Type 2 Diabetes Mellitus and COVID-19 in Mexico. A comprehensive Assessment
Introduction
On February 11, 2020, the International Committee for
Taxonomy in Viruses named SARS-CoV-2. Composed of a genome
of 30,000 base pairs, belonging to the Coronaviridae family of the
order Nidovirales. Phylogenetically coronaviruses are classified
into alpha, beta, gamma and delta. Coronaviruses were identified
50 years ago as pathogens responsible for the common cold, mainly
HCoV-OC43, HCoV-229E among other variants. At the beginning
of 2002, coronaviruses were considered exclusively veterinary
pathogens, however, by 2019 they were identified in biological
samples from patients diagnosed with pneumonia [1-4]. Showing
an age trend initially with geriatric patients, it has been shown that
the risk of mortality increases after 75 years [5]. However, today
age is no longer a dependent factor for infection. It is important
to mention this since it may be due to multiple etiologies in
addition to infection, such as: comorbidities, lack of metabolic
control, suspension of work in the outpatient clinic due to hospital
oversaturation derived from the pandemic, sedentary lifestyle,
among others.
Hence it is important to emphasize the lack of metabolic control
derived from all those cardiometabolic diseases, such as: obesity,
hypertension, dyslipidemias and mainly diabetes mellitus, which
turns out to be the first pandemic that has not been adequately
controlled since ancient times [6]. All these factors are directly and
proportionally related to the risk of severe progression and poor
prognosis due to the chronic inflammatory state that generate more
the acute systemic inflammatory response derived from COVID-19.
In the case of obesity, another factor shared by both pathologies
increased even more derived from confinement due to the forced
closure of sports centers, favoring a sedentary lifestyle. The anxiety
derived from the pandemic favors a greater consumption of foods
with low nutritional power, again favoring obesity and lack of
metabolic control. Therefore, in the context of a controlled diabetic
patient, the measures that had to be implemented as a strategy
to reduce the rate of infections are one of the factors to generate
lack of control. The percentage of uncontrolled diabetics since
the beginning of the pandemic is more and more common and continues to rise, which entails greater spending on health, greater
generation of medical supplies and resources. There is an excess of
mortality in the Mexican Republic derived from the pandemic, not
only due to COVID-19, but also due to other causes [7,8] without
forgetting to mention the possibility of under- registration that
exists, for example, in marginalized areas or those who could not
have hospital access derived from the same scenario. That is why
the relevance of this article where a comprehensive scenario is
proposed for the knowledge and management of COVID-19 in
those patients who already have a chronic damage such as Diabetes
Mellitus.
Pathophysiology
The incubation period for SARS-CoV-2 is 5 days with a range of
2 to 14 days [9]. The spectrum of diseases generated by coronavirus
infection is mainly acute respiratory, chronic, enteric, hematological,
endothelial and of the central nervous system. The mechanism of
transmission of the disease by SARS-CoV-2 is from person to person
through the airway by the drops of Flügge that are exhaled when
coughing, sneezing or speaking and are inhaled or deposited in
the mouth and ocular conjunctiva, as well as surfaces, which can
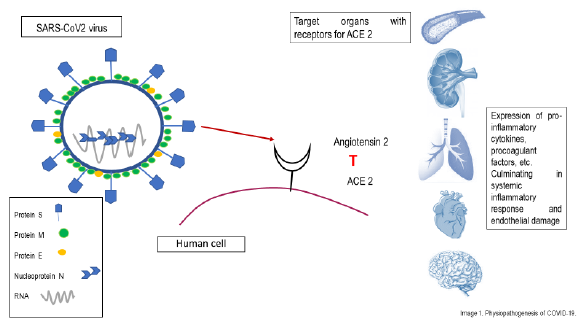
function as fomites [10]. The main structural proteins found on the
membrane surface of the SARS-CoV-2 viral particles participate
within the pathophysiology, which are: Spike (S), membrane (M)
and envelope (E). Among other, these are responsible for the
anchorage and entry of these microorganisms to the host’s cells.
It should be noted the type 2 angiotensin converting enzyme (ACE
2) which is a type I membrane protein that contains receptors in
the lung, heart, kidney and intestine, endothelium, nervous system,
mainly. The ACE 2 receptors that are located in the lower respiratory
tract of humans are the cellular receptors for SARS CoV-2. Since
the virion has the S-glycoprotein or Spike protein, which projects
through the viral envelope and forms the spicules of the crown, this
is glycosylated and is responsible for mediating the binding of the
receptor (protein S + ACE 2), as well as its fusion with the host cell
[11,12].
