Analysis of Disease Patterns and Treatment Results of COVID 19 Patients Through Data Analysis of COVID 19 Patients at Seoul Metropolitan Seobuk Hospital
Research Article
Introduction
Seoul Metropolitan Seobuk Hospital is a hospital which is directly managed by the Seoul Metropolitan Government and has mainly been used for homeless people and tuberculosis patients. It is a public hospital providing primarily inpatient and outpatient treatment for the elderly and for vulnerable people groups including the homeless and the disabled. From March 2, 2020, on, Seoul Metropolitan Seobuk Hospital was designated for the treatment of COVID 19 infectious diseases and has continuously treated COVID 19 inpatients until now, August 2021. At the beginning of the pandemic, in February 2020, there were few confirmed cases of COVID 19 in South Korea but now, as of August 27th, 2021, the total cumulative number of confirmed cases in South Korea is 245,158 and the death toll is 2.265. Recently, the number of confirmed cases in the Seoul and Gyeonggi-do region has been accounting for about 60% of the nation’s total cases. During the last 50days the number of daily confirmed cases has surpassed than 1,500 [1,2].
In our Korean quarantine system, once a person has a confirmed positive COVID 19 test, they are transferred to one of the designated hospitals for infectious diseases or a life treatment Center within the shortest time possible. If they are over 60 years old or are younger but already have an existing medical condition, they will be transferred to an infectious disease hospital. If they are under 60 and they have no underlying diseases, they are transferred to a life treatment center first. If they develop any severe symptoms while staying at a life treatment center, they are transferred to one of the infectious disease hospitals. As of today, 20th of August 2021 there are 7 Seoul city governmental hospitals and 9 other hospitals which are designated as COVID 19 hospitals in Seoul city and Gyeonggi -do area. 2,002 patients are hospitalized in these infectious disease hospitals according to the protocol of the quarantine system. As of August 20th, 2021, there are 15 life treatment facilities operating in Seoul city and Gyeonggi –do area with a current number of 1,878 COVID 19 patients quarantined according to the quarantine system [3-5].
If their symptoms worsen or their oxygen saturation drops, they can be transferred to an infectious disease hospital for hospitalization. COVID 19 patients who are young children, disabled or otherwise in need of nursing care by a family member, will sometimes be hospitalized together with them, despite the risk for the care giver to contract the virus as well. In rare cases the patients can be quarantined in their own home according to their wishes. All COVID 19 patients are assigned an epidemiological investigator who will guide them in all these decision processes. From March 2, 2020, to August 20, 2021, the total number of 2,315 confirmed COVID 19 patients has been admitted to Seobuk Metropolitan Hospital while the number of discharged patients was 2,215. During the last two months, the number of daily confirmed cases has been over 1,500 and we continue to treat many patients, daily filling the available hospital beds [5-10].
In Republic of Korea, the COVID 19 virus vaccine was first administered in early 2021 to the elderly and to vulnerable patients (including patients in nursing homes for homeless and disabled people), as well as to hospital and other government quarantine facilities staffs. The number of COVID 19 patients under the age of 60 who are not yet fully vaccinated has increased compared to the age pattern of patients we had in 2020. In fact, it was expected that the course of the COVID 19 disease would differ, depending on age and pre-existing medical conditions, but this is not necessarily the case. Young patients with no pre-existing disease and in otherwise good health, can have a COVID 19 disease pattern that is often rapid and very severe. We observed many cases of elderly patients with multiple chronic diseases who overcame the disease called COVID 19 well and without any major complications and sequelae.
In this paper, using the data from March 2, 2020 to May 25, 2021 of the 1,523 patients hospitalized in Seobuk Metropolitan Hospital, we analyze the data according to diagnosed diseases, diseases diagnosed by clinical features during the time of hospitalization, the patients’ past history and current medication We describe the existing and past diseases as well as the COVID 19-related diseases of the COVID 19 patients who were admitted to the hospital. By summarizing the treatments and treatment results, including the therapeutic medications administered, we would like to share and suggest ways to understand the COVID 19 diseases and how to deal with them.
