Effectiveness of Blood Flow Restriction Training in Patients Undergoing Knee Surgery
Introduction
BFRT involves restricting blood flow to a targeted muscle group whilst making it perform movements under low load resistance. The aim of this is to achieve the same effect that putting the muscle through High Resistance Training (HRT) would accomplish. HRT is often not possible in certain patients due to cases involving injury requiring knee surgery. In individuals without injury, there is already evidence that noteworthy improvements have been made to muscular hypertrophy, muscle fibre recruitment and endurance with BFRT (Takarada, et al. [4]). For healthy individuals, the American College of Sports Medicine recommends training with loads of 60–70% of their one repetition maximum (RM) for 8-12 repetitions to maximize muscular strength. However, for patients with knee pathology, performing movements with loads of 60–70% of their one RM may not be possible and could cause further injury (Buckthorpe, et al. [5]). Quadriceps and hamstring muscles often atrophy after anterior cruciate ligament (ACL) reconstruction surgery or whilst awaiting for the operation to take place. The intention of using BFRT with patients is to reduce the level of atrophy and weakness in muscles before and after surgery (Ferraz, et al. [2,5]). Despite successful ACL reconstruction surgery, many patients still suffer from poor function due to quadriceps muscle weakness. The impairment of the quadriceps muscle will often last for several months post-reconstruction. Loss of muscle and strength can lead to chronic asymmetry if not corrected. Chronic asymmetry, in turn, can lead to an increased risk of re-injury and early-onset osteoarthritis (DePhillipo, et al. [1]).
BFRT has been shown to build local muscle endurance superiorly in normal blood flow exercise. The reason for this is thought to be due to increased vascular function and muscle oxygenation. There is evidence that it reduces muscle atrophy for patients who had ACL reconstruction (Iversen, et al. [3]). However, there is also evidence suggesting that there is no effect (Harper, et al. [6]). In severe osteoarthritis, Total Knee Replacement (TKR) is the preferred option as it limits pain and aims to maintain the function of the lower limb. However, many TKR patients suffer from a long-term reduction in quadriceps strength and an overall substandard outcome thought to be related to the insufficient recovery of function. This issue is suggested to be correlated to preoperative muscle strength and function. As patients about to have TKR have osteoarthritis or other knee pathology that prevent heavy resistance training, BFRT is once again recommended as a suitable alternative. Trials are in progress but are yet to be completed for the effectiveness of BFRT eight weeks prior to TKR (Jorgensen, et al. [7]). There is difficulty creating a definitive strategy on how to use BFRT before or after knee surgery because of the lack of consistency and standardization in protocols. There is variation concerning the length of BFR treatment:
1. The difference in when treatment is commenced after surgery.
2. The frequency and length of BFRT used once started; and
3. The changeable occlusion pressures and cuff widths [1]. There do not seem to be safety concerns in using BFRT after knee surgery and no increased risk of Deep Vein Thrombosis (DVT) has been reported. However, it could cause an unintentional increase in muscular pain and could prolong post-surgical swelling [1]. This literature review intends to give the reader an insight into the effectiveness of BFRT for surgical patients with knee pathology. This study will discuss several papers and relate whether the evidence suggests that BFRT can be used more widely in to aid knee surgery rehabilitation.
Methods
Search Design
Studies were chosen following a comprehensive search of the PubMed database by two independent researchers. The database was filtered to highlight studies that included the following in their title or abstract: ‘blood flow restriction’, ‘KAATSU’ or ‘blood flow occlusion’. To further narrow the search criteria and suit the objectives, search filters for ‘rehabilitation’, ‘lower limb’, ‘upper limb’, ‘injury’ or ‘recovery’ were included with an ‘AND’ function. The database was searched from its inception until 1st October 2021. The studies selected for further discussion were ‘randomized controlled trials’ only. Literature reviews were also assessed as a means to search for more trials to be used for comparison.
Design Rationale
‘Randomized controlled trials’ were solely chosen for their ability to provide clear, objective outcomes, which, when pooled together, would provide data from which to draw significant conclusions. No time limit was placed on the trials used as, after consideration, each of the content was still deemed relevant to the objectives of the review. Specific focus on recovery and rehabilitation in the context of Orthopaedic patients was necessary for the review to have actionable outcomes. Blood flow restriction training was trialed in hypertrophy exercises and there was an increase in performance in numerous studies; however, comparing studies of this nature and those with a focus on rehabilitation was deemed not viable. Initially, one of the primary goals of the review was to observe for differences in the benefits of blood flow restriction training between the upper and lower limbs. Following a review of the available literature, there were an insufficient number of studies concerning the upper limb, in the context of rehab for surgical interventions, to allow for direct comparison.
