Efficacy Analysis of Trans-Vaginal Cystocele Repair with Transobturator Four-Arm Mesh: A Mid-Term Follow-Up
Introduction
Pelvic organ prolapse (POP) refers to a female pelvic organ (vagina, uterus, bladder and/or rectum) that enters or protrudes beyond the vagina. POP is a common disease involving women’s pelvic floor, which has a negative impact on women’s quality of life, sex life and body image [1]. The prevalence of POP varies depending on the diagnostic criteria, from 3% to 50%, based on symptoms and vaginal examination findings [2]. Cystocele (also known as anterior vaginal wall prolapse) is the most common type of POP caused by the relaxation of the anterior vaginal wall. According to statistics, the incidence of posterior vaginal wall prolapse (rectocele) is twice that of uterine prolapse. Hysterectomy (or vaginal vault prolapse during hysterectomy) three times [3]. Various surgical methods are available to treat anterior vaginal wall prolapse (Cystocele), possibly reflecting lack of consensus regarding the optimum approach [4]. The current treatment methods are divided into traditional non-mesh anterior pelvic repair surgery and mesh repair surgery [5]. In 2002, the FDA approved the first surgical mesh product for POP disease. The introduction of surgical mesh makes transvaginal POP repair easier to learn and operate, and mesh shows better anatomical repair advantages in the treatment of cystocele [6]. In the past two decades, transvaginal polypropylene mesh (transvaginal mesh repair, TVM) has made great progress in the treatment of cystocele [7]. However, compared with traditional meshless repair surgery, mesh surgery is still controversial in terms of symptom relief rate, surgical complications, and recurrence of prolapse. The purpose of this study is to evaluate the effectiveness and safety of transvaginal transobturator polypropylene pelvic floor mesh in the treatment of cystocele.
Clinical Characteristics Surgical Steps and Follow- Up
A retrospective analysis of the clinical data of patients with cystocele in the Department of Urology, Shanghai Changhai Hospital from September 2016 to April 2018. The surgeries were performed by a single surgeon with extensive experience in urology and pelvic organ prolapsed (POP) repair. According to the classification of pelvic Organ prolapse quantification (POP-Q), patients who are diagnosed as ≥ II degree [8] and have no history of POP surgery. The surgical method is transvaginal transobturator bladder prolapse repair with four-arm polypropylene mesh. If patients combined with III-degree or IV-degree posterior vaginal wall prolapse, the vaginal posterior wall repair (autologous tissue repair) will be performed simultaneously with transvaginal transobturator bladder prolapse repair. Obtain the patient’s informed consent. Collect the patient’s clinical data, operation time, blood loss, hospital stay and complications and other information. Using TiLOOP Total 4 four-arm pelvic floor prolapse repair mesh, prepare two sets of puncture needles.
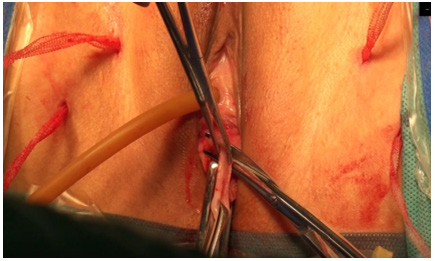
The patient takes the lithotomy position, an indwelling F18 catheter to empty the bladder, injects normal saline under the vaginal wall, and takes 2cm from the lower edge of the urethra vagina to the fornix of the anterior vagina tomake a longitudinal incision as shown in (Figure 1) to fully separate the vagina and bladder The fascia on both sides of the serosal layer, the anterior branch puncture point is at the height of the urethral orifice and the base of thigh. The posterior branch is 2cm outside and 2cm below the anterior branch (Figure 2). The upper edge of the mesh is fixed at the bladder neck and the lower edge is fixed at the cervix. The mesh is in an expanded state. Cut off the excess anterior vaginal wall (Figure 3). The extra sling is cutted off. Put iodophor gauze into the vagina and take it out after 48 hours (Figure 4). Follow-ups were conducted at 12 and 24 months after surgery. A POP-Q of 0 or I was defined as an objective cure. Intraoperative complications, early complications and late complications were counted. Complications less than 30 days after surgery were defined as early complications, and complications greater than 30 days after surgery were defined as late complications. The statistical method uses SPSS 13.0 software, the measurement data is represented by the mean, median, standard deviation, minimum and maximum value, and the count data is represented by frequency and percentage.