Materials and Methods
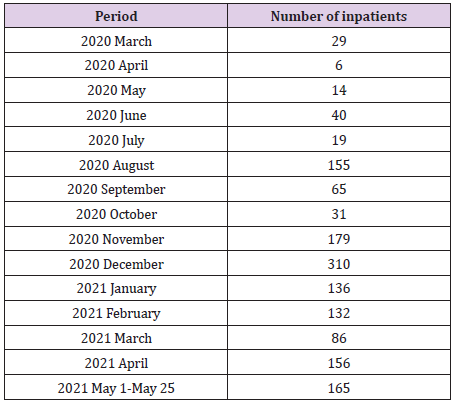
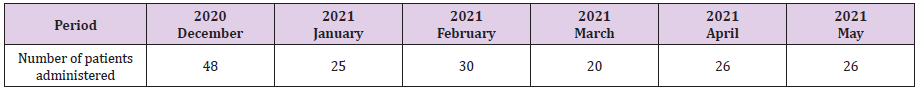
Seobuk Metropolitan Hospital is as city governmental hospital in Seoul. It was one of the first hospitals to become a COVID 19-dedicated hospital among various national and public hospitals in Seoul in March 2020. From March 2020 to August 2020, one or two wards were operated as COVID 19 beds units, usually accommodating between 30 and 50 patients per month, as at that time the number of COVID 19 patients in Seoul city and Gyeonggi –do area was quite low. However, since August 2020 up to now, we are running 7-8 wards with more than 150 patients a day. In Seobuk Metropolitan hospital, COVID 19 patients are cared for by 12-14 specialists from different departments (internal medicine, general surgery, family medicine, psychiatry, neurology, thoracic surgery, pediatrics, etc.). As soon as COVID 19 inpatients are diagnosed through a COVID 19 test, inpatient treatment at an infectious disease hospital or isolation treatment at a life treatment center will be maintained for an average of 7-14, after which, being released from isolation, patients are allowed to return to their daily life.
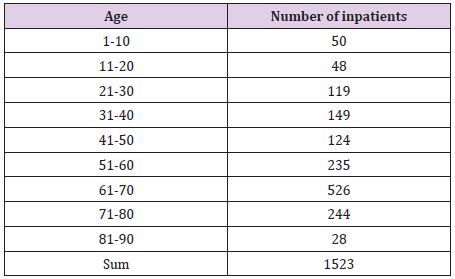
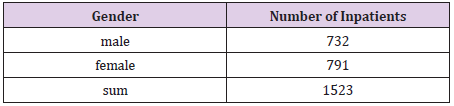
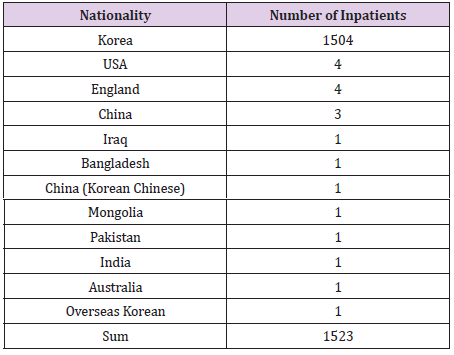
All treatment and living costs are fully covered by the government during the patients’ stay at an infectious disease hospital or a life treatment center. As long as the COVID 19 test is positive, COVID 19 patients stay there free of charge. In other countries, including the United States, most patients are usually admitted to hospital and receive treatment when their disease reaches a more severe status or they are in need of oxygen therapy or even a ventilator., In Republic of Korea, however, the quarantine system has been and continues to operate in such a way that isolation and treatment begin at a living treatment center or a hospital dedicated to COVID 19 within 1-2 days from the moment of a positive COVID 19 test result. In this paper, we analyze the charts of 1,523 patients who received inpatient treatment from March 2, 2020, to May 25, 2021, at our hospital dedicated to COVID 19 infectious diseases. The monthly number of hospitalized COVID 19 patients (Table 1), the age status (Table 2), the gender status (Table 3), and the nationality of the patients (Table 4) will be explained in the materials and method.
