Diabetes and its Association with Peripheral Arterial Disease
Introduction
Diabetes
In the past five years, changes in lifestyle and globalization have led to significant changes in society, political systems, the environment, and human behavior. In underdeveloped and developing countries, the number of patients with diabetes and obesity has increased significantly [1-2]. Diabetes is now a major problem spread over the world and causing death in most countries [3]. In 2013, the International Diabetes Federation (IDF) estimated that there are approx. 382 M people worldwide suffer from diabetes, and this number is expected to increase to 592 million by 2035 [4]. It is the endocrine disorder in which the blood glucose/sugar level is very high as compared to the normal levels. The food is main source of glucose for the body. For the transportation of glucose into the cells and production of energy from it is done under the influence of a hormone, called insulin. The impaired insulin production and utilization of insulin by the body causes diabetes [5]. Diabetes is a chronic complex metabolic disorder, which requires continuous and regular medical care and checkup including multifactorial strategies to minimize the risks of complications’ development, presented clinically as the sustained and continuous hyperglycemic state in the body. Prolonged hyperglycemia can cause a large number of complications -renal, ocular, cardiovascular, and other recurrent infection. Studies have shown its high prevalence markedly in the developing countries or in the countries with lower to middle income status [5].
Diabetes and Insulin
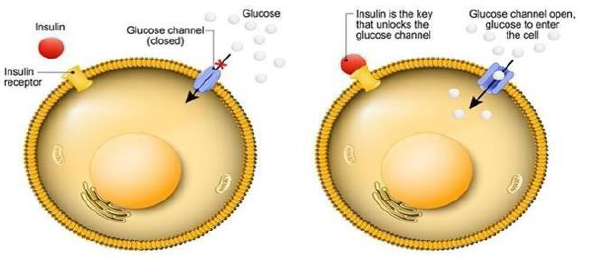
The National Institutes of Health has been invested almost $ 200 million in diabetes research. Human fluids have recently appeared, and oral medications are only sulfonylurea. Insulin pump technologies and home plasma glucose monitoring are still in the “early stages.” Pancreas transplantation was almost unsuccessful, and the surgical mortality rate was 25%. Only 30% of patients have not used insulin for more than 1 year, and the islet transplantation is unsuccessful. The incidence of diabetes across the country is now alarmingly increasing. In 2003, 13.8 M people in the United States were diagnosed with diabetes, including 5 million undiagnosed diabetes and 41 million pre-diabetic patients. Since 1990, due to demographic changes, the prevalence of diabetes has increased almost every year, especially among ethnic minorities, the increase in the incidence of diabetes, the increase in awareness and discovery of diabetes, the change in diagnostic criteria, and the consequent increase and microvascular complications, The further increase in individuals along with obesity, leads to insulin resistance, which leads to diabetes. The cost of the disease is 92 billion U.S. dollars, and the research investment in 2002 was slightly less than 800 M U.S. dollars [6]. Blood glucose level is regulated by insulin. Insulin is an endocrine hormone which is produced and secreted by beta cells of pancreas. Insulin performs its action by binding to the insulin receptors on outer membranes of the cells for the glucose uptake. The activation of receptors, release of insulin and uptake of glucose by the cells is regulated by downstream cell signaling pathway. The impaired secretion or binding both leads to impaired glucose uptake by the cells and resulting hyperglycemia [7].
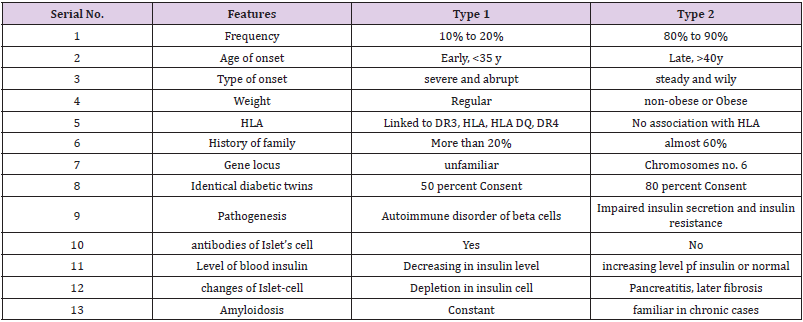
Types of Diabetes
There are 3 major types of diabetes, Type-1, Type-2 and
gestational. First one is linked with the insulin sensitivity. Second
one is linked with beta cells problems that are released by
pancreases. And third one is related with hormonal changes that
take place during pregnancy [8].
