Prognostic Significance of Mean Platelet Volume to Lymphocyte Ratio in Patients with Metastatic Colon Cancer
Introduction
Colorectal cancer is the second most common cancer, the third
most common cause of cancer death [1]. Approximately 25% of the
patients have metastatic disease at the time of diagnosis, and about
half of these patients die within the first 5 years [2]. Inflammation
plays an important role in the development of cancer, tumor
progression, angiogenesis, and cancer metastasis [3]. Infection,
chronic irritation and inflammation are the underlying causes
of the development of many types of cancer. Previous studies
have shown that inflammatory biomarkers such as Neutrophil/
Lymphocyte Ratio (NLR), Plateret/Lymphocyte Ratio (PLR),
Monocyte/Lymphocyte Ratio (MLR), Mean Platelet Volume (MPV),
and C-reactive Protein (CRP) may be used as prognostic factors in
gastrointestinal cancers [4,5]. Platelet activation is known to play
an essential role in tumor growth and metastasis. Studies have
shown that PLR is a negative prognostic marker in advanced cancer
[6]. MPV is associated platelet activation and production as well as
the mean platelet volume in the blood [7,8]. Studies revealed that
MPV is closely related with many types of cancer such as colon,
thyroid and, renal cell carcinoma [9-11].
Tumor Node Metastasis (TNM) staging system remains a prominent method in predicting prognosis and determining treatment options. However, the survival of patients even in the same stage varies. New biomarkers are required to determine the prognosis. Platelet, MPV and lymphocyte levels, which are among the most analyzed parameters in peripheral blood, are both costeffective and routinely usable inflammatory markers. In this study, we aimed to investigate the prognostic significance of MPVLR in patients with metastatic colon cancer.
Methodology
A total of one hundred sixteen patients, diagnosed as colon cancer with de novo metastatic disease or developed metastasis during follow-up, between January 2014 and December 2020, were retrospectively evaluated. Inclusion criteria for the study were patients over 18 years of age, histopathologically diagnosed with colon adenocarcinoma, and patients who developed metastases during diagnosis or during follow-up. Patients receiving antiinflammatory therapy, patients with hematological or autoimmune diseases, heart failure and hemodialysis patients were excluded from the study. Information obtained from patients’ files and computer records are as follows: Age, gender, tumor localization (right colon vs. left colon), grade, number of chemotherapy steps, metastasis status at the time of diagnosis, blood hematological and biochemical markers, history of metastasectomy, KRAS, NRAS, BRAF mutation status, presence of liver metastases. Peripheral blood samples were taken from De nova metastatic patients before treatment. Peripheral blood samples were taken before any treatment when metastasis was detected in the patients who developed metastases during the follow-up.
Overall survival was determined as the length of time from metastatic diagnosis to death, or to the last follow-up date for survivors. Progression-free survival was accepted as the length of time from metastatic diagnosis to disease progression, or to the last follow-up date for patients without progression. All patients received biological agents such as bevacizumab, cetuximab or panitumumab depending on the mutation status. Peripheral venous blood samples were collected into sterile blood collection tubes containing Ethylenediaminetetraacetic Acid (EDTA) (5-7 ml). Mean platelet volume to lymphocyte ratio was estimated by dividing MPV (fL) by the number of lymphocytes (109/L). All statistical analyzes were performed using Statistical Package for the Social Sciences (SPSS) 20 (IBM Corporation, New York, NY) software. The relationship between categorical variables was assessed by chi-square test. Categorical data were expressed as frequencies and percentages. The relationship between MPVLR and prognosis was evaluated using the cox analysis. Multivariant analysis was performed using the cox proportional hazards model. Hazard ratios (HR) were estimated from the cox regresyon analysis and were reported as relative risk with corresponding 95% Confidence Intervals (Cls). Receiver Operating Characteristic (ROC) curve analysis was performed to estimate the best cut-off value of MPVLR for overall survival. The best cut-off point was expressed by using the Youden index (sensivity + specificity -1). A value of P<0.05 was considered statistically significant.