Results
In this article, we would like to talk about the disease patterns of hospitalized COVID 19 patients. The tables below show a classification of pre-existing diseases the patients had before contracting the virus. as well as those diagnosed during hospitalization. In addition, we also discuss whether there is a difference between the clinical picture of COVID 19 itself and the clinical picture due to accompanying diseases. We also examine how oxygen therapy has been implemented and how many patients developed pneumonia during inpatient period. The tables show the presence of pneumonia as well as the use of oxygen treatment among COVID 19 patients. The purpose of this study is also to analyze the data on the use of therapeutic agents during the patients’ hospitalization period.
Comorbidity of COVID 19 Patients
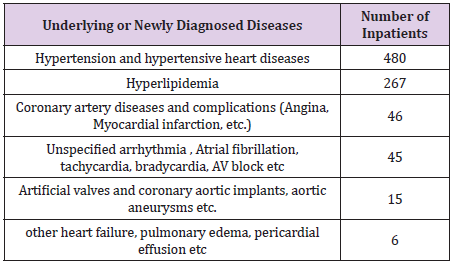
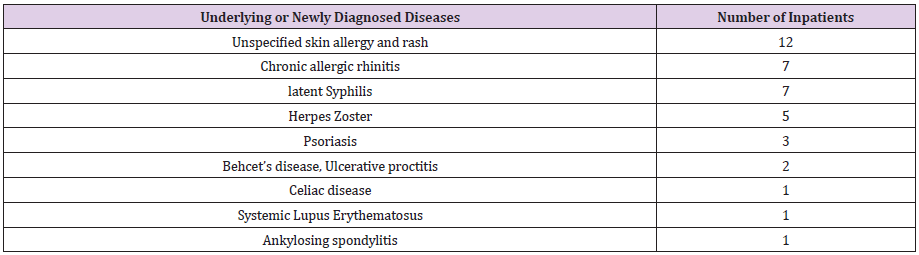
The purpose of this study is to investigate the comorbidities according to systemic classification by analyzing the data of the existing comorbidities of inpatients and their diseases diagnosed at the time of hospitalization. The purpose of this study is to explain the disease pattern of the COVID 19 itself by looking at the accompanying diseases of the patients as well as at newly diagnosed diseases. Table 5 to 12 summarize the diagnoses according to systemic classifications of the 1,523 patients hospitalized from March 2, 2020, to May 25, 2021, according to their underlying or newly diagnosed diseases during their hospitalization period. The most common underlying cardiovascular diseases were hypertension, hyperlipidemia, coronary artery disease, arrhythmia, and artificial valves or implants. Many patients with a prior coronary artery implant, suffered from high blood pressure and increased pulse rate due to COVID 19 infection status. The COVID 19 disease itself increases the association between the onset of cardiovascular diseases and blood clots, as well as the frequency of overall cardiovascular diseases, and creates many situations that require medication.
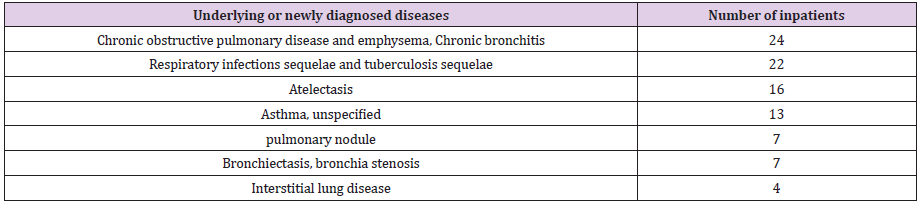
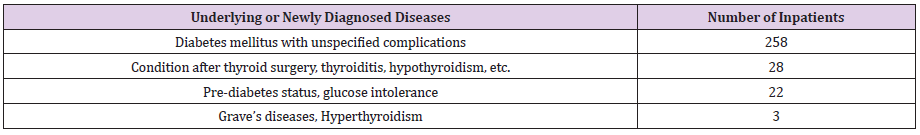
In most cases, the patients were instructed to continue with their medication even after being discharged and to conduct a follow-up examination. As an accompanying underlying disease, respiratory diseases such as chronic obstructive pulmonary disease, emphysema, sequelae of tuberculosis, asthma, and bronchiectasis were common. For all patients hospitalized for COVID 19, chest CT scans are conducted to check the progress of the disease and to detect any underlying lung disease. In some cases, the follow up examination after discharge confirms a resolved pneumonia or lung lesions. Diabetes mellitus is the most common endocrine accompanying underlying disease. Many patients are hospitalized and diagnosed with diabetes. COVID 19 disease itself can be seen as an extremely stressful situation, which in itself can easily provoke the development of diabetes. In addition, the treatment for the COVID 19 disease itself (Dexamethasone using) caused increased blood sugar during the course of treatment.