Type 1 Diabetes: Type-1 diabetes is insulin dependent diabetes
or Juvenile diabetes is an autoimmune disease, presented in
childhood, chronic in nature caused by insulin deficiency resulting
hyperglycemia. This condition requires the administration of
insulin in the body daily [8]. It is caused by autoimmune destruction
of endocrine pancreas’ β cells. The process of this autoimmune
destruction is influenced by genetic factors after being triggered by
any environmental factor and progresses with passage of time from
months to years. The increased knowledge regarding this type of
diabetes regarding its onset, epidemiology, genetics and treatment
due to increased research and investigations has increased the
burden of disease and helped to improve the management criteria
and protocol but still it is one of the common diseases globally [9].
The onset of type 1 DM is usually abrupt and is seen in people of age
less than 30 years. It can be fatal unless diagnosed and managed as
soon as possible. In 90℅ individuals it is autoimmune while in 10%
of individuals it is idiopathic. If remains untreated, type 1 DM can
become complicated and results ketoacidosis. It is observed that it
is seen mostly in young children of age 10-14 years, but sometimes
also seen in adults. Type 1 DM is considered to be a catabolic in
nature which is characterized by absence or reduced insulin
circulating in body. Levels of plasma glycogen is elevated, and the
beta cells of pancreas fail to respond to the insulin secretion stimuli.
Insulin injections are required to improve the metabolic disturbed
state, reduce the plasma glycogen levels, avoid ketoacidosis and
reduce glucose level of in blood [10].
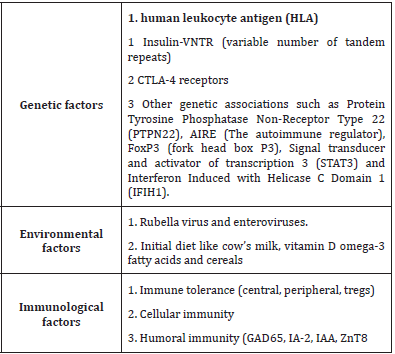
The contributing and predisposing factors of type 1 diabetes
are as follow [11].
Type 2 Diabetes: The type 2 diabetes in also known as insulin
independent or diabetes mellitus that is one of the most prevalent
disease today. The pathophysiology and causes of this disease are a
bit complex and is associated with non-modifiable and modifiable
risk factors. Modifiable risk factors include lifestyle, high blood
pressure, smoking, poor diet, and obesity. Unchangeable risk factors
include age, race, genetics, and ethnicity. By definition, the diabetes
is a metabolic or endocrine disease characterized by increased
glucose level either due to decreased action of insulin or decreased
secretion of insulin. The uncontrolled diabetes can lead to damage
to vital organs i.e., cardiovascular system, nerves, kidneys and
eyes. In diabetes mellitus, increased HBA1c level also considered
to be a cause of macrovascular and microvascular damages [12].
T2DM is more common as compared with T1DM. It usually remains
asymptomatic and usually diagnosed by chance. This is chronic in
nature and gradually develops. It is more common in elderly and
middle-aged people. As compared to T1DM it is usually milder,
compatible with life and ketoacidosis usually doesn’t develop. If
proper management and treatment is given, the survival rate is high.
The clinical presentation of T2DM can be seriously complicated in
the presence of comorbid conditions [10] Figure 1.
Figure 1: Activation of receptors, release of insulin and uptake of glucose by cells are controlled by downstream cell signaling pathways. In this diagram pathway is described by cell signaling. Constant raised blood glucose level which is called hyperglycemia is the major effect of uncontrolled diabetes. Hyperglycemia, with the passage of time leads to severe and serious damage to major body’s systems especially the blood vessels and nerves [8].
Complications of Diabetes Mellitus
Diabetics are at higher risk for developing the following
conditions that affect their ability to survive. Diabetes mellitus
is characterized by multiple microvascular like retinopathy,
nephropathy, neuropathy in addition to macrovascular such
ischemic heart disease, cerebrovascular disease, and peripheral
vascular disease [13]. This hormonal and metabolic disorder is
one of the most common endocrine diseases affecting about 6% of
the world’s population [14]. The type of diabetes associated with
coronary artery disease and other forms of heart disease is T2DM.
