Transperineal Prostate Biopsies Under Local Anesthesia: Initial Experience
Introduction: Prostate biopsies (PB) are commonly performed using a transrectal approach under local anesthesia (LA). However, serious infectious complications can occur. The aim of our work was to evaluate the feasibility and safety of transperineal PB under LA.
Method: Between September and December 2020, all patients who had an indication of PB were offered to undertake it using a transperineal approach under LA. We proposed systematic biopsies, and additional targeted biopsies for patients presenting a target on pre-biopsy MRI (PIRADS≥3). The level of pain was evaluated using an analogic scale. Duration of procedure and adverse events within 30 days were also collected, as well as the results of biopsy cores histological analysis.
Results: 19 patients were included during the period. Median duration for the LA procedure was 13 [10-16] min, using a median volume of 65 [10-16] mL of Lidocaïne 0,5%. Median duration of the biopsy procedure itself was 12 [10-15] min. Median maximal level of pain was 3/10 [2;5]. A prostate cancer was diagnosed in 15 (79%) patients. No complication was reported during the 30 days following PB.
Conclusion: Our initial experience suggest that transperineal PB are feasible and safe under AL.
Keywords: Prostate Cancer; Prostate Biopsies; Transperineal; Local Anesthesia
Abbreviations: EAU: European Association of Urology; PB: Prostate Biopsies; LA: Local Anesthesia
Introduction
Since their initial description in the early 1980s [1], echoguided PB has been commonly performed by the transrectal approach. The transperineal approach has been rarely proposed - even though many reports suggested its non-inferiority in terms of diagnostic performance [2-5] mainly because of the poor tolerance, requiring general anaesthesia and thus hospital management. Despite antibiotic prophylaxis with oral fluoroquinolone, the main complications of transrectal PB are acute prostatitis, reported in 2.8% of cases [6]. Several publications recently suggested that severe post-PB sepsis rate increased over the past decade [6,7]. In addition, some reports suggested an increase of fluoroquinolone resistance, leading to a higher mortality rate [7-9]. Several solutions have been proposed to reduce the risk of sepsis, such as rectal disinfection [10] or the systematic performance of prebiopsy coprocultures in order to adapt the antibiotic prophylaxis to each individual case. Coproculture is now recommended by the European Association of Urology (EAU) for patients at risk of sepsis [11], but this organization in routine care limit the adherence of urologists to this practice. The transperineal approach could be an alternative to reduce this infectious risk.
The transperineal approach has received renewed interest in recent years due to the development of focal treatments for prostate cancer, which are performed mostly by transperineal approach [12]. Using the same approach for diagnosis, characterization and then treatment may be more relevant. Furthermore, the development of fusion and biopsy guidance software has made the technique of targeted PB reliable and accurate, regardless of the approach, transrectal or transperineal [13-17]. The main obstacle to the widespread use of transperineal PB remains its poor tolerance, which has motivated its use under general anesthesia until now. We have recently started our experience in performing transperineal PB under LA, in consultation. The objective of this work was to report the feasibility and tolerance of these PBs, performed by a single operator, during the first three months of his experience.
Patients and Methods
Patient Selection
Since November 2020, all patients with an indication for prostate biopsies in our center were offered transperineal biopsies under local anesthesia as an alternative to the transrectal approach. This work reports the initial experience, over a three-month period, of a single operator. In case of a suspicious image on MRI (PIRADS score 3), targeted biopsies were performed in addition to systematic sampling.
