Oral Manifestations of Behcet’s Syndrome: Case Report
Introduction
Systemic diseases may be preceded or spread, with oral
manifestations. The lesions of the oral cavity are attended, for the
most part, by Stomatology Specialists, so that knowledge of the oral
manifestations of systemic diseases contributes to correct behavior
in the face of these conditions that, finally, must be referred to
the specialist in the attention of each one of them [1]. Behcet’s
syndrome is an autoimmune disease of the seronegative vasculitic
type, with a disease of vessels of variable caliber [2]. Although the
etiology of Behcet’s Syndrome is unknown, there are numerous
investigations that indicate the participation of genetic, infectious
(viral and bacterial) and immunological factors. Among the most
important are the association with the HLA genotype of the patients,
the cross-reactivity with human peptides and the activation of
the vascular endothelium [3]. This disease is more common and
severe along the old “silk road”, which extended from East Asia to
the Mediterranean, Turkey’s current territory. 80 to 370 cases are
reported per 100,000 inhabitants in Turkey, while the prevalence
ranges from 13.5 to 35 per 100,000 in Japan, Korea, China, Iran, Iraq
and Saudi Arabia; being a more severe manifestation in Japan [4].
In relation to sex, a predominance of female sex in countries of
America and male sex in Asia is described, mainly between the ages
of 20 and 40 [5]. In Cuba there are no prevalence studies of this
entity [3]. The first description made of this pathology arises may
have been described by Hippocrates in his third book of endemic
diseases [4]. In 1930, the Greek ophthalmologist Benediktos
Adamantiades reported to a patient with arthritis, oral and genital
ulcers, phlebitis, and iritis but it was not until 1936 that the
Turkish dermatologist Hulsui Behcet determined the description of this disease of more accurate way [6]. The clinical spectrum
of this disease, characterized by a symptomatic triad (recurrent
oral and genital ulcers with uveitis and hypotension) in addition
to the fact that the histopathological study of the affected organs
and the analytical data are nonspecific, makes its diagnosis based
on the clinical method of description and grouping of signs and
symptoms [7]. In 1990, the criteria for the diagnosis of this entity
were established for the first time by the International Study Group
for Behçet’s Disease [8].
In 2006, new diagnostic criteria of the International Group for
the study of Behcet’s disease were established [9], which declared
a major or mandatory criterion: recurrent oral ulcers and minor
criteria: recurrent genital ulcers, eye lesions, skin lesions, vascular
lesions and positive patergia test [10]. In 2013, the international
criteria for the diagnosis of the disease were reviewed, as a result
of the analysis they proposed to award 2 points to ocular lesions
and oral and genital aphthous lesions and assign 1 point to skin
lesions, of the Central Nervous System, vascular manifestations and
the positive patergia test. According to these criteria, a patient with
a score ≥ 4 points is classified as a Behcet disease [3]. At present it is
known that it is not curable, but treatable [4]. The goals of therapy
are to: suppress inflammation, reduce the frequency and severity of
recurrences. To be effective, treatment must be implemented early
[11]. Objective: Describe the oral manifestations and therapeutic
behavior to be followed before a patient with Behcet syndrome.
Case Presentation
Patient of 20 years of age, female sex, black race, urban origin, who comes to the emergency services of Maxillofacial Surgery of the body of guard of the Dr. Gustavo Aldereguía Lima Hospital in Cienfuegos, Cuba referred by the specialist in Stomatology General Comprehensive that provided services in the area of health corresponding to the patient for presenting multiple ulcerated lesions throughout the oral cavity and lips Figure 1.
Anamnesis
During the interrogation, the patient was referred to as inflammation of the entire oral cavity, pain during food intake and difficulty swallowing (dysphagia), burning sensation and burning of the mouth, halitosis, recurrent episodes (7 to 8 times a year) ulcerated bleeding lesions, which previously healed spontaneously until their total disappearance but during the last episode the lesions persist. It also refers to the presence of genital ulcers, skin rash in the frontal region and persistent joint pain.