Inclusion and Exclusion Criteria
After a review of the available literature, the following conditions were proposed for the study to be considered suitable:
1. Randomized controlled trial or technical note.
2. Primary focus on blood flow restriction training.
3. A patient group comprising individuals using BFRT as a form of rehabilitation or recovery following injury or surgery; and
4. Sole focus on lower limb and concentration on studies about surgical conditions, such as ACL reconstruction and TKR. From these criteria, nine studies were selected.
Limitations of the Methodology Used
Only the PubMed database was used to search for studies. Limiting to the above-mentioned search criteria also restricted the number of studies available, hence reducing the significance of the review’s findings. The authors recognized this but deemed that it was more important to keep the aims of the review concise and coherent. Two researchers compiled a list of trials independently.
Studies Reviewed
Safety
DePhillipo, et al. [1] technical note written in 2018 outlines the application technique for blood flow restriction (BFR), safety considerations and post-operative rehabilitation protocols regarding BFRT [1]. BFR causes venous occlusion and reduces the arterial blood supply to the muscle, which produces an anaerobic environment due to decreased oxygen supply. This can occur even with low resistance exercises, which is the reason why BFR should be effective. The anaerobic environment induces cell signalling and hormonal changes that cause protein synthesis, proliferation of myogenic satellite cells and activation and mobilisation of type II muscle fibres, thus promoting muscle hypertrophy. The goal is to use BFRT to achieve similar increases in muscle hypertrophy obtained by traditional strength training programmes, all whilst causing less pain during and after training, as well as reducing loading on the joints [1].
Indications to use BFRT on patients after knee surgery include 1. Patients who have a protected weight-bearing status; they can bear weight as tolerated. However, gait aids are mandatory at all times until further follow-up.
2. Muscular inhibition
3. Muscle atrophy prevention from lack of use in patients with significant post-operative pain
4. Restoring muscular strength to its pre-surgery or -injury level [1].
There are also several risks when it comes to BFR; the most apparent one is the use of the tourniquets. Thus, all patients should be checked for risk factors and contraindications prior to tourniquet use. Some of the factors that place patients at risk include but are not limited to obesity, diabetes, circulatory system issues, arterial calcification, sickle cell anaemia, renal compromise and severe hypertension. Possible contraindications include but are not limited to venous thromboembolism, medications with elevated clotting risk, peripheral vascular disease, sickle cell anaemia, lymphadenectomy and cancers [1]. Some of the potential complications of tourniquet use are skin injury, nerve injury, arterial injury, pain, temperature changes, prolonged post-operative swelling and ischaemia. The factors causing these complications are
1. Extended use of the tourniquet without a break.
2. The high pressure and narrow width of a cuff.
3. The high-pressure gradients under the tourniquet. The risk of these complications can be reduced by noting the minimum pressure required to produce limb occlusion for each patient and recommending the use of pressure in BFRT for that patient. Modern pneumatic tourniquets allow patients to personalize the pressure required for occlusion. With the use of third-generation pneumatic tourniquets, there is only a 0.04% to 0.08% chance of complications, making them much safer. It has also been proven that lower pressures are needed when using a wider cuff to produce circulatory occlusion according to the Crenshaw et al. study [1]. Moreover, Estebe et al. claimed that a wider cuff is preferred as it causes less pain than a narrow cuff when occlusion is necessary [1]. The possibility of DVT occurring is a concern often mentioned with tourniquet use. However, it has been shown that pneumatic tourniquet use does not seem to be an independent risk factor. The studies by Madarame, et al. [8] and Clark, et al. [9] which were conducted using BFRT, do not show concerning changes to thrombus formation markers such as fibrinogen, D-dimer, C-Reactive Protein (CRP) or tissue plasminogen activator [8,9]. Additionally, the action of deflating the tourniquet appears to stimulate antithrombolytic factors. Both resistance exercise and acute periods of tourniquet use result in stimulation to the fibrinolytic system [1].
