The Two-Way Link Between Diabetes Mellitus and Periodontal Disease: Medical- Healthcare Professionals’ Clinical Practice
Introduction
Although the notion “Oral health and general health are inseparable” is most frequently and widely narrated in the scientific literature, it has not infiltrated well enough into the medical community. Quite understandably, since the beginning, there is a dental-medical divide that has not been closed, and it is not going to change anytime soon as these two disciplines are also structurally separated. Diabetes mellitus and periodontal disease are global epidemic ailment with severe health consequences. Medical professionals provide primary care to patients with diabetes mellitus for their general health needs. Periodontal disease, along with other complications, has been suggested as the sixth most common complication of diabetes mellitus [1,2]. Furthermore, recent evidence confirms the mutual and bidirectional relationship between periodontal disease and diabetes mellitus [3,4] which means that severe periodontal disease adversely influences the glycaemic control in persons living with diabetes and vice versa [5-7]. Hence, logically, persons living with diabetes require collaborative care by medical and dental professionals for their health needs [8,9]. However, worldwide, this is not actively practised or even considered in most of the instances [10].
The recent statistics on Australian healthcare workforce (2015) reports around 392 fulltime medical providers per 100,000 populations [11]. According to the current data from the Department of Health, Australia (2018), there are around 98,400 medical practitioners and 20,600 dental healthcare practitioners registered with AHPRA. This number is around 5.5 times more than oral health professionals, where only 72 oral healthcare professionals are available to look after 100,000 individuals [12]. Among them, nearly 85% of dentists work in the private sector. Australian Institute of Health and Welfare (AIHW) also reports that during 2016-17 approximately 70,200 patients were hospitalised due to dental complications that could have been avoided with timely treatment [13].
Inter-professional collaboration between medical and oral health professionals have been implicated in the effective prevention and management of diabetes-related complications. Such coordinated care is challenging as it is dependent on multiple providers across different disciplines. The critical aspect of this care is the allied knowledge of the disease (periodontal and diabetes) by the disciplines involved. This knowledge includes but not limited to the aetiology, pathogenesis, associated risk factors, and the management strategies of the particular disease. Recent evidence suggests that medical professionals, including general medical practitioners, specialists, nurses and allied healthcare workers, do not receive any training and knowledge in oral health, resulting in poor understanding of oral health problems [14].
A study reported developing an inter-professional learning tool for qualified pharmacists, nurses, healthcare assistants and junior doctors to improve care for the persons living with diabetes [15]. The study completely overlooked the importance of involving oral healthcare professionals to manage patients with diabetes mellitus. In contrast, Silk, [16] suggested that a comprehensive approach can achieve improved oral health outcomes. This holistic approach involves improving oral health literacy and practice in patients, learning new skills by medical and dental professionals and adopting a collaborative approach in patient management. In this regard, a recent systematic review noted that one-third of medical professionals were unaware of the relationship between oral health and diabetes. Only 30% reported referring their patients for an oral health assessment to dentists [17]. They also highlighted the importance of inter-professional education for medical and dental professionals. The literature regarding medical professionals’ knowledge, attitude, and practices of diabetes mellitus and periodontal disease from Australia is missing. Therefore, the study investigates medical professionals’ understanding of the link between periodontal disease and diabetes mellitus in a cohort of medical professionals practising in Australia.
Methodology
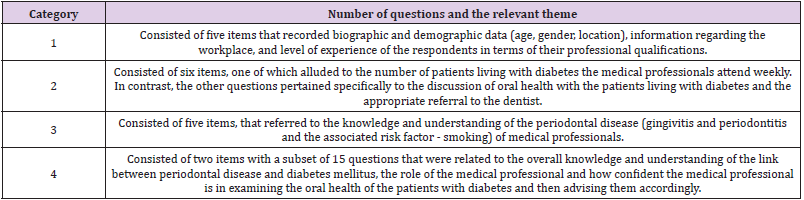
A convenience sample of medical professionals participated in this pilot study to complete an 31-item questionnaire. A power calculation was not necessary for this pilot study. An online survey was designed to investigate the knowledge and understanding of periodontal disease (gingivitis and periodontitis) and the link between periodontal disease and diabetes mellitus. The questionnaire was created with the help of a panel of experts that have experience in research methods to assess the relevancy, clarity, simplicity and necessity of the questions. The panel conducted the content validity of the survey questionnaire for appropriateness. The survey questions were finalised after completing the systematic review of the literature investigating the medical professional’s knowledge and understanding of the link. Five medical healthcare professionals also did the initial piloting of the questionnaire before disseminating the questionnaire. The ethical approval was obtained from the institutional Human Research Ethics Committee (HREC – CSU, approval # H16154). The survey invitation with the web link was available to the medical practitioners for a period of four months. Medical healthcare professionals were also contacted by the authors at their practices in a face to face meeting requesting to participate in the research. A reminder to complete the survey questionnaire was also circulated after one month. The questionnaire consisted of four categories (Table 1). Most items were in multiple-choice format, with options of “other” where the participants could elaborate further in text free fields if they deemed appropriate. Some questions also had the option of selecting multiple choices with the possibility of reporting others.