It is characterized by long pregnancy periods in which insulin
resistance is predominant, and hormones produce insulin with
B-cell compensation, which is sufficient to maintain normal blood
sugar. The work of Raven and colleagues has shown that coronary
artery disease is increasingly associated not only with diabetes,
but also with insulin resistance [13]. Type-2 diabetes-related heart
disease is a type of epicardial coronary artery disease, including
sudden cardiac death and severe coronary syndrome, unstable
angina, and severe myocardial infarction; Small vessel coronary
artery disease; Mental illness; Peripheral vascular disease;
Hypertension; and heart failure [15].
Gestational Diabetes: Suffering from this type of diabetes is
at risk of development of complications during whole pregnancy
and delivery. The child born to such mother also remains at risk
of type 2 diabetes in future [8]. In gestational diabetes, the blood
glucose levels are above the normal values but remains below the
diagnostic value of diabetes [10].
Prevalence of Diabetes: In the meeting of NDSP (2016-
17), the diabetes prevalence recorded was 26.3%, out of which
approximately 19% were chronic diabetic patients while
approximately 7% were newly declared diabetic patients [16]. The
increase in diabetes prevalence rate indicates the increase in the
occurrence of risk factors. The prevalence rate of diabetes mellitus
can be reduced by improving the modifiable factors [17].
Predisposing factors of Diabetes Mellitus: The predisposing
and risk factors of DM are a bit complex and are associated with
non-modifiable and modifiable risk factors. The modifiable risk
factors include lifestyle, hypertension, smoking, poor diet and
obesity. The non-modifiable risk factors include age, race, genetics
and ethnicity [12].
Risk Factors of Diabetes Mellitus: Diabetes mellitus is
the major cause of the chronic pancreatitis (CP) [18-20]. This is
nondependent risk factor for mortality in CP patients, with the
surgical procedures or not [21-25]. The endocrine pancreatic failure
can cause life-threatening problems like severe hypoglycemia [26]
or chronic macroangiopathy microgliopathy problems, which
are more common in diabetic CP patients than in other diabetic
patients [27-29]. Patients range from 41% to 86%. Number of
patients (medical, surgical or mixed) [30-33]. Non-functional
pancreatic tissue in patients with CP may be due to disease
progression or surgery. The role of enzyme secretion in decreasing
the diabetes is controversial. It is not possible to estimate the effects
of surgical procedures in post-diabetic diabetes for CP patients,
as most surgical procedures involve only one type of surgery or
patients with CP and other metabolic disorders or non-surgical
Are included. This prevents the evaluation of the correct effect of
metabolic surgery on the postoperative morbidity of diabetes. As
far as we know, compared to conservative treatment, there has
not been a major clinical-surgical study in CP patients undergoing
surgical treatment [34].
Symptoms of Diabetes: The earliest and common symptoms
of diabetes are as follow:
Type-1 and type-2 diabetes were accompanied by excessive
urination and fatigue. Irritability, easy fatigue of blurred vision,
and excessive thirst for both types of diabetes. The frequency of
symptoms was similar in the group of type-1 and type 2-diabetes
(p> 0.005), having frequent infections, numbness and tingling
in the hands and feet (more common in DM), weight loss (more
common in juvenile type diabetes) [35].
Pre-Diabetic Conditions: It is a condition of continuous
increased blood glucose level above the normal before development
of diabetes. It is a phase prior to development of diabetes. Research
showed that globally, about 415 million peoples presented
pre-diabetic condition in 2015 and this value may increase to
approximately 642 M till 2040 [36].
Insulin Resistance Syndrome (Syndrome X): In the
individuals who are obese and suffering from type 2 DM side by side,
the association of dyslipidemia, hypertension, hyper insulinemia
and hyperglycemia which can result coronary artery disease,
stroke and peripheral arterial disease can be result of genetic defect
causing insulin resistance, which can be more worsen by obesity.
Studies show that the insulin resistance further contributes to
increased blood glucose level, which causes hyperinsulinemia, and
the continuous increased level of insulin predisposes to increased
level of TAG (triglycerides) and more retention of sodium and
ultimately causing hypertension. In this way, elevated level of
insulin promotes the proliferation of endothelial cells. This whole
phenomenon stimulates the initiation of atherosclerosis [10].
