Experience of Using Videolaparoscopic in the Treatment of Liver Echinococcosis
Recently, endoscopic interventions have begun to take up a significant share of all operations. The introduction of new technologies opens up broad prospects for the use of minimally invasive operations in various branches of surgery [1,2]. Video laparoscopy has become one of the promising areas of minimally invasive treatment of liver echinococcosis for highland Kyrgyzstan. It is gaining more and more popularity among surgeons and is used in almost all private clinics and many state surgical hospitals, both for diagnostic and therapeutic purposes, but this operation has not yet found application in the Kyrgyz Republic. According to world statistics, at present, minimally invasive interventions are used in almost a third of patients with echinococcosis [3,4]. Interest in the use of video laparoscopic technologies in liver echinococcosis is due to the fact that traditional interventions are accompanied by severe surgical trauma and long-term rehabilitation of patients [5-6], and the frequency of complications in the immediate postoperative period, which dictates the need to improve old and search for new methods of surgical treatment of echinococcosis.
Outcomes
To show the possibilities and effectiveness of video-laparoscopic technologies in the surgical treatment of liver echinococcosis in comparison with laparotomic liver echinococcectomy.
Material and Research Methods
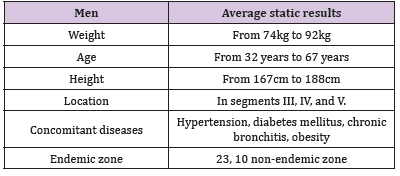
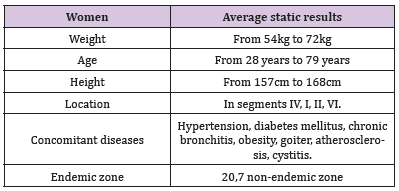
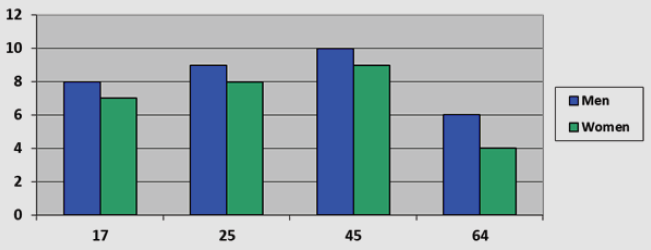
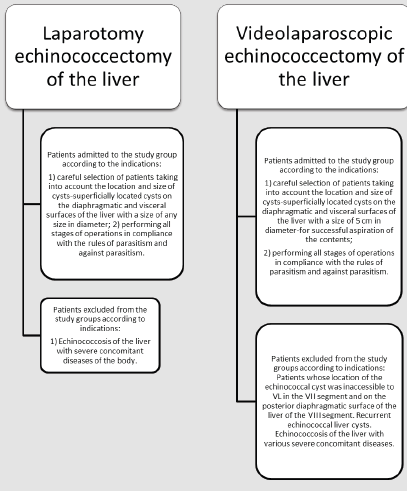
There were 60 patients hospitalized in the surgical department of the City Clinical Hospital No. 1 and the Educational-Medical- Scientific Medical Center of the Kyrgyz State Medical Academy named after I.K. Akhunbaev in Bishkek from 2018-2020, who were diagnosed with echinococcosis of the liver and underwent surgical treatment by video laparoscopy in 32 patients and 28 patients by laparotomy. The age of the patients is from 17 to 64 years old, of which 27 are women and 33 are men. (Figure 1) (Tables 1 & 2) The main diagnostic method was ultrasound, which was also used in the postoperative period to identify complications in the abdominal cavity and assess the results of surgical treatment. The diameter of echinococcal cysts (EC) ranged from 6.1 to 17 cm. All 45 patients had single cysts, 15 - two. They were localized in the III segment in 15, in the IV - in 12, at the border of the III - IV segments - in 18, in the V segment - 9, and in the VIII segment - 6. (Figure 2)
Results and Their Discussion
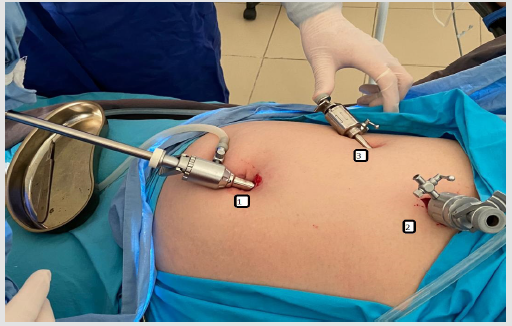
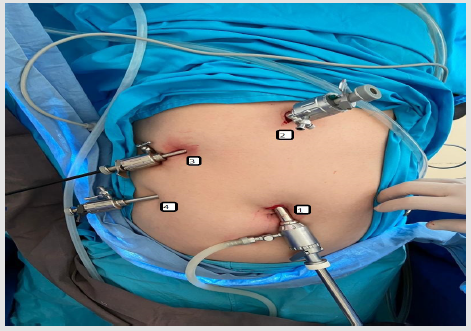
The variant of the operative technique was based on the use of 3 trocars, as shown in (Figure 3):
1. 10mm - main, paraumbilical;
2. Epigastric, 10mm - for the introduction and removal of a rubber bag with a chitinous sheath;
3. Subcostal, right 5mm.
In 2 cases, it became necessary to apply the 4th - mesogastric, 5 mm trocar, as shown in (Figure 4).
