite reports out of Italy noted a 65% reduction in trauma services provided for shoulder and elbow injuries during the time residents were asked to stay in the home [11]. One of the effects of the pandemic was the loss of follow-up of outpatients [12]. It is hypothesized that the main causes of this issue were the isolation and the fear of contagion in hospital environment [10] (Figure 1).
Radiographic checks showed a partial loss of reduction and physio-kinesitherapy was indicated but she was unable to underwent to treatment because of the new social restrictions. Further radiographs showed gradual loss of reduction. Therefore, we started contemplating a definitive treatment by performing a ORIF with bone graft or a shoulder arthroplasty, but at that moment, the patient was lost at follow-up. Given the poor bone quality, after the removal of the EF, we would probably have implanted a hemiarthroplasty or a reverse prosthesis with a press-fit primary humeral stem fixation, considered an optimal choice because of the possible easier revision, decreased operative time, healing time, and resolution of the symptoms [16]. After 7 months, the patient came back to our department, suffering from pain and severe functional limitation, compounded by a preternatural movement of the joint. Radiographs showed evident dislocated nonunion with reabsorption of tuberosities and metaphysis.
Therefore, our choice has been to implant a reverse shoulder prosthesis with a cemented trauma stem “Equinoxe” by Exactech number 8 mm. This choice involved several compromises like technical difficulties due to the severe bone loss and higher risks of dislocations, infections, nerve injuries and thromboembolism due to the use of cement, compared to an arthroplasty with a pressfit stem [17-20]. At three-month follow-up, the patient showed no pain and a sufficient function of the joint. Since the exact amount of loss to follow-up is not valuable, there is a chance that cases of nonunion in longstanding fractures like this could increase in the near future. Our experience shows that cemented stem fixation can be an important choice of treatment for these patients. Other strategies, like telemedicine, should be considered and eventually implemented to prevent this kind of consequences resulting from the pandemic [21-23].
For more
Articles on : https://biomedres01.blogspot.com/





No comments:
Post a Comment
Note: Only a member of this blog may post a comment.