Epidural Adhesion: The Most Obvious Target for Low Back Pain Treatment
Opinion
Low back pain is one of the most common causes of suffering for many people. Although many methods have been proposed for the exact cause and treatment of low back pain, many patients are living with low back pain that does not improve even with such methods. Traditionally, most patients with low back pain have confirmed the findings of a herniated disc or spinal stenosis through MRI or CT, and have received surgical treatment for it. However recent studies revealed that such findings from image studies cannot explain the patients pain and are not helpful to predict the prognosis [1]. One of the most frequently observed lesions during epiduroscopy (for patients with chronic low back pain) is epidural adhesion. It is the fibrotic lesion in epidural space which leads to persistent back pain by pulling, stretching, or compression nerve roots or dura mater [2]. Epidural adhesion, also called as epidural fibrosis, is mostly comes from chronic inflammation or post-surgery state (e.g., epidural scar tissue). An epiduroscopic revealed that more than 90% of patients with persistent back pain after lumbar surgery had epidural fibrosis [3].
One of the most recently used methods for treatment for back pain is epidural injection, which the needle is in the epidural space and can deliver the necessary drugs for relieving pain directly near the nerves. Several studies showed the effect of epidural injection for spinal pain. The focus in the epidural injection is the role of drug, which are the local anesthetics (for stabilizing nerves), steroids (for anti-inflammation) in usual. But, how about the injection itself? Epidural injection can work either by lavage of the epidural space or by a mechanical effect. Injection volume, regardless of the regimen, is a factor for greater relief of radicular leg pain and/or low back pain after epidural injection [4]. A recent meta-analysis revealed that epidural saline injection, without steroid, is effective in reducing low back and/or leg pain and it is not a true placebo of epidural steroid injection [5]. This concept can be also applied for transforaminal epidural approach. Mild epidural adhesion can be removed by epidural injection with sufficient volume of injectate, even the local anesthetics or steroids are not included. For this, the appropriate needle tip position is important.
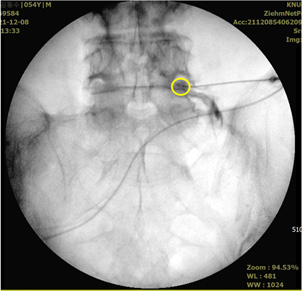
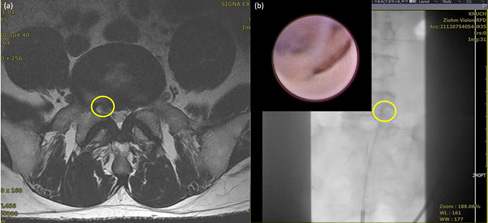
The needle should be advanced medially to the lateral margin of the pedicle at least for lavage effect. The injectate, either saline or drug, can spread into epidural space more efficiently at this position [6] (Figure 1). When the patient’s symptoms do not improve significantly with epidural injection, we are already treating epidural adhesion using a treatment called neuroplasty, and the epiduroscope allowed us to see the pathology directly (Figure 2). However, with the current technology, it is difficult to treat if the adhesion is severe. Hyaludronidase is currently used, but it does not show a significant effect on severe adhesions, and there are no data on the difference from general hydrodisection. In the future, a drug that can selectively remove only adhesions while protecting the surrounding tissue or a catheter with a shape and material that can physically remove adhesions should be developed.
Figure 1: The fluoroscopic image of transforaminal epidural injection at right L5-S1. Yellow circle indicates the needle tip which is located medially to the lateral margin of the pedicle. And the contrast media disperses both into epidural space and following the nerve root.
Figure 2: MRI image and epiduroscopic view of the patient who complain chronic low back pain which radiates to right leg (calf).
(a) Axial view of lumbar MRI at L5-S1
(b) The fluoroscopic image of epiduroscopy and epiduroscopic view which shows epidural adhesion (left upper). Yellow circle: the pathologic site.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.