A Unique Case of Rehabilitation of a Young Girl with a Bilateral Above the Knee Stumps and Spina Bifida
Introduction
Prosthetics after amputation of the lower extremities is a complex problem in the medical and social rehabilitation of patients. The higher the level of amputation, the more difficulties encountered in the manufacture of leg prostheses. However, only with the help of prostheses, the patient will be able to stand and move independently, using aids. According to [1], 50,000 amputations are performed annually in Russia. Of these, 51% - for obliterating diseases of the vessels of the lower extremities, 26.2% - for diabetes mellitus. Thigh amputations account for 61.5%, of which paired thigh amputations account for 59%. It is known that after amputations of the lower extremities in 70% of cases, there is a presence of vicious stumps, including those complicated by pain. In addition, the higher the level of amputation, the more difficulties are encountered in the manufacture of a prosthesis in which the patient can move independently or use aids for walking [2]. Combinations of leg amputation with congenital malformations of the musculoskeletal system and, in particular, the spine, for example, Spina bifida, are especially difficult. The most common and significant clinical form of Spina bifida is myelomeningocele (MMC), in which a hernia forms with the involvement of the membranes and tissues of the spinal cord [3-8]. The condition, which occurs in about 1 child in 1000 newborns [9,5]), is characterized by the inability of the lumbosacral spinal neural tube to close during embryonic development.
Exposed nerve tissue degenerates in utero, resulting in various neurological deficits and varies with the level of lesion [3,5,10]. In this form of Spina bifida, a part of the spinal cord emerges through the spinal defect in the form of a “pouch” with the spinal cord [11]. It can be covered with skin, in other cases, the brain tissue itself and nerve roots can go out, and the very severity of neurological manifestations and disorders will be associated with the localization and severity of the spinal cord defect [12]. Myelomeningocele (MMC) affects the quality of life in childhood, adolescence and adulthood, making it difficult for individuals, families and society as a whole [3,13-20]. And this is due to the fact that non-infection in 80% of cases is accompanied not only by paralysis of the legs, but also by dysfunction of the bladder and intestines [8]. Despite these problems, sick people are preserved intellectually or emotionally. They also go to school, study at institutes, want and can play sports. In Russia there are a world champion in fencing, the 37th world tennis player, a member of the Russian Paralympic ski / biathlon team, a champion of Russia, there is a world champion in wheelchair dancing in 2015 [16]. For the treatment of the defect, as a rule, surgical correction is used, in most cases immediately after birth [21,22]. However, in recent years in Russia, the United States and other countries intrauterine correction of Spina bifida in the fetus has been widely used [23-28].
It reduces the risk of ventriculoperitoneal shunting and increases the level of cognitive and motor development compared with the post-natal treatment group. We consider the rehabilitation of patients with a similar injury to the spine and with vicious paired amputations of the lower extremities at above the knee level to be the most difficult. To put the patient on his feet, atypical prostheses should be made, including non-standard sockets for primary prosthetics. Primary prostheses are made primarily in order to form the volumetric dimensions of the stumps. They also restore support, teach the patient the principles of virtualization, balance, and movement over short distances. Material and methods. A clinical example of successful rehabilitation of a 26-year-old female patient is presented, with depressed amputation stumps of both thighs in the middle third and flexion contractures in the hip joints at an angle of 15 degrees in combination with Spina bifida (The case from my work in 2015, in the “Russian Scientific Center” Restorative Traumatology and Orthopedics them. acad. G.A. Ilizarov “, Kurgancity, Russia (director - A.V. Gubin, MD). In connection with Spina bifida and paralysis of the lower extremities, accompanied by also severe deformities of the both feet, the patient underwent above the knee amputation at the age of 14 years at the place of residence. Later she lived in one of the orphanages in Russia, moving only in a wheelchair.
Prolonged sitting in a wheelchair led to the development of contact osteomyelitis of the right half of the pelvic bones. It can be assumed that urinary incontinence played a role in the development of osteomyelitis. The ischial bone was also involved in the inflammatory process, namely, it serves as the main supporting landing site for the stump in the socket of the above the knee prosthesis. It was decided to preliminary prepare for prosthetics by step-by-step surgical treatment. At the first stage, specialists of the Department of Purulent Orthopedics (Dr. S.V. Mukhtyaev) performed reconstruction of the right ischium, necrectomy of sequestration, ultrasonic cavitation of the wound, drainage, with positive dynamics of treatment, and wound healing by primary intention (Figures 1-3).The second stage, together with neurosurgeons (S.O. Ryabykh, D.M.Savin, A.A. Koryukov).From the point of view of morphology, the macro preparation was represented by a rounded soft tissue formation (fat pouch) up to 6 cm in size, on the cut, brown-yellow tissue covered with skin up to 13 mm thick. The material contains fragments of thin skin with signs of papillary mutilation (Figure 4). The fragment contained adipose tissue with bundles of atrophied skeletal muscles, which should normally be absent. The presence of signs of skeletal muscle atrophy indicated a possible gradual degeneration due to the lack of normal function.