Technique
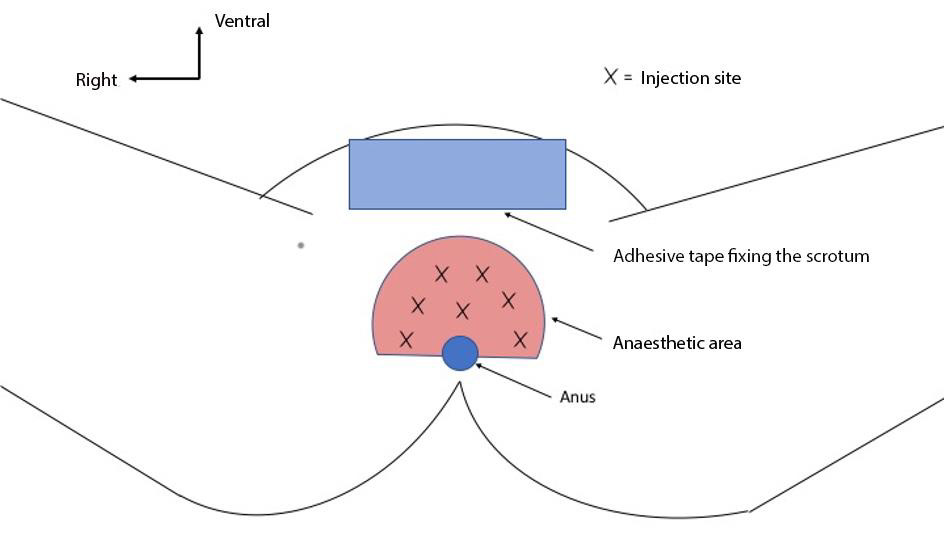
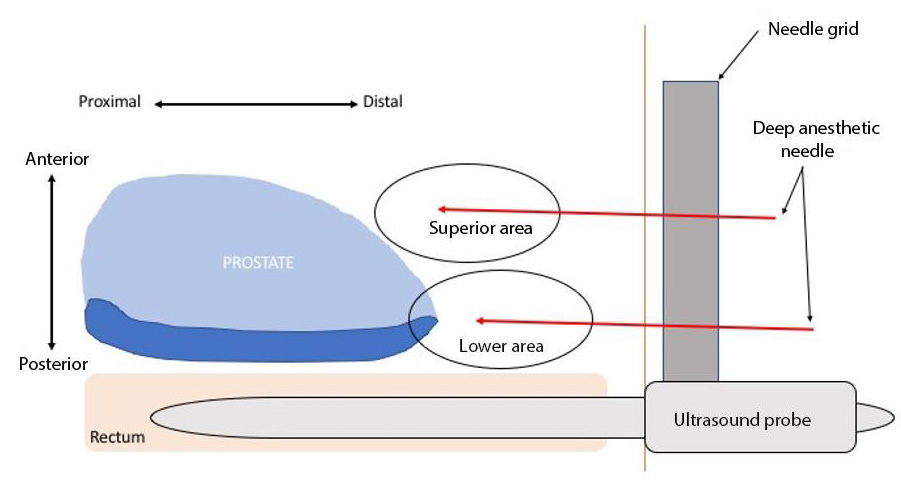
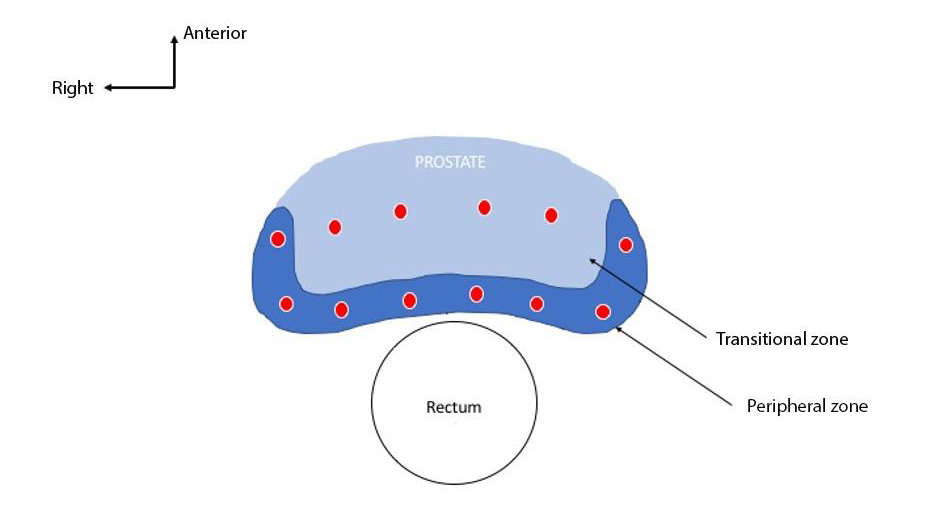
All patients received antibiotic prophylaxis with Ofloxacin in a single dose of 200 mg per os. A rectal enema was performed a two hours before biopsies. The biopsies were performed in a consultation room. The patient was installed in the gynecological position. The articulated arm used to stabilize the probe was attached to the examination table. A 0.5% lidocaine solution was prepared by diluting 40mL of 1% lidocaine in 40mL of saline. Subcutaneous anesthesia was performed by injection of approximately 10 mL of lidocaine solution. The area of anesthesia extended in a hemi-disc, centered on the anus, of approximately 5 cm radius (Figure 1). After skin anesthesia, the ultrasound probe was inserted, after having been attached to the stabilization arm. The anesthesia of subcutaneous tissues was performed under ultrasound control using a Chiba 22ga needle of 20cm length. During the progression of the needle from the subcutaneous tissues to the prostate, an injection was performed approximately every 5 mm. After injecting the lidocaine solution in the lower medial sagittal area, the injection was repeated in the upper medial sagittal area (Figure 2). The same protocol of injections was repeated in the left para-sagittal area and then in the right para-sagittal area, for a total of 6 injection points of local anesthesia. In patients with an MRI target of PIRADS≥3 score, the operator started with 3 to 4 targeted biopsies. All patients underwent systematic biopsies (Figure 3).