Results
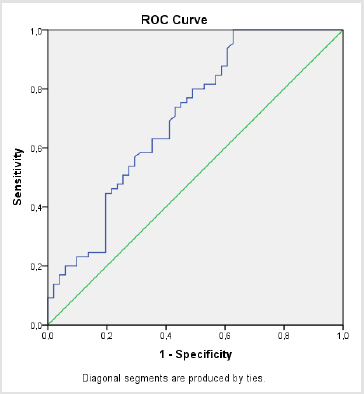
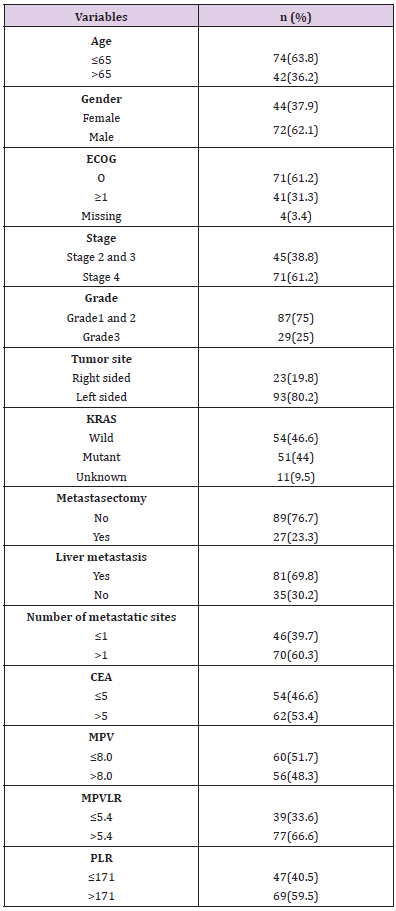
The clinicopathological characteristics of the patients were shown in Table 1. Forty-four (37.9%) of 116 patients were female and 72 (62.1%) were male. The median age of the patients was 65 (range 25-86) years. Median follow-up time was 21 months (0- 105). The estimated 5-year survival was 63%. During the follow-up, 65 (56%) of the patients died. Patients with confirmed mutation received targeted therapy as first line treatment. Mean platelet volume to lymphocyte ratio cut-off point for Overall Survival (OS) was estimated as 5.4 (AUC 0.800, 95% Cl: 0.611-0.804, p=0.000) (Figure 1). Optimum cut off point for PLR was estimated as 171 (AUC 0.564, 95% Cl: 0.458-0.670; p=0.237). Specificity and sensitivity of MPVLR was 80% and 51%, and of PLR 67% and 51%, respectively. Median value of MPV estimated as cut off (median MPV 8 fL).
ECOG: Eastern Cooperative Oncology Group Performance Status; CEA: Carcinoembryonic Antigen; MPV: Mean Platelet Volume; MPVLR: Mean Platelet Volume to Lymphocyte ratio; PLR: Platelet to Lymphocyte ratio
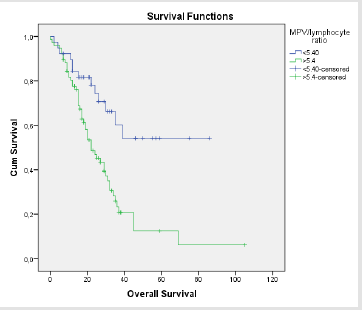
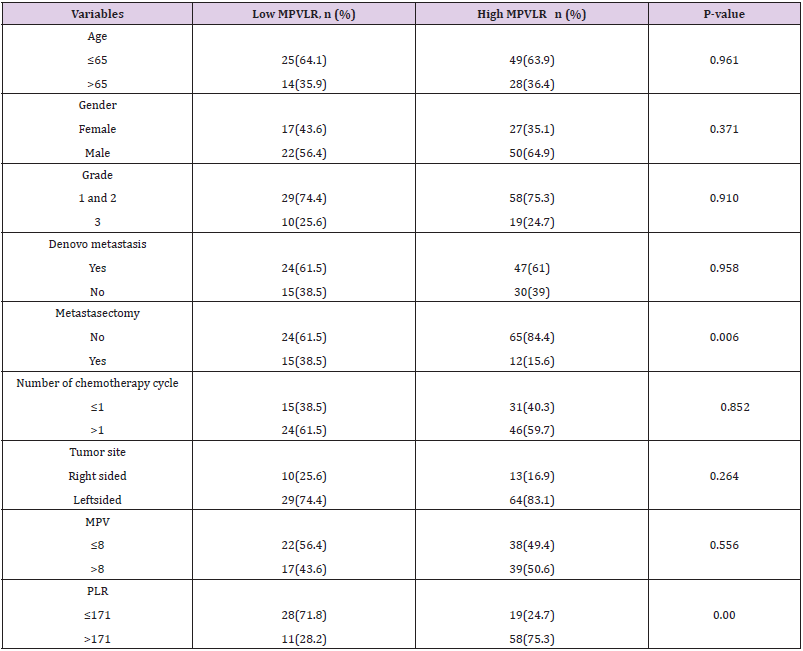
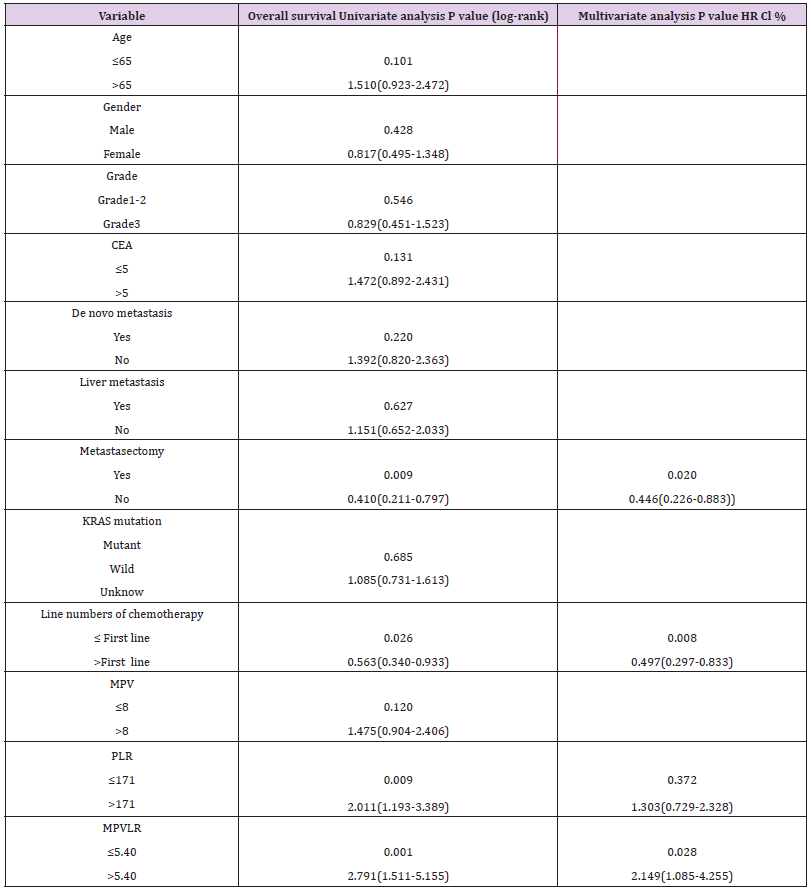
There was no significant relationship between age, gender, grade, de novo metastasis, number of received chemotherapy lines, tumor location, and MPVLR. A significant relationship was found between MPVLR and PLR (p <0.001), and metastasectomy (p=0.006) (Table 2). Mean platelet volume to lymphocyte ratio was categorized