Problem Statement: Diabetes, being a chronic disease, is an
iceberg disease. The incidence and prevalence of diabetes have
increased globally, but a dramatic increase is seen in developing
and newly industrialized countries [10].
Diagnosis
Diagnosis of diabetes can be made either by measuring plasma
glucose level (random or fasting) or by HBA1C. The randomly
measuring plasma glucose can be done after 2 horses of taking any
some food.
Fasting Plasma Glucose Level: After 8 hours of meal or
overnight fasting, a blood sample is taken. The value greater than
126 mg/dl is an indicator of diabetes.
Oral Glucose Tolerance Test: The procedure of this test
involves the measurement of the level of plasma glucose 2 hours
before and after ingesting 75mg of glucose. If the plasma level of
glucose in the second sample (after 2 hours of ingesting glucose) is
greater than 200mg/dl, diabetes is diagnosed.
HbA1C: HbA1C gives the average levels of blood glucose levels
over the last 3 months. It is a standardized, convenient and rapid
test. One of its drawbacks is its high cost. HbA1C greater than 6.5 %
is diagnostic for diabetes [37].
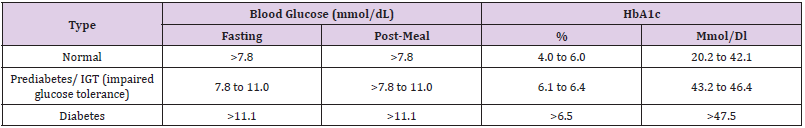
Blood Glucose Levels: The normal, pre-diabetic and diabetic
blood glucose levels are as follow [38].
Diabetes and Peripheral Arterial Diseases: Studies show
that that diabetes and peripheral arterial diseases are linked
with each other. Diabetes is a risk enhancer in peripheral arterial
diseases i.e., atherosclerosis. It is observed that even with the
improvements in treatments and investigation standards, the
risk of peripheral vascular disease is higher in diabetic patients
as compared to non-diabetic patients so with diabetes and PAD
have more significant probability and negative outcomes than
non-diabetic patients. People with diabetes type 2 and PAD have
a higher risk of amputation in lower extremity, and a higher risk
of coronary heart disease. Over 5 years, 20% of diabetics with PAD
will develop myocardial infarction or stroke and 30% will die of
heart disease. Patients with ischemia: 30% remission and 20% will
die within 6 months [38].
Peripheral Arterial Disease: Peripheral arterial disease (PAD)
is caused by atherosclerosis, which can cause arteries to narrow or
occlude, resulting in less blood flow to the affected arteries [39]. It
is also called peripheral vascular disease and may be an increased
risk factor for other vascular events [40]. This disease has become
an important issue in the field of health because it not only affects
daily activities and other physical activities, but also affects mental
health [41], which significantly affects the quality of life of patients
[42-43]. There are approximately 236 million people in the world.
23.6 hundred people long-lived and older are affected by PAD [44].
According to reports, 15 countries include more than two-thirds of
global PAD cases in 2015.In Western countries, despite the declining
incidence of disease, the mortality rate of PAD has been increasing
for many years [45-46]. With the general aging of the population
as well as the increasing complexity of the associated diseases, this
trend is expected to become commonplace in the future [47]. Proper
blood flow to the affected limb is important, otherwise it will lead
to increased stiffness and severe limb ischemia (CLI) symptoms,
accompanied by resting pain and cramps in the affected limb.
When a patient develops CLI, the estimated 1-year survival rate
with two limbs is only 45% [48]. Finally, endovascular treatment
(EVT) is easily performed as a first-line rehabilitation intervention
for the treatment of PAD, and surgery provides an alternative to
EVT [49-50]. However, these interventions are not often tolerated,
especially for patients with high risk factors and most debilitating
diseases, such as heart disease (CVD) and diabetes (DM), which can
sometimes lead to muscle loss. Become the cause of death or death [51].