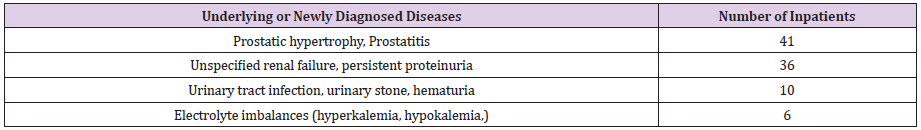
Patients need to receive long-term diabetes or glucose intolerance status follow-up after their discharge from hospital. As an accompanying underlying disease, there are several with chronic renal failure who continued medication. Usually, the COVID 19 disease itself generally caused persistent high fever, difficulty in ingesting food and water. Very severe dehydration problems occur frequently to COVID 19 patients, these dehydration problems can damage kidney function. Many treatments such as electrolyte correction and dehydration correction are required. In patients with such pre-existing, well controlled chronic diseases, sometimes symptoms similar to their own disease develop. We saw both the original underlying disease flaring up as well as the appearance of new skin rashes occurring during hospitalization due to COVID 19. In many cases, patients’ reactions to the COVID 19virus itself are also perceived as individual allergies or anaphylaxis-like reactions. These symptoms usually disappear as patients recover from COVID 19 virus.
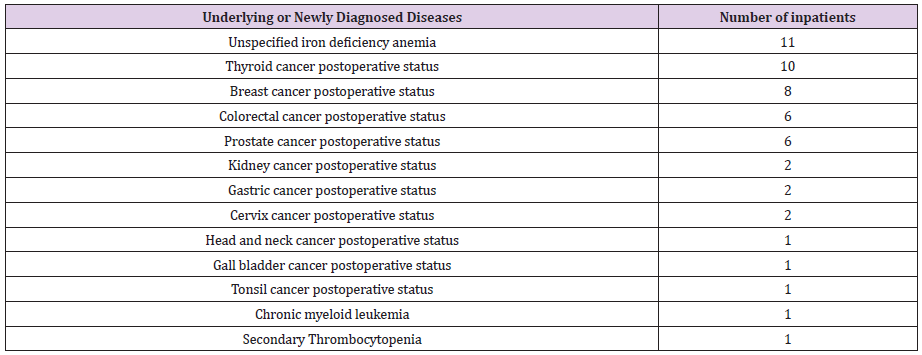
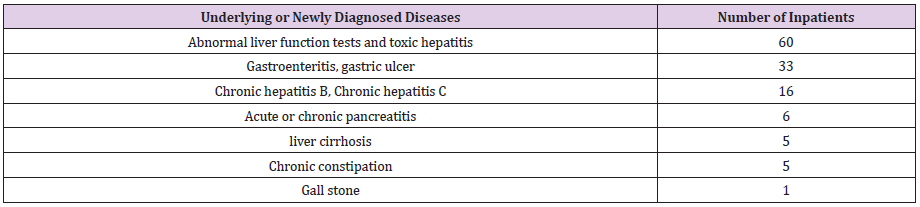
We didn’t find any special complications for patients who had completed surgery and chemotherapy 2-3 years prior to contracting the COVID 19 virus. However, as for any other patient, the amplified viral load, high fever and prolonged severe inflammation, causes a temporary thrombocytopenia and a decrease in the count of neutrophils along with the sepsis. These parameters return to normal as the patient recovers from COVID 19. An elevated liver function is the commonly diagnosed pathology during hospitalization indicating the accompanying underlying disease of a toxic hepatitis due to the COVID 19 virus. Patients who confirmed that their liver function tests were normal before admission as well as patients with existing chronic diseases such as hepatitis B, hepatitis C, and cirrhosis whose liver function levels were maintained at near normal levels before the outbreak of COVID 19, experience a rise in the liver function parameters which can be attributed to the COVID 19 infection. The most common digestive symptoms during hospitalization were diarrhea, nausea and vomiting.