into two groups according to cut off point. There were 39 and 77 patients in MPVLR below 5.4 and above 5.4 groups, respectively. Death occurred in 13 out of 39 patients with MPVLR level below 5.4 while 52 out of 77 patients died in the other group. Survival was worse in patients with MPVLR above 5.4 (HR: 2.149, 95 Cl: 1.085-4.255, p=0.001). Median survival was not available in patients with MPVLR less than 5.4, while it was 22 months in patients with MPVLR above 5.4 (Figure 2). Univariate analysis revealed that metastasectomy (p=0.009), number of chemotherapy lines (p=0.026), PLR (p=0.009) and MPVLR (p=0.001) had significant effect on overall survival. There was no significant effect of age (0.101), gender (0.428), grade (0.546), presence of liver metastases (0.627), de novo metastasis (p=0.220), KRAS mutation status (0.685), MPV (0.120), and CEA (0.131) on overall survival. Multivariate cox regression analysis showed that the effects of metastasectomy (HR: 0.446, 95% Cl: 0.226-0.883, p=0.020), number of chemotherapy lines (HR: 0.497, 95% Cl: 0.297-0.833, p=0.008) and MPVLR (HR: 2.149, 95% Cl 1.085-4.255, p=0.031) on overall survival continued (Table 3). Univariate analysis showed no significant effect of age (p=0.542), gender (p=0.712), de novo metastasis (p=0.133), KRAS mutation status (p=0.251), and PLR (p=0.08) on Progression Free Survival (PFS). Metastasectomy was found to have significant effect on PFS (p=0.049). There was no significant difference in PFS between patients with MPVLR below and above 5.4 (P=0.422, HR: 1.181 Cl: 0.776-1.797).