Physical Exam
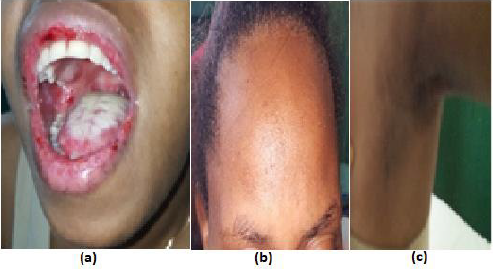
Multiple ulcers were detected in the oral cavity of approximately 1cm and more, covered by a yellowish-green pseudo membrane and with fetidity due to the over-added infection of the lesions, with irregular, undefined, elevated, rounded, hyperemic edges, bleeding to the minimum stimulus, painful on palpation, located in the region of the oropharynx, tongue, palate, gum, floor of mouth, mucosa of cheeks and lips Figure 2a. In addition, irregular and rough surface was detected upon palpation of the frontal cutaneous region Figure 2b and in the left axillary and subaxillary region Figure 2c. The case of the patient was consulted with the Internal Medicine services for a better treatment of genital lesions and joint pain.
Figure 2:
(a) yellowish-green pseudo membrane located in the tongue and oropharynx;(b) Skin rash in the frontal region;
(c) Irregular and rough surface in the left axillary and subaxillary region.
Complementary Exams
The following complements were indicated:
a) Blood count
b) Leukogram
c) Blood chemistry
d) Hepatic Profile
e) HIV serology
f) Rheumatoid Factor
g) C-reactive protein
h) LE cells
i) Immunoglobulins Serum
j) Patergia test
k) Surface antigen
l) Hepatitis C antibody
The results of the complementary examinations were within
the normal parameters except the Leukogram in which there was
a considerable increase in segmented leukocytes (neutrophils)
with a value of 80%, which showed that the over-added infection
of the lesions was bacterial. During the patergia test, a small sterile
needle was inserted into the skin of the forearm, causing a small
red papule to appear at the needle insertion site one or two days
after the test was performed, which indicated hyperreactivity of the
immune system to minor trauma or damage Figure 3. It is not 100%
specific, only a proportion of patients with Behcet syndrome have
a positive response.
Diagnosis
With these results, some possible diagnoses were ruled out: Human Immunodeficiency Syndrome, Rheumatoid Arthritis, Hepatitis B and C, Herpes Simplex type 1, Recurrent Aphthous Stomatitis, Parvovirus, Discoid Lupus Erythematosus. Finally, the patient was diagnosed with Behcet Syndrome with a scientific basis in the criteria for the diagnosis of this syndrome of 2013, complying with the mandatory or major requirement: recurrent oral ulcers in oral mucosa with a minimum of 3 episodes during a year (2 points ) and with three minor criteria: genital ulcers (2 points), erythema nodosum (1 point) in this case in the left frontal, axillary and subaxillary region and positive patergia test (1 point). According to this current classification criterion it is only necessary to accumulate a score ≥ 4 points, in this case the patient added a total of 6 points.
Treatment
As part of the Stomatological treatment, the patient was
indicated a series of hygienic dietary measures such as: eliminating
or reducing acidic foods from the diet (lemon, orange, tangerine,
pineapple, guava, tomato, natural yogurt); avoid ingesting foods
with artificial condiments and at elevated temperatures and instead
use natural condiments and ingesting food and drinks that are
refreshing but not gaseous; Eliminate local irritants such as coffee,
cigar and alcohol. In addition, local topical anesthetics such as 0.2%
lidocaine were indicated half an hour before eating food to relieve
the pain caused by chewing and swallowing in these cases. In this
case, the indication of mouthwash with saline solution or 20%
chamomile tincture was very effective, 20 drops in 200 milliliters
of boiled water 3 times a day for 7 days, the use of chamomile was
preferred as part of the natural medicine treatment and traditional
for its properties: anti-inflammatory, analgesic, antibacterial,
antiulcer, antiviral and antifungal.