This strong bond unites the entire SARS-CoV-2 membrane
with the host cell membrane, entering it through endocytosis. Viral
particles release their RNA that binds to viral DNA, initiating the
viral replication cycle, which leave the host cell through exocytosis.
Once the RNA of the SARS-CoV-2 particles begins its translation
and transcription, two processes are generated: the first related to
the high demand for manufacturing viral proteins causing cellular
stress that ends in apoptosis of the target cells; while in the second,
the viral RNA acts in a molecular pattern associated with pathogens,
which leads it to be recognized by the cells of the immune system,
initiating the activation of the cytokine cascade and the migration
of neutrophils. Hypercoagulability, venous stasis and endothelial
damage is another of the main characteristics mediated by the ACE
2 receptors that SARS-CoV-2 particles possess, being observed in
the endothelium of the veins, arteries and arterial smooth muscle
cells of the brain; This produces dysfunction and inflammation of
the microvasculature that alters vascular flow and initiates platelet
activation, increasing risk for macrovascular and microvascular
thrombosis, pulmonary thromboembolism, deep vein thrombosis,
catheter-related thrombosis, ischemic cerebrovascular disease,
acrosyndromes, and capillary leak syndrome. in organs such as
lungs, kidneys and heart, increasing mortality, one of the main
complications [13] (Figure 1).
SARS-COV2 as a Diabetogenic Agent
Diabetes is associated with a chronic low-grade inflammatory
state that favors the development of an exaggerated and constant
inflammatory response. At the molecular level, there is an increase
in the levels of IL-6 and C-reactive protein (CRP), so the proinflammatory
state typical of diabetes can favor the cytokine storm
and the systemic inflammatory response that accompanies the acute
respiratory distress syndrome (ARDS) in patients with COVID 19
[14]. This is why diabetics infected with SARS-CoV-2 have a higher
rate of hospital admission, severe pneumonia, and higher mortality
compared to non-diabetic subjects [15]. SARS-CoV-2 is considered
diabetogenic since it is also capable of causing direct damage to the
pancreas, due to the expression of ACE 2 (mainly in islet cells) even
in a higher proportion than at the lung level, which could worsen
hyperglycemia and even induce the onset of diabetes in previously
non- diabetic subjects [16]. It should be noted that only 1-2% of
patients with mild COVID-19 infection present pancreatic lesions,
while 17% of patients with severe cases present with lesions of
the pancreas, which can accentuate the systemic inflammatory
response and, therefore, Therefore, accelerate the appearance of
ARDS [17]. On the other hand, the current scenario of the pandemic
even in uninfected subjects may favor the deterioration of metabolic
control due to difficulties in accessing the health system, lack of
physical activity and increased stress associated with confinement.
Therapeutic strategies should be aimed at facilitating access
to the health system through telemedicine to advise the patient
on the adaptation of treatment or any other remotely manageable
medical situation and guide patients and caregivers in the control of
diabetes in order to prevent hospitalization [18]. Clinical symptoms.
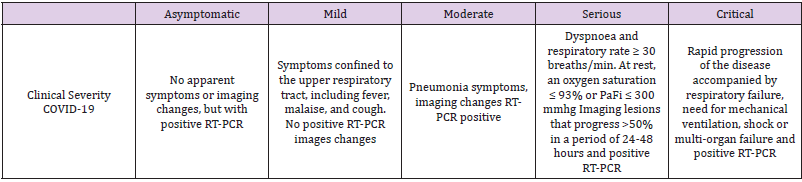
Different stages of SARS-CoV-2 disease have been described in
humans depending on the clinical severity, which can range from
mild symptoms such as: fever, myalgia, headache, cough, anosmia.
Up to severe symptoms characteristic of pneumonia with severe
respiratory impairment [19,20-25]. Table 1 Mild and moderate
infections comprise 80.9% of the registered cases; the severe ones,
13.8% and the critical ones, 4.7%. In the adult population it is 1.2%;
while in pediatric population it is 15.8% [26]. The prevalence of
asymptomatic patients differs according to the age group and
can be reported by up to 40% [27]. Due to the high percentage of
asymptomatic patients not only in Mexico, but also worldwide, it is
vitally important to continue using a facial mask in our daily lives
in order to reduce the risk of contagion. Even people with a full
vaccination schedule are not exempt from COVID-19 infection.