Access
The first trocar is placed on the superior paraumbilical point. Depending on the localization of the cyst, the rest of the trocars were imposed as follows: for the right-sided one, they were placed in the epigastrium and the right hypochondrium, and for the left-sided one, in the left hypochondrium along the midclavicular line and the epigastric point below the xiphoid process with its conduction to the left of the round ligament of the liver.
The Course of the Operation
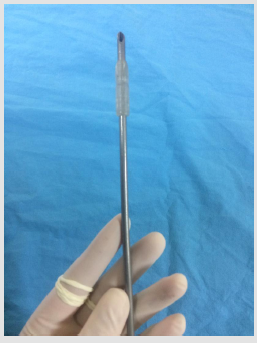
Before the puncture, the place of the proposed puncture was covered with a napkin moistened with Decasan solution. Then the cyst was punctured with a special puncture needle with a terminal extension, shown in Figure 3, the contents were aspirated as much as possible, and a 25% hypertonic sodium chloride solution was injected for 4-5 minutes. After exposure, the hypertonic solution was aspirated, then the cyst was opened and the chitinous membrane was removed in a homemade rubber bag (made from a sterile glove). (Figure 5) To detect biliary fistulas, the cavity was examined with a laparoscope and a dry sterile tissue was pressed to the floor of the cavity for several minutes. A partial pericystectomy was performed in 6 cases of superficial localization of the echinococcal cyst. In 7 cases the cavity was tamponized with a strand of the greater omentum, in 16 the cavity was removed by abdominalization, and in 3 patients the cavity was removed by invagination. The duration of the operation was 60 ± 5 minutes. Abdominal drainage was placed relative to the location of the cavity and removed on the 2nd or 3rd day.
To prevent relapse of hepatic echinococcosis all the patients were given 3 courses of chemotherapy - albendazole at the rate of 10-15 mg/kg during 24 days with 2 weeks interval between the courses. No accumulation of fluid in the residual cavity and in the subhepatic area was noted. One patient had moderate bile leakage of not more than 50 ml in the first day, it stopped on its own. There were no other complications. The hospital stay was 3-5 bed-days.In laparotomy treatment of hepatic echinococcosis. At the superficial localization of the echinococcal cyst, pericystectomy was performed in 8 cases. In 7 cases the cavity was tamponized with a strand of the greater omentum, in 7 cases the cavity was removed by abdominalization, and in 6 patients the cavity was removed by invagination. The duration of the operation was 80 ± 5 minutes. Abdominal drainage was placed relative to the location of the cavity and removed on day 5-7. When the patients were discharged from the hospital they were also given 3 courses of chemotherapy - albendazole at the rate of 10-15 mg/kg for 24 days with 2 weeks interval between the courses, in order to prevent relapse of liver echinococcosis. Fluid accumulation in the residual cavity and in the subhepatic area was noted in 3 patients. In 3 patients there was moderate bile leakage of not more than 70 ml in the first day, it stopped on its own. Complications in the form of superficial wound suppuration occurred in 6 patients after 4 days of stay in the hospital, wounds closed on the 12th-13th day. Hospital stay was 8-12 bed-days.
The conditions of the VL before commissioning were as follows:
1. Careful selection of patients with regard to location and size of cysts - superficially located cysts on the diaphragmatic and visceral surfaces of the liver measuring from 5 cm in diameter - for successful aspiration of the contents
2. Performing all phases of surgery in a parasitic and antiparasitic manner.
3. Patients with the following indications were not included in the group.
4. Patients whose echinococcal cyst location was inaccessible to VL in segment VII and posterior diaphragmatic surface of segment VIII liver.
5. Recurrent echinococcal cysts of the liver.
6. Echinococcosis of the liver with various severe comorbidities.
The main concerns about the consequences of the operation are not related to the technical capabilities of performing echinococcectomy, but to the danger of the spread of parasites and the recurrence of the disease. Therefore, the final decision on the possibility of high-power transmission lines was made after diagnostic laparoscopy. At the slightest doubt, the traditional method of surgical treatment was chosen. Undoubtedly, these operations should be performed by surgeons who know both laparoscopic and traditional open methods of echinococcectomy (Figure 6).
Conclusion
1. Laparoscopic methods of treatment of liver echinococcosis can be carried out, but with mandatory consideration of the size and location of cysts.
2. When performing laparoscopic echinococcectomy with even greater care and caution, the rules of aparasitism and antiparasitism should be observed in order to prevent infection of neighboring organs and the abdominal cavity.
Thus, VL is the most effective treatment of liver echinococcosis with suitable sizes and location in available segments.
| For more Articles on : https://biomedres01.blogspot.com/ |



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.