The Internal Medicine services treated the patient with a
prednisone in a 20-milligram bulb intravenously every 8 hours, then
gradually reduced to a maintenance dose of 10 milligrams orally
in tablets, this corticosteroid was very effective in the treatment of
inflammatory component of oral, genital and arthropathic lesions
of the patient and as an immunomodulator. In addition, colchicine
(0.5 mg) was given one tablet every 8 hours; methotrexate (2.5 mg)
four tablets in weekly dose; folic acid (5 mg) one tablet daily, except
on the day of Metrotexate, all in order to control the rheumatologic
component. Currently, the patient is compensated for the disease.
Discussion
Systemic diseases are those morbid processes that affect more
than one organic system. The etiopathogenesis of many of these
diseases is still not completely clear, but it is well known that, in
large part of them, inflammatory processes and immune system
disorders that give rise to the various manifestations are involved.
The majority of patients with recurrent oral aphthous ulcers
have no other involvement, but in others the presence of chronic
aphthous stomatitis lesions is associated with systemic processes
[1]. Behcet’s syndrome is a very rare autoimmune disease condition
in these latitudes [4]. The most accepted concept so far defines it as:
in a chronic, multisystemic, recurrent inflammatory process whose
main alteration lies in a vasculitis that involves the arteries and veins
of any caliber. It is characterized in the clinic by presenting patients
with inflammation of the mucous membranes, translated by oral
and genital ulcers; in addition to uveitis; digestive symptoms, skin
lesions, arthritis and occasional neurological intake.
The etiology of Behcet’s disease is unknown and although the
majority of cases are sporadic, some studies support the possible
genetic origin with evidence of autosomal recessive inheritance
as it is reported that in 1 in 10 families there is another member
with the disease or other autoimmune diseases in first-degree
relatives such as hypothyroidism, scleroderma, discoid lupus
erythematosus and juvenile idiopathic arthritis. Another of the
arguments described in defense of this genesis is the increased risk
of suffering from Behcet’s disease when it is associated with the
presence of the HLA-B51 main histocompatibility system antigen
[12]. It is believed as for many autoimmune or auto-inflammatory
syndromes, that certain infectious factors (in particular,
Streptococcus antigens) and / or environmental factors are capable
of triggering symptoms in individuals with certain genetic variants
[13]. In some investigations, the herpes simplex virus type 1 and
parvovirus B 19, among the triggers of Behcet’s syndrome, other
research reports that in this syndrome there is an alteration in the
number and activation of lymphocytes, so the CD4 + / CD8 + index
inversion has been observed.
The syndrome is usually more serious and frequent in men
[3], however the case presented corresponds to a female patient.
The white skin color shows a predominance, although there is
a great miscegenation in Cuba [12], this ailment is uncommon in
the black population but when it appears they present greater
complications and worse prognosis [14]. Over the years different
criteria have been used to diagnose the disease, the International
Study Group for Behçet’s Disease in 1990 considers the existence of
recurrent oral ulceration with at least two of the following clinical
manifestations: recurrent genital ulceration, ocular involvement,
involvement cutaneous or positive patergia test to make the
diagnosis [8]. In 2006 the International Group declares it necessary
to present: Mandatory Criteria or major criteria: recurrent oral
ulcers (minor canker sores, major canker sores or herpetiform
ulcers, in oral mucosa with a minimum of 3 episodes for a year).
Minor criteria: recurrent genital ulcers (ulcers or aphthous scars in
genital areas observed by the doctor or the patient) (2 points). Eye
lesions (anterior or posterior uveitis, or the presence of vitreous
cells in the examination with slit lamp or vasculitis retinal diagnosis
by an ophthalmologist) (1point).
Skin lesions (erythema nodosum, folliculitis, papulopustular
lesions, acneiform nodules, observed by the doctor in postadolescent
patients not treated with corticosteroids) (2 points).