Prognostic factors for serious and severe disease are
considered: cardiovascular disease, diabetes mellitus, hypertension,
chronic lung disease, cerebrovascular disease, cancer, chronic
kidney disease, obesity and smoking [28,29]. Some alterations in
laboratory parameters associated with a pro-inflammatory and
procoagulant state are indicative of a poor prognosis, such as multiorgan
failure [30]:
• Lymphopenia.
• Elevated liver enzymes.
• Elevated LDH.
• Elevation of acute inflammation markers (CRP, ferritin,
procalcitonin).
• D-dimer elevation.
• Prothrombin time lengthening.
• Elevation of troponins.
• CPK elevation.
• Markers of kidney damage (elevated creatinine, anuria).
Diagnosis. There are different detection techniques for SARSCoV-
2, each with different sensitivity and specificity. We currently
have three types of diagnostic tests [17,18]:
a) Nucleic acid detection tests (PCR). In the case of the gold
standard. Being its high cost the main limitation for its
application.
b) Antigen (Ag) detection tests.
c) Antibody detection tests (Ab): IgM / A and IgG.
We must emphasize that a negative result does not exclude
infection, therefore, if the clinical suspicion is high (clinical data,
epidemiological context, radiological findings, sometimes earlier
in computed tomography than the positivity of the PCR and
analytical studies), it is recommends repeating the same sample in
48-72 hours or trying to obtain it from the lower respiratory tract,
especially in severe or progressive disease [16]. Throughout the
pandemic, a high percentage of false negatives has been observed
in the practice of antigenic tests, the most used in Mexico due to
the difference in cost between PCR, which has perpetuated in the
patient the uncertainty of being or not with the infection, which
means that they do not follow the medical indications and finally
contribute to continue perpetuating the contagion. Educating the
patient about what a negative result implies despite high clinical
suspicion is part of our work in this pandemic and therefore,
as health professionals, we should not base our treatment on
a laboratory test and the recommended measures should be
initiated in the context of isolation, symptomatic treatment and
continuous monitoring of associated comorbidities in order to
avoid complications as explained in detail.
Treatment of diabetes mellitus in patients with COVID-19.
Treatment depends on the clinical characteristics of each patient,
risk of complications, age, ease of access to the health area,
socioeconomic status, risk of drug interactions especially in patients
with polypharmacy, etc. Treatment for COVID-19 infection should
be symptomatic, that is, based on the clinical picture presented by
each patient, which can be: antihistamines, cough suppressants,
thromboprophylaxis, analgesics and anti-inflammatories, educate
for self-monitoring of vital signs and provide all the necessary alarm
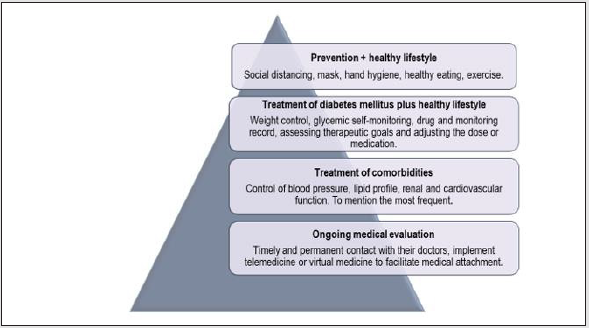
data. As outpatient management in non-serious patients and mild
symptoms, the following should be taken into account: prevention
of infection, healthy lifestyle, general measures to improve diabetes
control, treatment of hyperglycemia, treatment of comorbidities
and support doctor (Figure 2). For the treatment of asymptomatic
or non-severe patients, the following is recommended: home
management, follow usual treatment for diabetes control, goal of
fasting glucose 70-130 mg / dL, HbA1c <6.5%, use of telemedicine
to clarify doubts and education, indicate alarm and isolation
measures, adjust the medication only if there is lack of control.
Speaking of telemedicine, Mexico is not fully prepared, since
it has a technological development of around 25%, however,
thanks to portable technology such as a cell phone that facilitates
the use of telemedicine, it can favor the medical attachment of
chronic degenerative diseases and likewise surveillance of the
clinical evolution of COVID-19 in those patients with a high risk
of complications. Up to 70% of the population could benefit from
these programs [22,24,30].