Figure 1: Median sagittal section diagram of subcutaneous anesthetic areas during transperineal biopsies under local anesthesia.
Data Collection and Analysis
All data were collected prospectively. The different stages of the procedure were timed. The maximum level of pain was assessed during the procedure and 1 minute after the last biopsy, using a numerical scale ranging from 0 (no pain) to 10 (maximum pain possible according to the patient). Categorical variables were described in terms of absolute numbers and percentage, n(%). Quantitative variables were described in terms of median, expressed with the first and third quartile, m[q1; q3].
Results
Characteristics of the Population
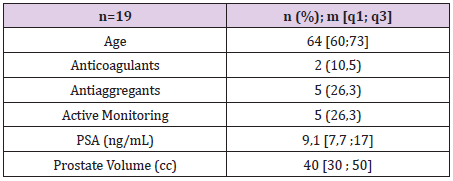
19 patients were included. The characteristics of the population are summarized in Table 1. The 5 patients under active surveillance protocol had PBs at least 6 months before the procedure.
Table 1: Characteristics of the population. Proportions are expressed as absolute numbers and percentages -n(%)- and continuous variables as medians -m[q1; q3].
Data Collected During the Procedure
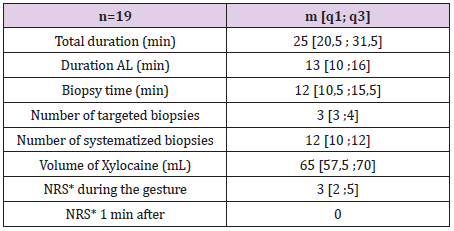
All procedures were performed completely using the transperineal approach, without any adverse event. No conversion to transrectal biopsy was required. The data collected per procedure are summarized in Table 2.
Table 2: Data collected during the biopsy procedure.
Note: *NRS: Numerical scale evaluating the patient’s pain, rated from 0 to 10.
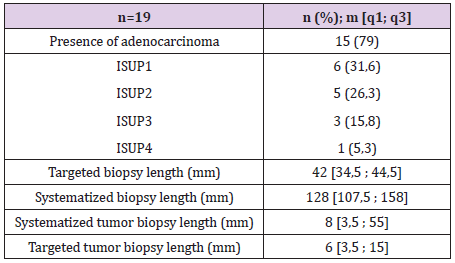
Histological Analysis
Prostate cancer was diagnosed in 15 (79%) patients. The results of the histological analysis are summarized in Table 3. No Clavien-Dindo≥2 score complications were reported within 30 days. No unusual symptoms were reported.