Patergia test: positive (cutaneous hypersensitivity characterized by
the appearance of a sterile pustule, 24 to 48 h after needle puncture,
observed by a doctor) (1 point). Vascular lesions (arterial, venous
thrombosis or aneurysms) (1 point). The diagnosis is made with the
mandatory criterion plus 3 points [10]. In 2013, an international
group, composed of representatives from 27 countries, reviewed
the international criteria, according to these criteria, a patient
with a score ≥ 4 points is classified as a Behcet disease [3]. The
presence of recurrent, painful, variable-sized canker sores that
heal in 1-3 weeks usually without scarring in most cases are the
first manifestation, as occurred in this case. The genital canker
sores present in 72-94% of cases are morphologically similar to
oral ones, usually heal at 2-4 weeks, but they do leave a scar [7].
There are no typical laboratory alterations of Behcet Syndrome.
Erythrosedimentation and C-reactive protein levels are often
moderately high but do not correlate well with disease activity, in
this case these values were kept within normal parameters.
Acute phase reactants may be elevated, mainly in patients with
vasculitis of large vessels. Serum immunoglobulins are sometimes
elevated and immunocomplex levels may be elevated, but
autoantibodies such as rheumatoid factor, antinuclear antibodies,
anticardiolipin and neutrophil antithoplasm (ANCA) are negative [3].
The patergia test is not 100% specific, only a proportion of patients
with Behcet Syndrome have a positive response and the positivity
in patients with the syndrome vary in different geographical areas
(60-70% in Turkey and Japan, but rare in America and Europe)
[11], however, the case presented is of a patient born in Cuba who
is part of the American continent in which the test was positive,
not coinciding with world statistics, where positivity is rare in the
Americas. The differential diagnosis should be made with: Reiter’s
disease, Steven-Johnson syndrome, aphthous stomatitis, recurrent
Mollaret meningitis, Whipple’s disease, multiple sclerosis, Harada’s
disease, inflammatory bowel diseases, sarcoidosis and ankylosing
spondylitis. The diagnosis is based on detailed medical history and
long-term clinical observation. There is no way to predict whether
a patient with recurrent oral ulcerations will develop the disease
even if frequent outbreaks constitute an alarm sign, as confirmed
in this case. The choice of treatment depends on the clinical
manifestations and their severity.
An early diagnosis followed by a treatment with corticosteroids,
medication used in this patient, could prevent the fearful
neurological complications in the opinion of several authors,
although more recent studies report highly positive results with
immunosuppressants [7]. It is described that all patients should
use colchicine and steroids, with Metrotexate being the diseasemodifying
drug most used in the treatment of this [5]. The majority
of patients diagnosed with Behcet syndrome have a productive life.
The symptoms are controlled with a healthy diet, rest, physical
exercises and drug treatment and the prognosis varies according to
the affected organs [7]. Behcet’s disease has a chronic course with
exacerbations and unpredictable remissions, the frequency and
severity of which may decrease over time. After the first five years,
the disease acquires a stable course or towards improvement;
after the fourth decade, clinical severity is decreased, with longer
intervals of recurrence between exacerbations. The prognosis is
good, unless there is commitment of vital organs. The presentation
at the age of early onset (before age 25) has been associated with
more severe manifestations of the disease and increased mortality
[13].
Conclusion
While it is true that multiple systemic diseases present with aphthous oral manifestations, oral ulcers in Behcet’s disease are the first clinical manifestation, which in most cases, lead the patient to seek medical help and constitute for countless authors the cornerstone to reach the diagnosis of this disease, so it is considered vital that the Comprehensive General Stomatologist putting into practice the knowledge acquired about the syndrome, consider it a possible differential diagnosis more before a patient with recurrent oral ulcerations. The timely management of a patient with an unusual and exceptional pathology can have an optimal evolution and reduction of complications in the quality of life. It is recommended to expand coverage and health education to be able to detect these cases in the first instance, thus avoiding underdiagnosis.
For more
Articles on : https://biomedres01.blogspot.com/




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.