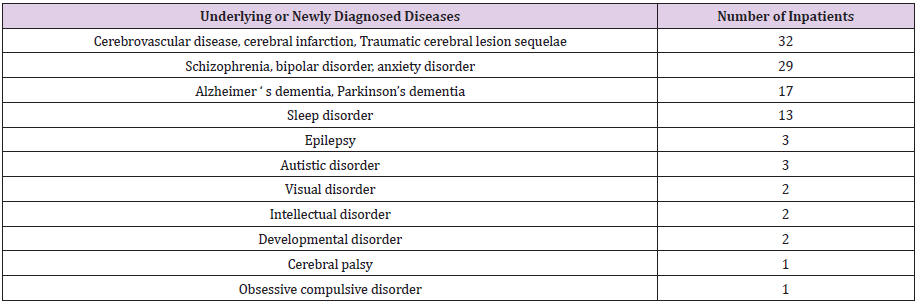
Patients with cerebrovascular disease and psychiatric disease as underlying diseases were suffer from long term chronic disease and have to be hospitalized together with the caregiver family member due to their paralysis or disability. The process of isolation and communication with the bedridden patients and psychiatric patients is very challenging and difficult due to their psychiatric problems and disabilities, but we do not think that the underlying diseases had much influence on the diagnosis, clinical picture, and medication process of COVID 19 disease (Tables 6-19).
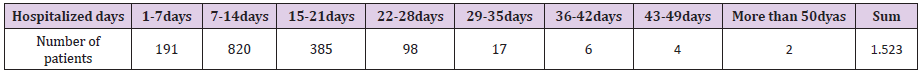
Table 18: Current status of the number of patients by hospital stay of the 1,523 hospitalized patients.
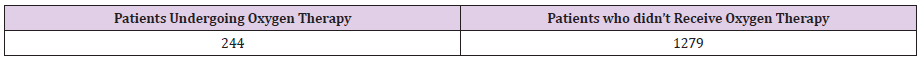
Oxygen Treatment for COVID 19 Patients
We would like to talk about oxygen therapy for COVID 19 patients. Patients admitted to the hospital and are given a selfsaturation check machine to check and record their saturation several times a day. When the oxygen saturation in room air is less than 94%, oxygen therapy is given. Oxygen is sometimes used intermittently for chest tightness. 244 patients used oxygen for 1 to 2 weeks during hospitalization, and 1,279 patients did not receive any oxygen treatment. When oxygen is used, oxygen saturation can be maintained over 94% . As the pneumonia improves, oxygen demand also decreases. If oxygen demand increases more, we use high flow O2 machine. If the oxygen saturation cannot be maintained over 95 % by using a reservoir mask of 5L/min because of high oxygen demand, we use a high flow O2 machine to increase the O2 supply. If the oxygen saturation cannot be maintained over 95 % by using a high flow O2 machine at its highest level, the COVID 19 patients should be transferred to a university hospital for ventilator and ECMO therapy.
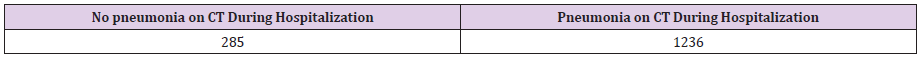
As the COVID 19 pneumonia improves, oxygen demand also decreases, and oxygen tapering becomes possible. Usually, patients are discharged when their oxygen saturation is higher than 95 % without oxygen therapy. As a result of a chest CT scan for all 1,523 COVID 19 patients hospitalized from March 2, 2020, to May 25, 2021, pneumonia was found in 1,238 patients while 285 did not have any. A chest CT will usually confirm the increase or decrease of the pneumonia. The COVID 19 patients who were hospitalized from early March 2020 to July 2020 were usually young and came from abroad. Many of them did not have severe symptoms. General treatments (analgesic, antipyretic, antibiotic, antihistamine, fluid therapy, etc.) used to treat common respiratory infections (bacteria, virus) were implemented.