Therefore, the long-term success of revascularization should
be measured by preventing amputation and reducing the burden
of symptoms [52]. The efficacy and long-term consequences of
the intervention are generally evaluated by clinical measures of
implant-free survival (AFS), because over time, such organ-related
results are useful for measuring survival rates and organ defense
capabilities [53]. In contrast, different risk factors for PAD (such
as smoking, diabetes, cardiovascular disease) have been reported
[54]. However, the risk factors that affect the results of AFS after
revascularization have not been determined. The purpose of this
study is to determine the risk factors associated with the reduction
of AFS in PAD patients after intravascular or surgical intervention
and use these transformative and irreversible risk factors useful
information that can develop on the basis of evidence-based
interventions, providing better facilities for patients’ long-term
recovery [54].
Mechanism of Disease Onset: The development of PAD
involves the atherosclerosis in the major large vessels including
aorta (abdominal part), iliac artery and femoral artery Figure 2. The
process of atherosclerosis initiates with the interaction between
the vascular cells and cholesterol. The atherosclerotic plaque is
formed gradually inside the any of above arteries. In the initial
stage of PAD, the arteries dilate to compensate the plaque and to
preserve the flow of blood through vessels. On the progression of
the disease, the arteries cannot further dilate, and the plaque causes
vessel stenosis and blocks the blood flow. This blockage in the
flow of blood represents the hallmark and clinical manifestations
of PAD and associated typical signs and symptoms [55]. As the
severity of hypoxia increases, microvascular adaptation becomes
unbearable. Completely replace mitochondrial damage and free
radical generation and subsequent muscle fiber damage, muscle
fiber degeneration and fibrosis. These changes ultimately lead to
hypoxia and better metabolic requirements, such as discomfort,
extreme pain that cannot be improved or damage the body, and
then debilitates the organs. Blue represents the direction of blood
flow to the muscles, and white represents increased blood pressure
in severe cases [56].
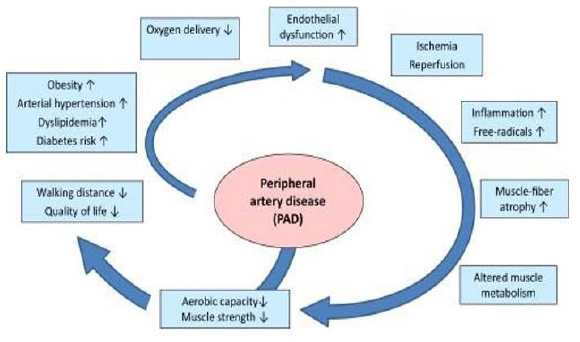
Figure 2: Schematic diagram of ischemic disease in PAD disease. Initially, the ischemic limb seeks to compensate and solve the problem of hypoxia by modifying microvascular and reducing hemodynamics to promote angiogenesis and/or estrogen production.
Risk Factors: Risk factors, medical management, and
intravascular interventions are considered key strategies for
the treatment and management of PAD [40]. Current systematic
reviews have found that older age, male gender, African American
race, lower BMI, higher risk and associated dietary coordination
(CVD, kidney disease, DM, dementia, detailed PP). Severe cases of
PAD and other medical complications have been identified as risk
factors for AFS. This study is similar to previous studies and used
to predict long-term outcomes (e.g., remission and survival) of PAD
patients after treatment [57-58]. The factors involved in these risks
are divided into personal and impersonal, which will be discussed
below. European Society of Cardiology Card (ESC) 2017 Chiropractic
Recommendations Check (CRC) and manage Chiropractic
recommendations for diagnosis and treatment guidelines [40].
According to research, these conditions include weight and food
hazards, including defects and abilities. First, obesity is similar to
the pathophysiological pathway of atherosclerosis and is a risk
factor for ischemic events [59].
Signs and Symptoms: Peripheral artery disease usually
asymptomatic but some patient shows generalized nonspecific
symptoms. Patient may complain fatigue, numbness in hand and
feet and burning sensation in the sole of feet especially at night
[35]. There are different modes of signs and symptoms in the
patient having peripheral artery disease. Mostly patient discomfort
during walking and having pain in legs. There are two most severe
symptoms that mostly appear after some time include intermittent
claudication and rest pain in legs. The aortoiliac disease patient
may also suffer from buttock and thigh discomfort. In PAD, due
to accumulation of lactic acid in muscles patient may also suffer
from some failure of power sense as they cannot be able to walk
for longer period of time and need to sit after 15-20 minutes of
walk named as claudication [60]. Intermittent claudication is the
discomfort of legs, pain and cramping with due to heavy activity
such as running and exercise. The pain mainly noticed in the calf but
may also be felt in the buttocks or thighs. The pain must be severe
enough that cause difficulty with normal walking and that pain can
be caused due to the decreased in blood flow in legs muscles. This
type of pain can be treated by having rest as the leg muscles relaxed
during low blood flow. The claudication remains stable about 70-80
% in patient for 10 years of period [61]. Rest pain in legs occur in
PAD patient when there is no proper supply of oxygen and blood in
legs muscles, and it is more severe condition when this can affect
the feet even during night when patient lying with face up [62]. The
common signs and symptoms include coldness in lower leg and
foot, toes and foot become sore that won’t heal, legs skin become
shiny, weak pulse in your legs or feet, hair loss on feet and legs,
slower growth of toenails and change in legs color [63].