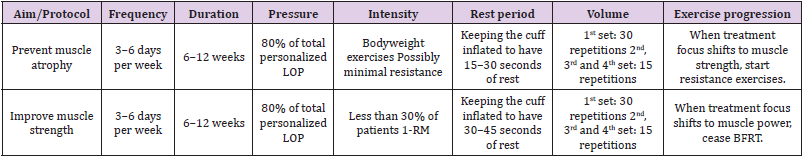
BFR has several protocols for use after surgery. This includes using a tourniquet cuff and a tourniquet system connected to a hose assembly to inflate the cuff. The cuff port connector should be on the lateral side of the limb when used to prevent hose entanglement and unnecessary added pressure on the superficial nerves. The system should be checked for defects that could impair function and should be tested to ensure that it is operational. Underneath the cuff, a protective sleeve should be placed on the skin to prevent skin or soft tissue damage. Additionally, the equipment should be examined to check that the system is clean before use. The cuff should be positioned around the most proximal portion of the upper thigh; if it is extremely close to the knee there is an increased risk of nerve compression and injury. Ideally, total Limb Occlusion Pressure (LOP) should be automatically calculated using a third-generation pneumatic tourniquet with a built-in Doppler ultrasound. The patient should lie in the supine position and remain as still as possible. It is recommended that 80% of total LOP is used during BFRT [1]. Post-operative protocols for BFRT to reduce muscle atrophy or improve muscle strength are shown in Table 1.
The ‘prevent muscle atrophy protocol’ should be followed in post-operative patients who are non-weight-bearing or have weight-bearing limits, while the ‘improve muscle strength protocol’ should be used in post-operative patients who can bear full weight. Whilst muscle strength refers to the patient’s ability to overcome resistance, muscle power is the ability to overcome resistance in the shortest amount of time [1]. For patients trying to prevent muscle atrophy, only bodyweight exercises with minimal or no resistance can be performed. The exercises involved could be terminal knee extensions, quadriceps sets or stationary bike use. Bodyweight closed kinetic chain exercises can be used in patients who are ambulating with full weight. A 2-second concentric contraction followed by a 2-second eccentric contraction should be the target for each repetition. If the individual is struggling to perform the number of required repetitions per set or to finish the total number of sets, then the rest period can be increased as necessary. The goal of this protocol is to perform a high number of repetitions using a light load with short rest periods to produce a metabolic response. The use of low load strength training aims to minimise tissue damage and allows for the same muscle groups to be trained for multiple days in a row. Once appropriate and the patient can weight bear, they can progress and commence on the ‘improve muscle strength protocol [1]. For patients trying to improve muscle strength and fully weight-bearing post-operatively, exercises with low resistance, i.e. a load of 30% or less than their 1-RM, should be performed. Ideally, muscle groups should be alternated if BFRT is carried out daily; for example, targeting quadriceps one day and then hamstrings the next. A few of the included exercises are leg presses, deadlifts and lunges. Longer rest times are observed compared to the ‘prevent muscle atrophy protocol’ as can be seen in Table 1. After patients have gained enough muscle strength, they can progress to develop muscle power, at which point they can stop using BFRT [1].
Total Knee Replacement
There is another multi-center, randomized, controlled, assessor-blinded study proposed but not yet completed for patients who have osteoarthritis who are awaiting TKR. The study aims to determine if pre-operative low-load BFRT can improve muscle strength, functional capacity and self-reported outcomes after TKR. Additionally, it will analyse whether pre-operative BFRT can prevent muscle atrophy three months after TKR surgery. Hopefully, this study will shed light on whether BFRT is a viable recovery option for patients after TKR [7].