Therapeutic Agents for COVID 19 Patients
The purpose of this study is to analyze the data on the use of therapeutic agents during the hospitalization period of patients. In addition, we intend to analyze the interaction or effect of antiviral drugs and antibody therapeutics as a treatment for COVID 19 virus. By analyzing the data related to the use of drugs by COVID 19 patients and the data related to the results of the treatment, we would like to examine the effects of the drugs that are clinically judged to have an impact on the treatment of the disease called COVID 19. We used Kaletra, which is an antiviral drug used in AIDS treatment on 686 COVID 19 virus patients between March 2020 and April 2021. Many patients discontinued this treatment halfway through because of its difficult side effects such as diarrhea. At that time, we believed that, in the absence of a special antiviral drug, Kaletra would reduce the viral load, but we finally came to the conclusion that it did not help much. We are looking back at this time as a time to observe the disease pattern of COVID 19.
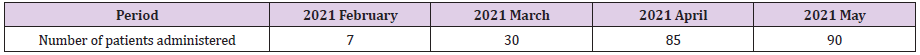
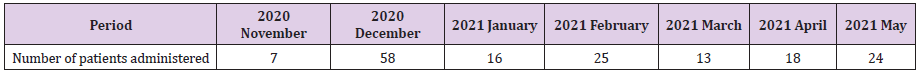
From August 2020 on, many elderlies, medically chronic patients, and patients with worsening symptoms were hospitalized in Republic of Korea and other drugs were recommended as treatments. In August 2020, many COVID 19 patients where in need of other antiviral drugs. In November 2020 we started to administer the antiviral agent Veklury (Remdesivir)as well as steroids, including Dexamethasone injections. In March 2021, we began with the administration of the monoclonal antibody treatment Regdanvimab (Regkirona). In case of pneumonia with a maintained oxygen saturation at more than 95% in room air, and symptoms occurring within 7 days, the monoclonal antibody treatment Regdanvimab (Regkirona) is the preferential treatment. In case of pneumonia and the oxygen saturation falling below 94% in room air, we start oxygen therapy and also directly use Veklury (Remdesivir) as an antiviral agent for 5 days together with a Dexamethasone injection 1.2 mg.
The dose of Dexamethasone is gradually decreased within 10days. However, in order to prevent the progression of pneumonia, monoclonal antibody therapy and antibiotics are used together. If pneumonia was severe and saturation is lower than 94 %, we use antiviral agents first. It usually takes one or two weeks for the pneumonia to improve, and the oxygen saturation restored to normal level.