Diagnosis of PAD: The diagnosis of PAD is medically important
for two reasons. The first is to identify patients at risk of advanced
myocardial infarction or stroke, even those with symptoms of
peripheral arterial disease. The second is the detection and
treatment of PAD symptoms, which may be related to dysfunction
and organ failure. The symptoms of PAD in diabetic patients are
usually more subtle than those in diabetic patients. Patients with
diabetes are at higher risk of developing PAD and hemorrhage
than proximal and near-atherosclerotic lesions, which are more
common in high-risk patients. In particular, PAD in diabetic
patients usually has a poor prognostic response to peripheral
neuropathy. Therefore, the general serious medical history may
be less common. However, patients may experience more subtle
symptoms, such as leg fatigue and slow walking, which can only
be considered wiretapping. The report pointed out that patients
with PAD and diabetes have lower body counts than single patients
[64]. In addition, diabetic patients identified with PAD are at
higher risk of sudden ischemia of arterial thrombosis [65] or a
significant event that may lead to neurobiochemical ulceration or
infection resulting in severe peripheral arterial disease causes the
limb ischemia. PAD with diabetes leads to gangrene formation in
effected area, contributing long term disorder and disability due to
functional impairment that’s other very severe. People with aortic
stenosis walk slowly (usually less than 2 miles per hour) and have
limited walking distance. This may lead to a “helpless cycle” with
gradual dysfunction and loss of function. Finally, the medical care,
productivity decline, and personal expenditures associated with
chronic manifestations of PAD (such as atherosclerotic disease) can
bring huge economic costs [66].
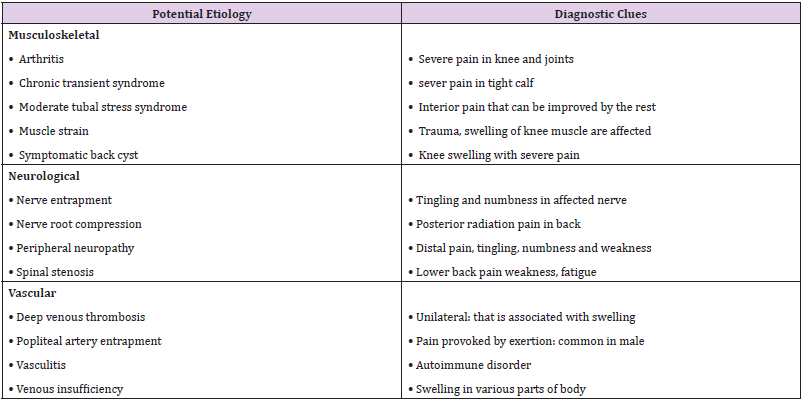
Differential Diagnosis: The physical examination and clinical
history are essential in the diagnostic procedure of PAD, it must be
distinguished from other type of claudication [35].
Management: The PAD can be managed by the primary
care and some modifications in risk factor that can cause PAD.
These risk factors include high blood pressure, age, smoking,
hypercholesterolemia, family history and physical inactivity. Person
aged 65-70 are at increased risk of having PAD. The incidence ratio
of PAD is about 14.5% in aged between 65-70 and the ratio in older
than 40 years is 4.3% [67]. If the risk factors are managed than it
will prevent the progression of PAD. Smoking, hypercholesterolemia
and physical inactivity are the most important risk factors that
can cause PAD. For hypercholesterolemia, static drugs are advised
by the doctor that are used to lower the cholesterol level mainly
low-density lipoprotein (LDL). These risk factors can be treated
according to doctor’s guideline. For the PAD management, person
should quit smoking as smoker have high incidence rate then
nonsmoker and it is compulsory to maintain body index. If body
mass index is greater than 25then person should maintain body
weight. It the body wait is higher according to body mass index than
the person should lose its weight and do exercise regularly [68,69].