MPV: Mean Platelet Volume; PLR: Platelet to Lymphocyte ratio; MPVLR: Mean Platelet Volume to Lymphocyte ratio
Table 3: Univariate and multivariate analyzes of clinicopathologic variables in terms of overall survival.
MPV: Mean Platelet Volume; PLR: Platelet to Lymphocyte ratio; MPVLR: Mean Platelet Volume to Lymphocyte ratio.
Discussion
In our study, survival was found to be shorter in patients
with high MPVLR, and high MPVLR was determined as poor
prognostic factor in metastatic colon cancer. This study was the
first to investigate the prognostic effect of MPVLR on metastatic
colon cancer. The relationship between inflammation and
cancer was defined by Rudolf Virchow in the 19th century [12].
Lymphocytes constitute the main component of the immune
system. Tumor-Infiltrating Lymphocytes (TILs), constitute one of
the most important effector mechanisms of anti-tumor immunity
[13]. Tumor cells are surrounded by immune cells, especially
lymphocytes. Lymphocytes play an important role in anti-tumor
immunity by inducing apoptosis and preventing the migration
and proliferation of tumor cells [14-16]. Lymphopenia was
determined to be associated with poor prognosis in many types
of cancer [16-19]. Platelets play an important role in hemostasis
and thrombosis. In addition, platelets contribute to the growth,
dissemination, and angiogenesis process of tumor cells. Plateletderived
growth factor, mainly secreted from platelets, and tissue
growth factor also leads to tumor growth [20,21]. Proinflammatory
cytokines released by cancer cells increase platelet count through
megakaryocyte proliferation [22]. Considering the relationship
between platelet and cancer, platelet-based markers can be used
to determine the prognosis of colon cancer. Mean platelet volume
is used for measurement of platelet diameter indicating platelet
activation. Large platelets are more reactive than small ones and
are more likely to cluster to induce thrombosis. The function of
platelets often depends on their size. Mean platelet volume better
indicates platelet activation than platelet count [23]. Furthermore,
MPV has been shown to have an important prognostic role in many
malignancies such as gastrointestinal tumors, colorectal cancer,
and lung cancer [24,25]. High PLR has been known from previous
studies to be a poor prognostic factor in cancer [6]. It was supposed
that use of MPV, a better indicator of platelet activation, instead
of platelet count in PLR would be more indicative in determining
prognosis.
This study is the first to investigate the effect of MPVLR on survival in metastatic colon cancer. In our study, the cut-off point of MPVLR for overall survival was estimated by ROC curve analysis. We determined cut off point for MPVLR as 5.4. High MPVLR was found to be a poor prognostic factor in patients with metastatic colon cancer. Survival was shorter in patients with high MPVLR. The limitations of our study were its retrospective design, and the fact that although undergoing bevacizumab, cetuximab, or panitumumab regimen according to KRAS and NRAS status, patients did not receive the same treatments due to not having the same mutation. As a result, MPVLR analysis before treatment, can be used in patients with metastatic colon cancer as a cheap and easily available prognostic marker.
For more Articles on : https://biomedres01.blogspot.com/


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.