Discussion
Our preliminary results suggest that transperineal prostate biopsies are feasible, with a good tolerance, in a consultation setting. No procedure had to be interrupted, and no adverse events were observed. Subsequently, no Clavien-Dindo>1 complications were reported by patients within 30 days. The median maximum pain reported during the examination was 3/10 [2;5]. These results seem comparable to these obtained with transrectal approach. Indeed, a study of nearly 200 patients rated the median pain of transrectal biopsies at 2.5 on a similar scale [18]. These results also seem comparable with recent series evaluating the transperineal approach under local anesthesia, with scores ranging from 2/10 to 5/10 [19-22]. Even if this median score of 3/10 seems acceptable, we observed heterogeneous results. Indeed, one patient reported a pain score of 6/10 and three other patients reported a score of 5/10. These pain scores do not seem acceptable for this type of diagnostic examination, and a larger study should confirm that these are exceptional situations, or related to the beginning of the experiment.
In addition, two patients felt no pain and two others felt very little pain at 1/10. These cases confirm that the analgesia technique used can be totally effective and allow a comfortable procedure. The patients who reported pain at some point of the procedure felt it mainly during the local anesthesia. The most painful moment was the introduction of the needle through periprostatic tissues. The majority of patients in our study described no pain at the time of biopsy punctures, and no pain after the procedure. These results are concordant with recent studies, which suggest the anesthetic procedure as the potentially painful stage of the procedure [19-22]. In addition, two of the three patients who previously underwent transrectal biopsies (active surveillance), reported less pain during transperineal biopsies compared to transrectal appraoch. One of the questions that currently arises is the comparison of the tolerance of the two approaches. To our knowledge there are no comparative trials in the literature.
Even if pain is probably the main point of the evaluation of the tolerance of the technique, the length of the procedure seems to us just as relevant, for the comfort of the patient, and on a larger scale in terms of accessibility of care and overall cost. In our study, the median length of the procedure was 25 [20 ;31] min. The duration was more than 30 min at the very beginning of our experience and then about 20 min for the last procedures. The recent work of Marra et al. also evaluated the length of procedures using a similar technique in 450 patients [19]. The median duration was 18 [15;22] min. It is therefore likely that the experience of the operator allows the duration of the procedure to be reduced, and thus optimizes patient comfort. The median duration of the LA procedure, was 13 [10;16] min, which corresponds to about half the duration of the procedure. In our experience, we observed that an AL procedure lasting less than 10 min did not provide optimal analgesia. This may reflect the minimal time required for effective analgesia, which could be explained by the time delay of action of lidocaine. In the work of Marra et al, the median duration of the anesthetic procedure was 3 [2;4] min, which could explain a high median pain of 5/10 [19].
One of the potential advantages of the transperineal approach is reduction of infectious risks. This risk is about 3% [6], it is greater in patients having iterative biopsies, which are nevertheless necessary in the context of active surveillance protocols, or surveillance after focal treatment [15]. In the series by Marra et al. the authors did not report any infection. The patients were nevertheless treated with fluoroquinolones, which may be debatable given the absence of rectal puncture. Another study that evaluated a series of 577 patients who received cephazoline as a single dose did not report any cases of post-biopsy prostatitis [15]. Finally, a smaller series of 45 patients who received no antibiotic prophylaxis reported no cases of infection [23]. A recent report using Norwegian social security data showed an increase in mortality related to infectious complications of prostate biopsies related to fluoroquinoloneresistant E. coli. The Oslo University Hospitals are now in the process of changing their PB protocol in favor of the transperineal approach [8].
Only a prospective randomized study will confirm that transperineal PB without antibiotic prophylaxis reduces the risk of infection compared to transrectal PB with antibiotic prophylaxis. No patient in our study had urinary retention. Other series report a low rate, less than 1% [21,22]. It is possible that this difference could be explained by a our relatively limited population . Other series have reported rates above 1%, but the procedures were performed under general anesthesia, which independently increases the risk of retention [15]. The main limitation of our study is related to the small number of patients. Our work was designed to evaluate the technical feasibility, and therefore does not present sufficient data to evaluate the infectious risk, nor the biopsy yield. Nevertheless, it allows us to conclude that transperineal PB under LA is feasible, and that the initial experience is not associated with a particular risk for the patient. The surgeon had a short training with another experienced surgeon before starting his own procedures. The experiment went on without any accidents, conversions, or adverse events.
Conclusion
Our results suggest that transperineal PB under LA is feasible and safe, in consultation, from the initial learning period.
For more Articles on :https://biomedres01.blogspot.com/


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.