Image 2: Measures to be implemented in diabetic patients with COVID-19 taken with modified from M.M. Lima-Martínez et al.
In the case of patients with mild-moderate infection: home management with close monitoring, assess risk of progression and assess the need for in-hospital management, medication adjustments according to glycemic control, fasting blood glucose target of 72-144 mg / dL, HbA1c <7%, close medical contact. For those with severecritical infection: use insulin in continuous intravenous infusion or basal-bolus-correction regimen, fasting glycemic goal of 72-180 mg / dL, HbA1c <8%, strict monitoring of plasma glucose, electrolytes, ketone bodies, renal and cardiovascular function, procoagulant markers among others. Always in-hospital (22,30). (Figure 3). With the above mentioned, the need for extra medication should be taken into account depending on the symptoms of COVID-19 according to the evidence reported so far. It is intended to exemplify the treatment of these two entities together, since if we only dedicate ourselves to treating the patient based exclusively on the diagnosis of COVID-19, forgetting about their underlying pathology, in this case diabetes mellitus, we increase the risk of complications and mortality. Special considerations for drugs for diabetes mellitus in COVID-19 should be taken into account, such as: Metformin, SGLT2-i, GLP-1 analogs, DPP-4 inhibitors, sulfonylureas, and insulin. Each one with specific indications, making the appropriate dose adjustments according to the patient’s needs, to optimize therapeutic goals, but it is important to emphasize that for those who require hospitalization derived from COVID-19, the drug of choice for glycemic control will be insulin [22].
Image 3: Indication in the management of covid 19 according to the clinical severity of diabetic patients. Takane and modified from M.M. Lime Martinez, et al. & Medina – Chavez JH, et al.
In diabetics hospitalized for COVID-19, the use of prophylactic doses of low molecular weight heparin, such as Enoxaparin, is suggested in the absence of contraindications (active bleeding or platelet count <25 × 109 / l, and others), with dose adjustment for patients with frank elevation of D-dimer and those that present severity criteria [15]. It is important to individualize the prothrombotic risk according to the age and associated comorbidities of each patient, even in patients with mild symptoms thromboprophylaxis is indicated, the duration of this measure will also depend on how many associated risk factors present and the clinical severity, which requires a minimum of 2 weeks in those asymptomatic or mild symptoms and up to 6 weeks in severe conditions. Even with the resolution of the symptoms and / or the hospital discharged, this measure must continue for a minimum of 7 days [30].
Conclusions
The union of protein S with ACE 2 is the most important point
within the pathophysiology since it culminates in a systemic
inflammatory response and endothelial damage, which opens the
door for a wide panorama of complications in the organism, even
that a patient debut as diabetic from infection. At the beginning
of 2020, when the first case of COVID-19 was registered, to date,
the Mexican population presents data of exhaustion derived from
isolation. Despite this, the vaccination program that was established
in Mexico has not been fast enough, placing itself practically in the
last place in Latin America for complete coverage of vaccines and
reducing the rate of infections to be able to restore daily activities in
a greater proportion and better still reduce morbidity and mortality
in vulnerable groups. In addition to this, the lack of supplies and
medical personnel in the health sector remains constant, which does
not favor the scenario of both pandemics since it also worsens the
medical adherence required by patients with chronic degenerative
diseases, leading to a greater risk of complications, greater risk of
contagion and finally higher mortality; thus, generating a vicious
circle. Offering a broad panorama as a comprehensive evaluation of
what COVID-19 implies in a patient with Diabetes Mellitus offers us
new opportunities to reduce complications and serious progression
of the disease, emphasizing the need to establish strategies such as
telemedicine if necessary for better medical surveillance, promote
pharmacological adherence and provide timely help in case of
seriousness, always treating together.
We are in a century where two pandemics converge with
each other, increasingly diabetic patients with lack of metabolic
control, generating catastrophic damage to health, psychosocial
and the economy. It is necessary to control both, starting with
preventive measures to be able to modify the impact that has been
generated so far. The points to follow in the context of DM2 and
COVID-19 will be prevention measures where isolation is the most
important, educating the patient, surveillance of comorbidities
and glucose self-monitoring to be able to adjust the dose or change
the medication in case of lack of control, monitor alarm signs and
offer symptomatic treatment according to the needs of the patient,
without forgetting the necessary use of telemedicine as a support
tool.
For more
Articles on : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.