Study Sample
The study’s inclusion criteria dictated that participants had to be a practising general and/or specialist medical practitioner registered with the Australian Health Practitioner Regulation Agency (AHPRA). The survey was anonymous, and the responses of the participants were not identifiable.
Data Analysis
The responses were collated electronically on Qualtrics and transferred onto an Excel® spread-sheet (Microsoft Corp., Redmond, Wash., USA) and analysed using a commercially available statistical software package (IBM SPSS® Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). The bivariate analyses using Fisher’s Exact and Chi-Square Test (in SPSS® 27) were utilised to analyse whether participants’ awareness regarding periodontal disease and the bidirectional association was associated with educational level and their clinical practice. A p-value of <.05 was considered to be statistically significant. The output of data was presented in a table format (total responses and percentage) and a graphical format.
Results
Category 1: Demographic and Diabetes Care Data
A total of 46 medical professionals completed the survey (response rate of 64%). Male to female ratio was 3:1, and their age ranged from 24-64. Over 82% of the participants reported providing services at the general medical practices, while 6.5% providing services at the hospitals and specialist practices.
Category 2: Data on the Discussion of Oral Health with the Patient Living with Diabetes and the Appropriate Referral to the Dentist
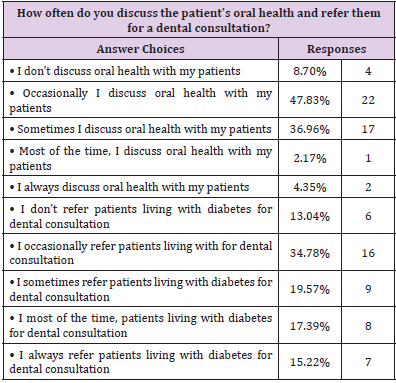
Just over 40% of the participants reported seeing 6-10 patients living with diabetes per week. This figure ranged to 8.70% (for more than 30 patients per week), 6.52% (26-30 patients/week), and 19.57% (for 16-20 patients per week) respectively. Concerning the oral health discussion with the patients living with diabetes, around 48% of participants occasionally discussed oral health during their consultation. While 37% of participants reported, some times and only 4.35% of participants reported always discussing oral health with their patients. On the other hand, around 9% of medical professionals never discuss oral health with their patients living with diabetes. When asked regarding the referral for the dental consultation, the response rate showed a similar trend, with only 15.2% always refer to a dental checkup, and 13% don’t refer their patients at all (Table 2). Similarly, only 15.22% of participants reported insisting their patients seek dental consultation. Just over 42% occasionally and 17.78% sometimes ask on their patients for a dental visit. Only 4.44% of participants always insist on their patients to see a dentist (Table 2).
Table 2: The frequency of patients living with diabetes with whom medical professionals discuss oral health and made the referral for a dental consultation.
Category 3: Data on the Fundamental Understanding of Periodontal Disease (Gingivitis and Periodontitis)
In the third category of survey questions, participants responded to some basic oral health/periodontology related questions. The questions were about understanding the periodontal disease, including gingivitis and periodontitis and the associated risk factors, for example, smoking). In response to the description of gingivitis, most of the participants (54.35%) opted inflammation in the marginal gum area that is reversible, while 26% selected gingivitis as an infection of the gums. In response to the first sign of gingivitis, bleeding gums was correctly indicated by 78.26% participants, while, around 21.74% attributed bad breath as the first sign of gingivitis. Just over 60% of the participants ticked smoking as a relevant factor in gingivitis and approximately 24% to glycaemic instability and 13% to diet high in carbohydrate. Around 2% of participants also attributed this to old age. When the distinction between gingivitis and periodontitis was asked, 56% of participants correctly selected bone destruction around teeth. At the same time, 26.67% still considered it as an inflammation in the marginal gum area that is reversible. Around 13% of participants thought periodontitis as the infection of the gums.