Figure 1: Photo of the dorsal surface of the patient’s pelvis before treatment. The area of skin lesion in the area of damaged pelvic bones by contact chronic osteomyelitis is visualized.
Figure 2: On radiographs of the pelvic bones, there is a heterogeneous structure and uneven contours of the ischial bones, confirming the presence of chronic osteomyelitis.
Figure 3: Reconstruction of the pelvic bones and sequestrectomy of the affected areas of the bone, ultrasonic cavitation and excision of the changed skin with the imposition of postoperative sutures were performed.
Figure 4: Influence of Methanolic Extractives of Prepupal Stages of Black Soldier Fly (MEPSBSF) on Activity of Asparateaminotransferase (AST) Alanine aminotransferase (ALT) and Lactate Dehydrogenase (LDH) in Serum in DMBA Induced Toxicity in Norwegian Rat, Rattus norvegicus (L).
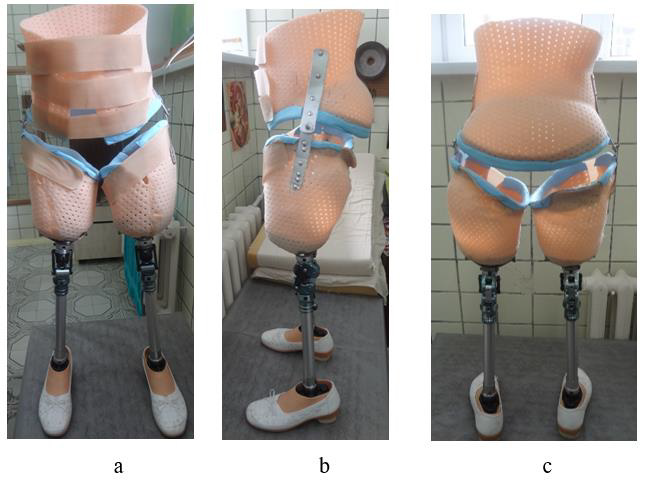
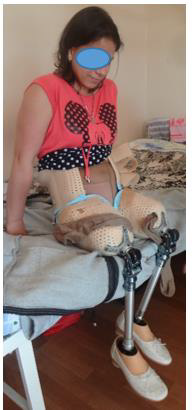
After the healing of the postoperative wound in the lumbar region, a stage of restorative treatment was performed (special packing for extension in the hip joints, the application of elastic bandages on the above the knee stumps, exercises aimed at strengthening the muscles of the trunk and limbs). The patient was prepared for the production of express above the knee prostheses and spine orthoses (A.A. Koryukov, A.V. Reznik, S.P. Pukhov). Individual receiving sleeves made of thermoplastic, connected by means of hip joints with a rigid lumbar corset, ensured structural rigidity and stability of an upright position when walking (Figures 5a-5c). Such an assembly was necessary due to the long-term lack of support, the presence of small flexion contractures in the hip joints, and weakness of the back muscles. The stage of fitting the socket and corset, learning to walk on prostheses took about 2 weeks in total. The patient quickly mastered walking with prostheses, and therefore knee modules were installed in her 10 days later. The walking pattern has become more physiological. In addition, due to the bending of the legs in the knee joints, in prostheses, if necessary, it was possible to sit down (Figure 6). While walking, the woman leaned on a walker, and in the future she was recommended to use other available means - crutches with armrests and walking sticks (Figures 7a-c to 8).
Figure 7: The patient’s appearance in prostheses at the stage of mastering walking
a. Back view and
b. b-c: Front.
Conclusion
1. In non-standard, atypical situations of pathology of the musculoskeletal system, stage-by-stage medical preparation for prosthetics is required, including various types of surgical treatment.
2. The use of modern thermoplastic materials, even in a hospital, makes it possible in a short time to make any individual therapeutic and training prostheses.
3. For the first time in many years, the patient was able to move independently and improve the quality of life.









No comments:
Post a Comment
Note: Only a member of this blog may post a comment.