Efficacy of IV Immunoglobulins on Psychiatric Symptoms: A Case Report
Introduction
Borderline personality disorder (BPD) is a fairly common psychiatric illness with a prevalence between 1.8% and 2% in the general population [1]. Diagnostic Criteria in the DSM-5 [2]: BPD is a pervasive pattern of instability in interpersonal relationships, self-image, and mood and marked impulsivity that begins by early adulthood and is present in a variety of contexts, as indicated by five (or more) of the following:
a) Desperate efforts to avoid real or imagined abandonment
(do not include behaviours indicated in criterion 5). A pattern of
unstable and intense interpersonal relationships, characterized
by the alternating between extremes of hyper-idealisation and
devaluation.
b) Altered identity: markedly and persistently unstable selfimage
or self-perception.
c) Impulsivity in at least two areas that are potentially
harmful to the subject (e.g. reckless spending, promiscuous sex,
substance abuse, reckless driving, binge drinking,).
d) Recurrent suicidal behaviour, gestures or threats, or
self-mutilating behaviour (self-harm, cuts on arms and legs,
cigarette burns, etc.).
e) Affective instability due to marked mood reactivity (e.g.,
episodic intense dysphoria, irritability or anxiety, usually
lasting a few hours, and only rarely more than a few days).
f) Chronic feelings of emptiness.
g) Inappropriate, intense anger or difficulty controlling
anger (e.g., frequent bouts of anger or constant rage, recurrent
physical confrontations).
h) Transient paranoid ideation, associated with stress, or
severe dissociative symptoms.
Individuals with this disorder have recurrent suicidal behavior, gestures or threats, or self-harming behavior. Successful suicide occurs in 8-10% of such individuals, and self-harming gestures (e.g., cutting or burning oneself) and suicide threats and attempts are very common (DSM-5) [2]. Major depressive disorder (MDD) is the most frequent comorbidity with a prevalence of 41-83% [3], followed by substance use disorder with a prevalence of 78% [4]. The basic therapy of BPD is psychotherapy while psychopharmacology has an additional role as symptomatic and treating comorbidities [5]. Current evidence from randomised controlled trials suggests that pharmacological treatment, particularly with mood stabilisers and second-generation antipsychotics, may be effective for symptomatic treatment, but the evidence does not currently support efficacy for the overall severity of BPD [6].
Some studies in literature highlight the correlation between immune-mediated inflammation and psychiatric disease. Intravenous immunoglobulins (IVIG) are a widely used therapy in the field of autoimmune diseases, and in particular in several neuroimmunological disorders [7]. IVIGs regulate the immune system with multiple mechanisms: modulation of Fc receptor function, interference with cytokine release and function; interference with complement activation; presence of anti-idiotype antibodies; modulation of B and T lymphocyte activity. There are few studies about the efficacy of IV immunoglobulins in psychiatric features [8-10].
Case Presentation
A 40-year patient diagnosed with borderline personality disorder and major depressive disorder in comorbidity with myasthenia was hospitalized for self-harm and suicidal behavior due to impulsivity. She showed particularly pronounced levels of the self-conscious emotions, shame and guilt, instability of affect, emotion dysregulation, feeling of emptiness, lack of interest to all activity, sleep disturbance, anxiety and depressed mood. Pharmacological treatment with acid valproic, aripiprazole and gabapentin were prescribed in addition to pyridostigmine. In the psychiatric history she was diagnosed with drug addiction (quetiapine, benzodiazepine, sedative antipsychotics and cocaine) and eating disorder. During hospitalization she had daily non suicidal self-injuries, agitation and she showed craving for quetiapine, benzodiazepine, sedative antipsychotics. After one week of hospitalization, she had a myasthenic crisis, glucocorticoids were contraindicated due to the psychiatric side effects, so intravenous immunoglobulins (IVIG) were prescribed by neurologist (0.4 mg/ kg/day for 5 days) in addition to azathioprine.
After one day of IVIG the psychiatric features improved: patient
reported an improved mood, lower level of agitation, a reduction
of self-harm behaviors and an improved nighttime sleep. After
sixth days of IVIG was observed a remission of myasthenic crisis
by the neurologist and the IVIG were stopped. Consolidated the
neurological and psychiatric improvements, the patient was
discharged. After 8 months, at the follow-up visit, the patient
had no re-exacerbations of psychiatric or myasthenic symptoms,
she regularly took the prescribed therapy with acid valproic,
aripiprazole, gabapentin, pyridostigmine and azathioprine and she
also has been in psychotherapy for 7 months and she has started
a new job in addition to taking care of her two children. At the
admission in hospital (T0), an assessment was performed by the
clinician with the following interviews:
a) Inventory of Statements About Self-Injury (ISAS)
b) Barrat Impulsiveness Scale, Version 11 (BIS-11)
c) Hamilton Anxiety Rating Scale (HAM-A)
d) Montgomery-Asberg Depression Rating Scale (MADRS)
e) Alexian Brothers Urge to Self-Injure Scale (ABUSI)
The same evaluation was repeated at the end of the IgEV
administration (6 days – T1) and after 8 months (T2) without other
treatment modifications.
Results
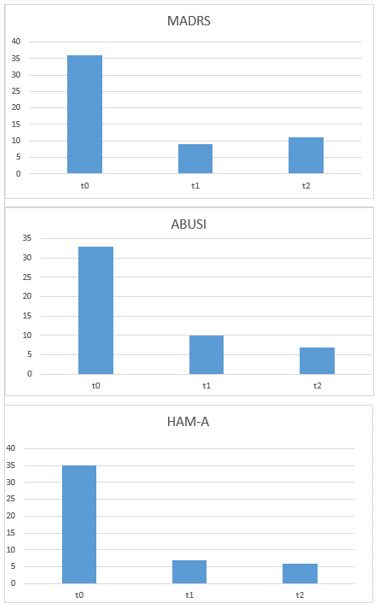
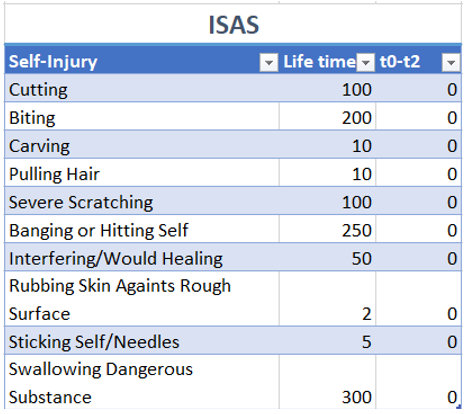
The patient presented a score of 79 at BIS-11. She reported a huge number of self-harm and suicidal behaviors as reported on ISAS (Figure 1). In Figure 2 we can see the reduction of anxiety, depressive symptoms and self-harm from t0 to t2.
Conclusion
We observed a reduction in self harm, impulsivity and a remission of depressive symptoms, only mild level of anxiety was reported immediately after the administration of immunoglobulins, and the remission continued up to 8 months after the administration (Figure 2). Further studies are needed to explain the mechanism that led to remission of psychiatric symptoms after administration of IVIG. Even though, the remission of the myasthenic crisis has led to an improvement of the psychiatric features, further causes cannot be excluded. Some studies in literature highlight the correlation between immune-mediated inflammation and psychiatric disease. However, there are few studies about the efficacy of IV immunoglobulins in psychiatric features which will needed to have more evidence and to better understanding the mechanism of action [8-10].
For more Articles on : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.