Paroxysmal Supraventricular Tachycardia and Atrial Fibrillation in the Same Patient: What Seems to be the Link?
Introduction
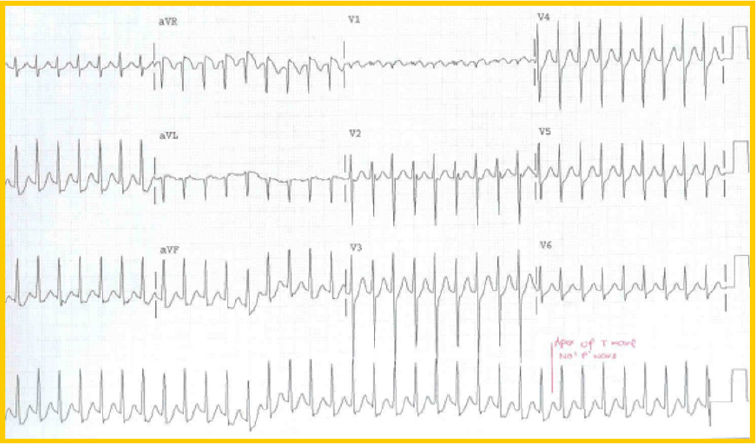
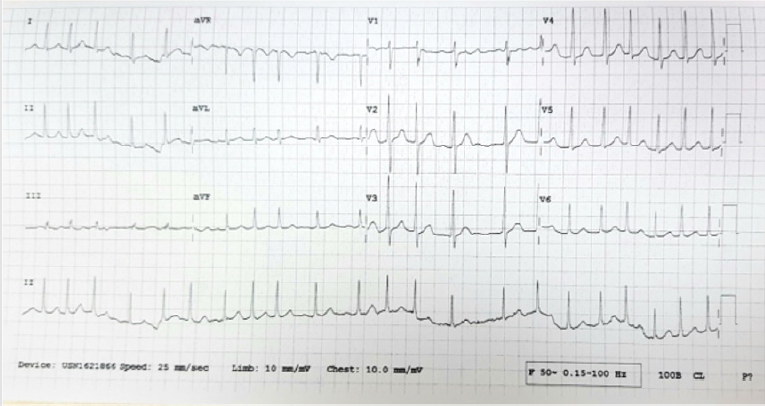
Imagine that you are the emergency physician on duty and a 56-year-old patient, with no past medical problems, presents with palpitations. It has been ongoing the last hour and the patient feels slightly light-headed but had not experienced any episodes of fainting. The nurse performs the 12-lead electrocardiogram (ECG) and shows it to you (Figure 1). You make the diagnosis of Paroxysmal Supraventricular Tachycardia (PSVT) and go on to take a rapid history from the patient, as your resident inserts a large bore cannula and collect some blood for investigations. As you instruct your nurse to prepare the drug Adenosine to be administered to the patient, your resident glance at the cardiac monitor and alert you that the rhythm has changed. He commented that the patient’s pulse is irregularly irregular now. The Blood Pressure was 162/ 89. Your nurse repeats the 12 lead ECG (Figure 2). It has indeed converted to Atrial Fibrillation (AF). You update your nurse that you will not be needing the Adenosine any further in view of the change in rhythm. As you have never encountered such a case before, you wonder what the underlying etiology and mechanism of both PSVT and AF is occurring in the same patient, within such a short span of time.
Supraventricular Tachycardia (SVT)
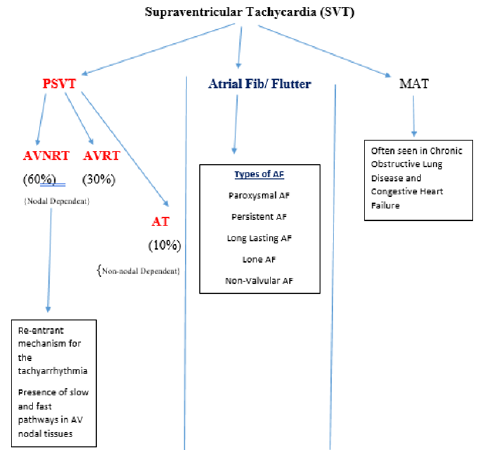
SVT is a tachyarrhthmia with its origin above the Bundle of His. It can be divided into three broad groups: PSVT, AF and multifocal atrial tachycardia (MAT). 60% of the PSVT is atrio-ventricular nodal re-entrant tachycardia (AVNRT), 30% atrio-ventricular reciprocating tachycardia and 10% are atrial tachycardia in nature (Figure 3). As it is, AF and atrial flutter are also classified as SVT [1-4]. Therefore, with reference to our case above, is it possible for a patient to have an inter-change of rhythms or a conversion of rhythms from PSVT to AF (both being different forms of SVT)? If this is the case, then what will be the mechanism involved?
Mechanisms and Postulations: PSVT and AF
There are currently some evidence as well as postulations that have been put forth in the literature to explain the phenomenon observed. Some of these are discussed below:
1. Currently it is noted that the atrioventricular accessory pathway (also known as the slow pathway) is involved in the genesis of AF. The phenomenon of enhanced atrial vulnerability can lead to the degeneration of AVNRT to AF. Here it is thought that during PSVT there is disturbance in the atrial electrophysiology, and this may be the mechanism of initiation of AF, when the slow pathway becomes activated [8,9].
2. During PSVT there is increased atrial refractoriness and as a result of the mechano-electrical feedback paroxysmal AF can be initiated [9-11].
3. There is also a postulation that increased atrial dispersion from increased stretch during PSVT can induce AF. Increased size of the atrial has been correlated with enhanced tissue vulnerability and thus the predisposition to AF. The change in size and pressure of the atria during PSVT creates electrophysiologic changes which can generate AF [10-12].
4. There is also a suggestion that genetic polymorphism predisposes patients to both arrhythmias (i.e.. AVNRT and AF) [12].
5. Some authors have reported that a significant proportion of patients coming for AF ablation are inducible for SVT. Alternatively, others have observed that SVT ablation in their patients showed a preventive effect on AF occurrences in patients with documentation of having both arrhythmias [5, 13-15].
6. Others have reported direct observations that synchronized tachyarrhythmias (atrial flutter, ANVRT, AVRT) can trigger AF [15,16].
7. It is also thought that the transition from AVNRT to AF may begin in the pulmonary vein area. The pulmonary veins’ myocardial sleeve, which is an extension of the left atrium, is thought to be potentially arrhythmogenic [17-19] The AF will continue if the reentrant wavelets continue roving through the atrial tissue. On the other hand, there have also been some postulates that there are non-pulmonary vein (NPV) triggers that may be responsible for persistent AF. The mechanism for this it appears may be due to the combination of reentrant and enhanced automaticity pathogenesis. Some have also gone on to observe that there is the left atrium NPV and right atrium NPV tissues and one may be more likely to be the causation of AF in each individual patient [20-24].
Conclusion
As there are multiple explanations and postulations for the possible link between PSVT and AF happening, as in the scenario we started with, it would be evident that the exact causation remains controversial and nebulous. The causation is likely to be multifactorial. In the meantime, as clinicians, it is good to be aware of this and deepen our understanding of why certain drugs are recommended for their therapy and management. It may shed some light on what mechanism/s are being targeted.
For more Articles on : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.