Outcome
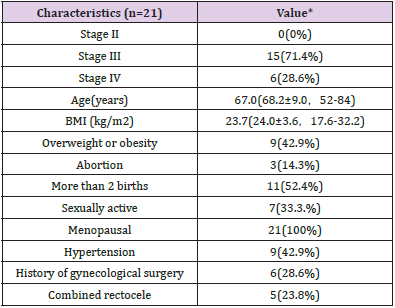
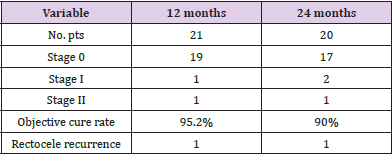
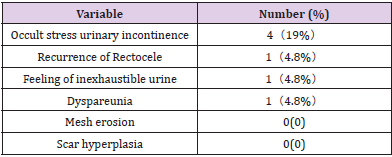
A total of 21 patients were included in this study. The clinical characteristics and demographic features are shown in Table 1. Among them, 15 cases (71.4%%) were stage III prolapse, 6 cases (28.6%) were stage IV prolapse; the average age was 68.2 (±9.0) years, 42.9% of them were overweight or obesity, and 52.4% had multiple births ( ≥2 times), 28.6% had a history of gynecological surgery. Among them, 5 cases were combined with posterior vaginal wall prolapse (rectocele), and all were stage III or IV, and underwent repair of posterior vaginal wall at the same time. The operation time was 66.0±13.7 (50-105) min, the blood loss was 26.2±13.2 (10-50) ml, the total hospital stay was 8.5±1.5 (6-12) days, and 20 cases (95.2%) were cured objectively after 12 months. 1 case had recurrence of posterior vaginal wall prolapse. One case was lost to follow-up 24 months after the operation, and 19 cases (95%) were cured objectively (showed Table 2). The complication statistics are shown in Table 3. All 21 patients had no early complications. In terms of late complications, 4 cases (19.0%) had occult stress urinary incontinence 2 months after the operation, of which 2 cases underwent TVT-O (Tension-free vaginal tape obturator)surgery; 1 case (4.8%) had recurrence of posterior vaginal wall prolapse (stage III) at 10 month after surgery who was cystocele combined with posterior vaginal, and underwent repair of posterior vaginal wall once again; 1 case (4.8%) had a feeling of inexhaustible urine, but the residual urine of ultrasound was negative, and the symptom improved after oral tamsulosin treatment; 1 case (4.8%) complained of dyspareunia and pain relief in 10 months after surgery. In this study, there were no complications of mesh erosion and scar hyperplasia.
Table 1: Demographic features and clinical characteristics.
Note: Value* defined as median (mean ± SD, range), or number (percentage)
Table 2: Follow-up at 12 and 24 months after surgery.
Note: Data are expressed as absolute number or percentage.
Table 3: Complications rate associated with operations at 12-months follow-up.
Note: Values are presented as number (%).
Discussion
POP seriously disturbs women’s quality of life and increases the medical burden. In the United States, about 22,500 surgical operations are performed each year due to pelvic organ prolapse, and cystocele and posterior vaginal wall prolapse account for 80% [9]. In the UK, POP accounts for about 20% of gynecological operations and is the main reason for hysterectomy in postmenopausal women [10]. An epidemiological survey of urban population in China shows that 9.67% of women suffer from POP of varying degrees, and the prevalence increases with age. The prevalence of women over 70 years old is about 26.11% [11]. The risk factors for POP vary among patients. A recent systematic review of studies found that parity, vaginal delivery, age, and body mass index were pivotal risk factors for primary POP in developed Western countries [12]. The 21 cases in this study were all postmenopausal women, and the proportion of elderly women was high. Among them, 42.9% were overweight or obesity and 52.4% had more than 2 births. POP surgery has two methods, transvaginal or transabdominal, which can be divided into autologous tissue (non-mesh) and polypropylene mesh repair. At present, 80-90% of operations choose the transvaginal surgery [13]. Anterior colporrhaphy, known as traditional repair of anterior vaginal wall prolapse including cystocele, alone has a high failure rate and can lead to vaginal shortening and/or constriction and is useful only for the midline defects [14, 15]. The transvaginal route of mesh procedure for anterior prolapse, first described by Julian, has reported good success rates in various non-randomized trials, ranging from 75% to 100% [16-18].