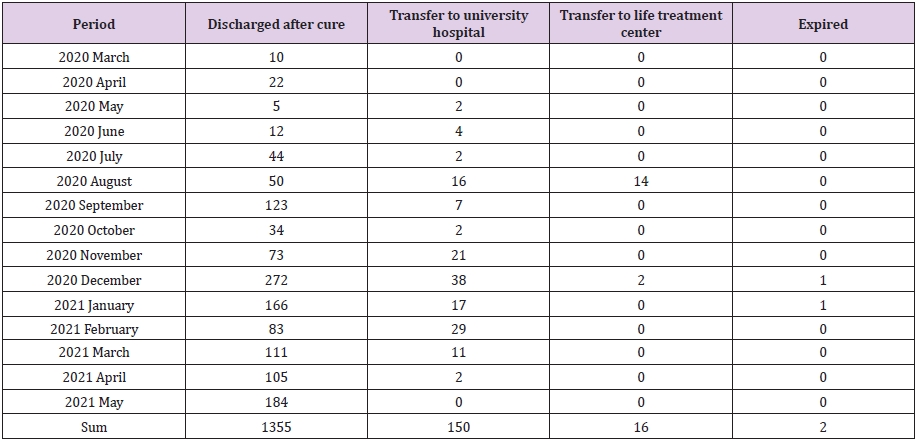
Treatment Progress of Inpatients
According to the data summarized through the chart of 1,523 COVID 19 patients hospitalized from March 2020 to May 2021, we see that for the majority of patients the time of hospitalization was usually between two and three weeks. Of the total 1,523 patients, 1,355 were discharged home after being cured, 16 patients were transferred to a life treatment center due to constrains of the hospital beds as it was too early to release them from quarantine, although there was no severe problem with the COVID 19 disease itself. 150 out of the total of 1,523 patients, almost 10% of the patients, needed to be transferred to a university hospital because of the severe progression of their pneumonia. One mortality case in our hospital was a 74-year-old female dementia patient who died with no CPR and only full high flow O2 therapy, Veklury (Remdesivir) treatment and general treatments by her husband’s agreement. Another 60-year-old female patient died in the hospital restroom by removing the oxygen therapy for a long time by herself.
Discussion
Severe Acute Respiratory Syndrome COVID 19virus 2 (SARSCoV- 2) is a positive-stranded RNA virus with an envelope that is 80% or more similar in RNA sequence to bat COVID 19virus. There is a strong theory that it may have acted as an intermediary. Human-to-human transmission is assumed to be the primary route of infection, but a number of research results suggesting the possibility of airborne transmission have been published recently. It is known that infection with SARSCov-2 is most contagious just before the onset of symptoms and in the early stages of the disease, and the infectivity is weakened 5 days after the onset of symptoms. In general, two or three CT scans were performed to confirm the diagnosis. Of the 1,523 patients, 1,236 patients had pneumonia while 285 patients had no pneumonia. Of the 1,523 patients, 244 patients received oxygen therapy including high flow therapy. Although they had pneumonia, many patients improved with the administration of antibody therapy, antibiotics, and fluids without needing oxygen treatment.
Patients whose symptoms of pneumonia develop within 7 days of admission, and whose oxygen saturation is maintained at 95% or above, will be administered a monoclonal antibody treatment Regdanvimab (Regkirona) If their fever rises as the pneumonia develops and their CRP rises above 3-5, they will be placed under the antibiotic Tazoperan for 5 or more days. If their oxygen saturation falls below 94% as the pneumonia progresses, they will be administered Veklury (Remdesivir) for about 5 days. During the 5 days of administration of Veklury (Remdesivir), the fever usually drops, and the oxygen demand starts to decrease. It is difficult to predict who will develop a severe pneumonia and who won’t. Age or underlying diseases are not necessarily factors that make the pneumonia worse. Of course, it is true that for elderly people with many underlying diseases, it is difficult to endure the ventilator treatment in the case of a severe pneumonia, so the mortality rate is high. Frankly speaking, we found that age, gender, nationality and underlying diseases are not predictors. But obesity itself could be risk factor.
From the clinical picture, it is true that high fever itself means that the pneumonia or other organ’s inflammation is progressing, and it is clear that oxygen saturation decreases rapidly as the pneumonia progresses. It is important to administer monoclonal antibody therapy Regdanvimab (Regkirona) as early as possible in the early stage of the infection. Likewise, the antiviral drug, Veklury (Remdesivir) should also be administered at the very time when the oxygen saturation begins to drop. COVID 19 disease develops and progresses very fast, in the time frame of one or two days, therefore the two drugs, Regdanvimab (Regkirona) and Veklury (Remdesivir) should be administered to the COVID 19 patients in the early phase of the disease. Early phase treatment including monoclonal antibody treatment and antiviral agent is very important to control the COVID 19 virus disease. The current quarantine system in Republic of Korea which allows COVID 19 patients to be treated in hospitals at the initial stage of their COVID 19 disease diagnosis is believed to have lowered the death rate considerably compared to many other countries.
| For more Articles on : https://biomedres01.blogspot.com/ |



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.