Anterior Cruciate Ligament Reconstruction
BFRT, as part of a wider rehabilitation programme following ACL reconstruction, has been trialed on multiple occasions (Erik Iversen, et al. [3,5,10,11]). Poor rehabilitation following ACL injury has been linked to an increased risk of knee osteoarthritis, re-injury and loss of function compared to pre-injury levels. BFRT has been noted as beneficial in aiding recovery, especially as patients may find increased pain in heavy load-bearing exercises; thus, reduced load and increased resistance due to BFRT can support strength recovery. This, in turn, drastically reduces the incidence of postoperative patellofemoral pain syndrome [11], as patients are able to perform rehabilitative exercises without needing to perform load bearing, pain-inducing movements (Giles, et al. [11]). A study performed in 2016 [3] observed the effects of occlusion stimulus on quadricep atrophy after ACL reconstruction. From the second day post-surgery, a group of patients received an occlusion stimulus, i.e., BFRT, for five minutes, followed by removal of the occlusion stimulus for three minutes. This was repeated five times, twice daily. The study observed changes in the cross-sectional quadricep area on MRI, which showed a significant reduction in size in both the group performing BFRT and the control group (13.8% and 13.1%, respectively). This study suggests that intermittent BFRT does not reduce atrophy following ACL reconstruction. However, this study only observed the effects of BFRT 16 days after surgery. The study also acknowledged that its findings are in contrast to that of several other similar studies1 and remarked that its findings may be due to a lower training intensity than that of other studies, with the optimum load under blood flow restriction being approximately 10% of maximal strength (Takashi, et al. [12]).
As opposed to a reduction of atrophy, a study completed in 2018 [13] aimed to assess the role of BFRT in preserving quadricep muscle endurance. In this case, exercise sessions were performed over the eight days prior to surgery. Twenty subjects were assigned into groups that either performed BFR knee-extension or non-BFR knee extension. Measurements of maximal isometric contraction, time of submaximal isometric contraction and the surface area of the vastus medialis muscle were taken at four- and twelve-weeks post-surgery. Maximal isometric contraction strength was shown to be concurrently decreased in both groups at the four- and twelveweek stage, with no significant difference between either group. The length of time a patient was able to sustain a submaximal contraction was significantly shorter in the control group after four weeks, as opposed to the BFR group, which did not decreasesignificantly from the pre-operative values. At 12 weeks postsurgery, both groups’ average submaximal contraction time had returned to their baseline values. This study also looked at the effect of BFRT on post-operative post-exercise muscle blood flow, demonstrating a 50% increase in muscle blood flow in the BFR group and a 30% decrease in the non-BFR group. This suggests that preconditioning with BFRT improved microvascular function even after surgery, whilst those who preconditioned without BFRT had a marked deterioration in function post-operatively.
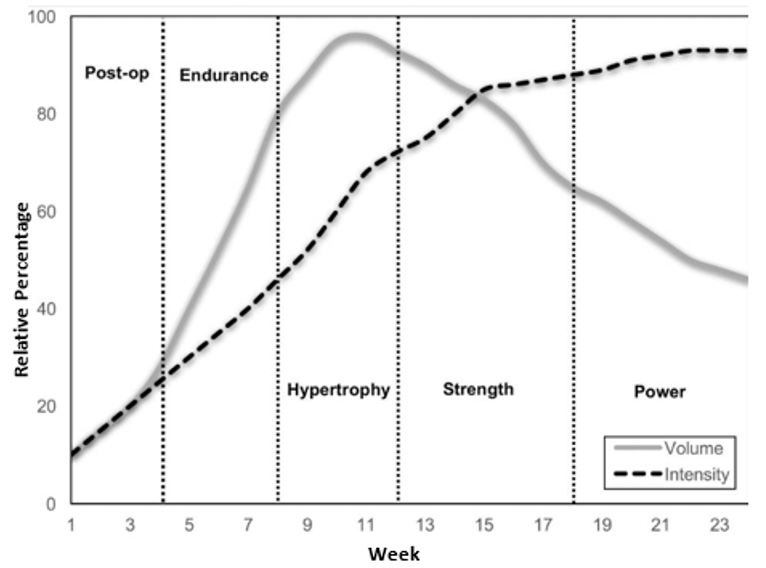
Restoring quadricep function after ACL reconstruction is important as if function remains poor the risk of re-injury and knee osteoarthritis is markedly increased2. This is demonstrated by findings that show a three times greater risk of subsequent knee injury in those with a limb symmetry index of less than 90%, i.e., one limb that is much stronger than the other (Grindem, et al. [14]). It often takes at least six months to retain knee extensor muscle strength, which in itself is often only a mid-rehabilitation marker as functional strength and movement quality are yet to be restored. Interventions that have the potential to reduce this period of time would be vastly appreciated by patients. The length of time an individual would be susceptible to re-injury would also be shorter. As seen in the graph above (Figure 1), the optimum approach to training after ACL surgery involves a period of hypertrophic training between weeks eight and twelve, with a submaximal endurance period from weeks four to eight. The initial four weeks comprise a period of immediate post-operative recovery, wherein heavy loads are not recommended due to ongoing tissue repair and joint instability. The study [13] advised that, in patients whose recovery has been slowed by ongoing pain on resisted knee extension, BFRT can be a useful tool to develop muscle strength, and could be used sparingly, especially during the hypertrophic portion of a periodized strength training programme.