Patient should receive antiplatelet therapy to prevent progression
of PAD. Some recent analysis shoes that the use of clopidogrel drug
is more effective to prevent PAD then aspirin. Continuously use
of more than one antiplatelet drug are not recommended for the
patient that are at low risk. The use of warfarin drug is not routinely
recommended for the patients having PAD unless they have a
separate prescription for its use [70].
Prognosis: The prognosis of the PAD depends upon the
patient’s risk factors, severity of disease, any comorbidity and
cardiovascular health status. Regarding the lower extremity health
in 5 years, almost 80 % of the patients show the symptoms of
stable claudication. Just in 1-2% patients, the disease progresses
to serious extremity ischemia in 5 years. Within 5 years, the 20-
30% of patients suffering from PAD, die out of which almost 70%
patients suffered from cardiovascular damage/event [71].
Diabetes and Its Association with PAD
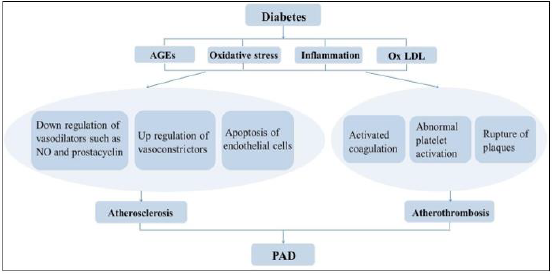
In peripheral arterial disease associated with diabetes, the increased level of glucose and abnormal lipid profile leads to dysfunction of endothelium of vessels, which causes dysfunction of vessel’s smooth muscle cells leading to inflammatory reaction and results in hypercoagulability state which play a vital role in development of arteriopathy associated with diabetic condition. The occurrence of peripheral vascular disease, in addition to its increased risk of ischemia, ulcers, gangrene formation and resulting amputation, is a risk factor for generalized atherosclerosis and cardiovascular disorders i.e., myocardial infarction and stroke [72- 73]. The patients suffering from diabetes and PAD simultaneously are at higher risk of development of morbidity and increased mortality from CVS diseases and increased rates of lower limb amputation. This resulting higher risks of amputation in patients suffering from diabetes is because of dry gangrene development, ulcers in foot which develops secondary to the PAD, and latestage presentation of patients with PAD. Approximately two-third of patients of diabetes having foot ulcers also have PAD, that is associated with greater risk of amputation and death rate. (Table 1) The PAD prevalence is almost 4 times greater and serious in diabetic patients as compared to patients who are not diabetic. The worldwide PAD prevalence is almost 200 million [74].
Pathophysiology
High blood sugar level and increased cholesterol level causes endothelial injuries. The reactive oxygen species are formed that oxidize LDL (low density lipoproteins) Figure 3. These products causes’ plaque formation as described above and causes vessel stenosis. These vascular changes can also lead to the thinning and hardening of vessels. Ultimately, these all-pathological changes results in development of peripheral arterial disease (PAD). Peripheral Arterial disease And Amputation of Lower Extremities The risk of lower limb amputation is increased by the peripheral arterial disease. It, itself an independent variant and indicator of cerebrovascular and cardiovascular disease, thus affect not only the quality of life but also the life expectancy. Studies have shown the prevalence of peripheral arterial disease in the patients suffering from diabetes mellitus is higher than in patients who are nondiabetic. In the patients suffering from diabetes, the peripheral; arterial disease occurs with high progression rate and usually remains asymptomatic. Many metabolic problems in diabetes i.e. HBA1c elevated level, abnormal oxidative stress, high level of LDL and constant hyperglycemic state have shown to worsening the pre-existing peripheral arterial disease [75,76].
Figure 3: Peripheral arterial disease related with diabetes in several ways. In this figure there are several symptoms explained. Some symptoms are appeared in diabetes patients after all their blood vessels blockage, the blood flow does not maintain, and peripheral arterial disease occur [75].