Category 4: Data on Overall Knowledge and Understanding of the Link between Periodontal Disease and Diabetes Mellitus
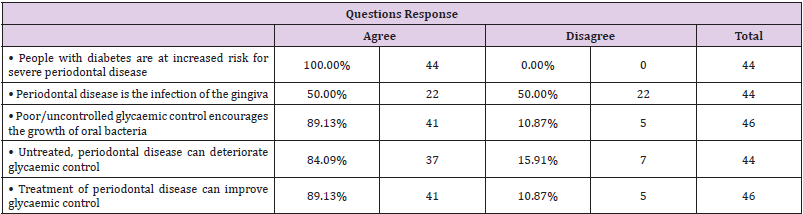
In the fourth category, the knowledge of the bidirectional association between periodontal disease and diabetes mellitus was evaluated. All participants agreed that people with diabetes are at increased risk of having severe periodontal disease. Majority of participants (89%) selected the option that poor/uncontrolled glycaemic control encourages the growth of oral bacteria. Similarly, 89% of participants agreed on the statement that the treatment of the periodontal disease could improve glycaemic management (Table 3). Only 16% of participants agree with the statement that the research is inconclusive regarding the bidirectional relationship between systemic health and periodontal health. On the other hand, only 28% strongly agreed that the association between periodontal health and diabetes is a reality, while, 31% of participants opted unsure for this statement. Regarding the question on the awareness of the recent literature on diabetes and periodontal relationship, only 34% of the participants chose to agree or strongly agree with the statement. In contrast, the rest (66%) selected unsure and disagree with the statement. Around 80% of the participants agreed/strongly agreed with the statement that patients with poor glycaemic control are more likely to have poor oral hygiene and periodontal disease. Majority of the participants (85%) agreed upon having a close collaboration with the dental practitioners to reduce their patient’s risk of developing periodontal disease, On the other hand, around 14% participants were still unsure about it (Table 4).
Around 80% of participants showed an interest in more education regarding patients’ periodontal health with diabetes. In response to the question regarding conducting oral health examination of their patients, almost 40% of the participants disagree with the statement. Only 42% were confident in doing oral health examination of their patients (2.63% strongly agree, and 39.47% agree). Around 40% of the participants were of the view that homecare measures could manage severe gum diseases. On the other hand, 32.5% of the participants were uncertain to answer this question. Just over 75% of the participants showed interest in including an oral health component in diabetes continuing education, while 25% opted unsure to answer this question. Missing values at random were below 2% hence were ignored.
Table 4: Response to questions concerning oral health and its impact on patient’s health and its related evidence.
Discussion
The results of the pilot study demonstrate higher understanding and awareness of the bidirectional relationship between diabetes mellitus and periodontal disease among this cohort of medical professionals. Majority of the medical practitioners (89%) knew that by providing periodontal therapy, the glycaemic index of patients living with diabetes (having the periodontal disease) could be improved. Similarly, a higher number of participants (93%) agreed with the statement that “Good oral health is vital to the overall wellbeing of the patient”. However, when asked regarding the recent literature on the bidirectional relationship between systemic health and periodontal health, only 40% responded correctly. Around 25% of the participants acknowledged that they are unaware of the recent literature regarding diabetes and periodontal health.
A range of outcomes has been reported by other studies that have investigated the knowledge and awareness of medical professionals regarding the bidirectional association between periodontal health and diabetes mellitus. Owens and colleagues [18] noted around 66% of endocrinologists agreed with the statement that the treatment of the periodontal disease might improve glycaemic control. Similarly, almost 74% of the medical professionals agreed with the above statement in the study by Bahammam [19]. In the present study, a higher number of medical professionals (89%) responded positively to this statement.
These outcomes demonstrate a gap between awareness/ knowledge and evidence-based clinical practice. Medical professionals are aware of the association between periodontal disease and systemic health, but they are not convinced. This lack of confidence is mainly due to the absence of appraisal of the topic’s pertinent literature. This is evident by the fact that majority (82%) of the medical professionals showed interest in more education regarding periodontal health of patients with diabetes and around 75% of participants agreed on including an oral health component in diabetes continuing education. Similar findings have been reported by other studies like Obulareddy, et al. [20] (90%) and Owens, et al. [18] (88%) that have shown interest of medical professionals in oral health education and training. This lack of confidence is prominently reflected in their clinical practice as most medical professionals don’t discuss oral health with their patients on regular bases, nor do they refer their patients for the oral health/ dental assessment.