Discussion
More evidence is required to conclude whether BFRT is a suitable option to help those undergoing TKR7 but as there appear to be positive results for those with osteoarthritis [2,6] and patients having ACL surgery [3,13], we estimate that further studies will be successful. Restoring quadricep function after ACL reconstruction is important as if function remains poor the risk of re-injury and knee osteoarthritis is markedly increased [2]. The rehabilitation programmed that are widely used have differing structures; the number that have trailed BFRT is small but early results have been promising. There is currently a lack of discernible evidence regarding whether BFRT is more beneficial pre- or post-operatively. The two primary studies analysed [3,13] show some positive results when BFRT was undertaken prior to surgery; however, no difference in maximal isometric strength in either group was noted and there was no reduction in atrophy in either the BFRT or non-BFRT groups taking part in rehabilitation that started post-surgery. The overall efficacy of BFRT with a specific emphasis on rehabilitation after ACL reconstruction still requires further examination. There are not yet a sufficient number of studies to analyses the long-term effects of BFRT on reduction of re-injury and subsequent muscle atrophy compared to other potential risks posed by BFRT, such as increased risk of future osteoarthritis. Its use as an adjunct to other, more conventional forms of post-reconstruction therapy has been suggested [5] but thus far the evidence supporting this is largely anecdotal. Although most of the studies have attempted blinding, it should be mentioned that participant blinding is not feasible due to it being obvious to the patient when they receive BFRT [2,3,6,13]. The efficacy of using BFR post-knee surgery and for osteoarthritis is uncertain as there is a scarcity of studies and the application of BFR often differs, for example, in regard to limb occlusion pressures, the timing of the initiation of BFR, the frequency of exercise and the angle at which certain exercises are performed with BFR. In the studies mentioned above, the training methods and use of BFR varied, making it difficult to directly compare the effectiveness of BFR. Our recommendation would be to apply BFRT using the postoperative protocols (knee surgery) listed earlier in this paper.
Furthermore, it is essential to consider the safety of the patient, taking into account preferential use of a wide, modern pneumatic tourniquet with contoured tourniquet cuffs. We also propose that all patients should be screened for risks and contraindications to tourniquet/BFRT use [1]. Additionally, clinicians may not understand the protocols to follow for BFRT to have the most positive effect on post-operative complications. If BFRT is to be used more widely, there should be education of clinicians and those helping to facilitate it [1]. On top of this, there should be education that BFRT can aid in the prevention of blood clots by activating fibrinolytic proteins and antithrombolytic factors, as there may be misconceptions that it increases the risk of DVT [1]. We believe that the advantages of being able to reduce muscle atrophy and improve muscle strength following knee surgery using only low-resistance exercises outweigh the risks of using BFR, especially as many of the risks associated with BFR can be reduced with the recommended tourniquet equipment and proper application of the devices [1]. However, disadvantages, such as the potential to cause prolonged post-operative swelling or the expense of buying equipment and paying any trained personnel required to facilitate BFR, should be considered before starting patients on these training programmes4.
Conclusion
BFRT is a safe intervention when used correctly and has the potential to aid many patients in preventing muscle atrophy as well as improving muscle strength for patients who have knee injury, or knee-related weakness and atrophy, commonly after surgery. The disadvantages are that it may cause prolonged swelling post-operatively, and it is expensive to have a third-generation tourniquet. Trained personnel may often be required to aid the patient in using BFRT equipment. Using standardized training programmed with similar methods for acquiring occlusion would allow for direct comparison of studies against each other and help to identify whether BFRT is truly an intervention that will produce positive results. Further research with larger cohorts of patients is required to fully assess whether BFRT is a valid alternative to improve strength and function and reduce atrophy in patients with a variety of lower limb conditions. If further evidence supports, the findings found in this paper then BFRT should be used more widely in practice for lower limb conditions requiring surgery.
For more Articles on: https://biomedres01.blogspot.com/

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.