Diabetic Foot
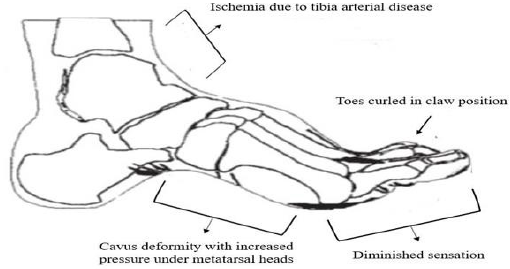
Figure 4 Diabetic foot is also a complication caused by peripheral arterial disorder in the lower extremities of diabetic patient. The mechanism of this disorder is given below [76]:
Figure 4: The underlying mechanism of diabetes foot ulcer. Sensory-motor neuropathy senses a loss of sensation in the legs and muscles of the stomach, resulting in metatarsal, flexed metatarsal overgrowth, and flex fungus. Ischemia and microvascular dysfunction lead to changes in the legs, resulting in ulcers [76].
Epidemiology
Epidemiological studies done globally have shown an association and link between diabetes and increased cases of peripheral arterial disease. Although patients usually do not show any symptoms, almost one-third of the patient’s complaint the intermittent blockage, presented as cramping, aching, numbness and tingling in the affected extremity which started on exertion and relieved by rest. Research showed that almost 12 million peoples in U.S suffered from peripheral arterial disease out of which approximately 20-30% of such patients are diabetic [77]. Studies showed, in 2011, almost 366 million people globally, or almost 8 % in the age group of 20-79 years had type 2 diabetes. This percentage is estimated to rise up to almost 550million by the year 2030. Greater than 50% of patients suffering from diabetes die due to any cardiovascular event i.e. myocardial infarction and stroke [78].
Diagnosis protocol
The diagnostic protocol can be followed as below [79].
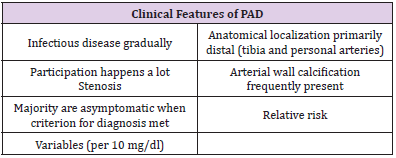
Risk Factors for Diabetes and Associated PAD: The two main risks of PAD are smoking and diabetes. Both of these risk factors are related to heart disease and stroke, but especially more so with PAD. Based on a PAD diagnosis of ABI 0.9, the relative risk of PAD was 4.05 for diabetes and 2.55 for current smoking in heart health studies (CSS) (Tables 2-4) [80-82].
Preventive Measures: To prevent development of diabetes and associated PAD, following preventive measures should be done by exercise regularly, quit smoking, lower blood pressure, lower cholesterol level and maintain normal blood sugar level [83].
Conclusion and Future Perspectives: Diabetes is a chronic progressing disorder which can be associated with serious complications i.e. PAD is not controlled and diagnosed. PAD can result in disability due to amputation of limb. Diabetes associated with PAD leads to severe cardiovascular damage resulting myocardial infarction and stroke thus, increases mortality and morbidity rates. Diabetes and associated PAD can be prevented by avoiding and minimizing risk factors. Diabetes is one of the commonest and most prevalent disease in Pakistan. PAD is its one of the major and serious complication. Previous studies and all above given discussion shows that it is increasing day by day and thus increasing mortality and morbidity rate. Amputation of limbs due to ulceration and gangrene is one of the major manifestations of developing PAD. With the advancement of medical knowledge and in this era of technology, many investigatory methods have been introduced to investigate and diagnose such complicated disease earlier and sooner so that it can be treated and managed as soon as possible, and the resulting complications can be avoided. The risk factors causing diabetes and its associated PAD can be reduced by lifestyle changes and preventive measures should be adopted to reduce the risk of development of the disease and its complications if the risk factors are irreversible. If the disease is initiated, continuous medical care should be taken, with regular follow up investigations to keep the prognosis of the disease slow and to prevent further complications. If primordial and primary interventions are not adopted and disease’s clinical manifestations are presented, the secondary interventions should be done to prevent any further serious illness, PAD and disability due to limb amputation (Table 5).
With advancement of medical technology, more efficient methods of investigations and management and treatments are introduced. By adding primordial and primary modes of interventions with these techniques and management, the risk of development of diabetes and its associated PAD can be prevented. However, the changing sedentary lifestyles and increasing risk factors increase the rate of development of this disease and more serious complications.
For more Articles on : https://biomedres01.blogspot.com/


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.