The study noted that a small percentage (15.2%) of medical professionals always refer patients with diabetes for a dental consultation. Gholami, et al. [21], on the other hand, reported a higher percentage of medical practitioners (95.8%) who refer patients with diabetes mellitus to the dentists for a consultation. A higher (100%) frequency of medical professionals that provide advice to their patients was noted in a recent report by Bahammam [19]. However, when the same cohort was asked about periodontal health information, only 56.5% deliver such information to their patients. Similarly, Owens, et al. [18] reported around 48.72% endocrinologists and 25% internists to refer their patients for dental consultation [18].
The results of the present study endorse the outcomes of the survey by Al-Habashneh, et al. [22] as they also reported the mismatch between the awareness of the bidirectional link and the clinical practice in their cohort of 164 medical professionals. However, the referral to the dentist was not found related to the knowledge or speciality status of the medical professionals in the present study as was found (direct relationship) in the survey by Al-Habashneh, et al. [22] They reported that specialists instruct and refer their patients living with diabetes more frequently to dentists compared with the general practitioners Lin, et al. [23] reported similar outcomes as around 77% endocrinologists reported in their study often referring their patients for a dental checkup.
Several studies have investigated medical professionals’ knowledge of oral/periodontal health. The present study found a moderate level of understanding and awareness of the periodontal disease among medical professionals. In this regard, 78.26% of participants knew the signs of gingivitis, while only 56% of the medical professionals were aware that periodontitis involves the destruction of the alveolar bone around the teeth. Al-Khabbaz, et al. [14] reported a lower level of understanding of alveolar bone loss in periodontal disease (39%) in their cohort of medical professionals. Owens, et al. [18] reported 92% of the participants, while the present study reported 54.35% of the medical professionals showed the understanding of gingivitis as the reversible inflammation of the gingival margin.
The outcomes of the present study highlighted a critical missing link “inter-professional education”. In health education, collaborative learning is a tool in which members of different professions learn together and from each other to improve patients’ quality of care (Centre for the advancement of interprofessional education - CAIPE) [14,22,23]. Recently, inter-professional education (IPE) has gained high importance in patient-centred care and has been included in most medical and dental curricula [16]. These courses and modules develop skills for complex patient needs and foster awareness of oral-systemic health interactions. These modules guide the professionals to institute inter-professional collaborative practise (IPCP) [16,24]. In this regard, medical-dental integration of the curriculum could provide the most favourable outcomes for the optimised care of patients with diabetes. The present study noted that medical professionals are quite welcoming to receive training in oral health examination and wants to improve the understanding of periodontal diseases.
The outcomes of the present study lead to the fact that if medical professionals are not fully equipped with the current literature (concerning diabetes mellitus and periodontal relationship) then ultimately patients under their care will not receive optimised preventive care. The information will not pass on to the patients, and hence both diseases will negatively influence each other. The results of the present pilot study should be interpreted carefully as they represent only a small percentage of medical healthcare professionals. The main limitations of the study are the low sample size, some unanswered responses, and the potential of unconscientious responses. Future research with the better methodological design that evaluates the barriers in the mutual and collaborative care of diabetes patients by medical professionals and the dental team should be conducted. Furthermore, the influence of information sources, medical healthcare professionals use to become informed and make clinical decisions should be explored. It is acknowledged that the bidirectional relationship between periodontal disease and diabetes is not causal. However, these two conditions strongly influence each other, mainly arbitrated by the hyper-inflammatory response [25]. The present study urged the need for effective collaboration between medical and oral healthcare providers to break professional silos for integrated disease prevention. The best example for the oral healthcare professionals, to follow, is the integrated oral health practice model that helps in the early detection of the disease by health screening and health promotion activities and instigating lifelong coordinated patient care with the support of medical healthcare professionals [26,27].
Conclusion
Within the limitations of the pilot study, it can be concluded that the investigated cohort is aware of the association between periodontal disease and diabetes mellitus. However, they are not fully convinced due to the lack of interactive forums that discuss such clinical management issues. Hence, this knowledge is not reflected in their clinical practice resulting in a low frequency of referral and communication with the dentist. It is the time medical professionals should realise the fact that “No health without oral health”.




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.