Palma introduced the transobturator four-arm mesh for the treatment of cystocele for the first time in 2004, and more and more relevant studies and cases have been reported since then [19]. In this study, the cure rate was 95.2% and 90% at 12 and 24 months after surgery, which was similar to the mid-term follow-up study of Yonguc and other double sling surgery [20]. In this study, there were no intraoperative complications such as bladder perforation or urethral injury; similarly, there was no need for blood transfusion caused by massive bleeding during the operation, and the average blood loss was only 26.2 (±13.2) ml, which is consistent with the results of the Kdous and Zhioua study [21]. There was no early complications such as fever, hematuria, urinary tract infection, and deep venous thrombosis. 4 cases (19.0%) developed occult stress urinary incontinence (SUI) during follow-up, of which 2 cases underwent Transobturator Tension-free Vaginal tape (TVT-O) in our hospital, and 2 cases did not receive surgery because of moderate symptoms. Occult SUI refers to the new SUI that appears after the POP is cured or relieved. About 50% of SUI women with no symptoms may develop SUI after the prolapse is repaired. Women with symptoms of urinary incontinence or a history of SUI have a higher risk of developing SUI. [22]. In this study, there were no cases of recurrence of cystocele. One case who was cystocele with posterior vaginal wall prolapse was found recurrence of posterior vaginal wall prolapse at 10 months and received posterior vaginal wall prolapse repair operation again.
Eboue et al. reported that the recurrence rate of cystocele was 2.4% after 123 women underwent transobturator four-arm mesh repair for 1 year [23]. We believe that the recurrence of cystocele is related to the displacement of the mesh, surgeon experience and the material of the mesh. The mesh and histocompatibility are critical. This process takes several weeks. We recommend that patients stay in bed within 2 weeks after surgery and avoid strenuous activities within 4 weeks, which may also be one of the reasons for no recurrence. One case (4.8%) had dyspareunia. We believe that dyspareunia has nothing to do with the mesh itself, but may be related to some other aspects of the operation. In order to reduce the risk of dyspareunia after surgery, the surgeon must ensure that the mesh placement is tension-free and the mesh arm is not stretched too tightly, so as to In order to relieve the pain of postoperative painful sexual intercourse [24]. Mesh erosion is one of the most common and serious complications after POP repair, with an incidence of 4% to 30% [25].
The size and location of the vaginal incision, the depth of the incision, sexual intercourse, and younger women are considered to be risk factors for mesh erosion. In addition, insufficient surgeon experience is also a factor in the high incidence of mesh erosion [26, 27]. In this study, the occurrence of no mesh erosion complications may be related to the surgeon professional training in urology and the guidance and supervision of experienced superior doctors. The main limitations of this study are single center, small number of cases, short follow-up time, and no quantitative subjective evaluation of surgical satisfaction. In summary, the transobturator four-arm polypropylene mesh is safe and effective in the treatment of cystocele, and the complications are controllable. The strength of the present study is relatively comprehensive long follow up and uniformity of this procedure as it is a single-center, single-surgeon study using the same technique. However, more randomized controlled, multi-center, long-term follow-up, and large-sample studies are still needed to further evaluate the safety and effectiveness of the transobturator four-arm pelvic floor mesh.
For more Articles on: https://biomedres01.blogspot.com/






No comments:
Post a Comment
Note: Only a member of this blog may post a comment.