Acute Acalculous Cholecystitis Due to Covid-19: A Case Report
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the seventh human coronavirus, was discovered in Wuhan, Hubei province, China. Since its first documentation in January 2020, the virus has emerged worldwide, with the consequent declaration of a pandemic disease (COVID-19) [1]. The common presentation includes fever, myalgia as well as respiratory symptoms such as dry cough, dyspnea and anosmia [2]. Besides pulmonary involvement, SARS-CoV-2 may affect other organs such as the liver, inducing occasionally acute hepatitis and late cholestasis [3]. Rarely, it has been reported to cause acalculous cholecystitis. Several mechanisms are considered to be involved in gallbladder injury in COVID-19 patients. We report here a rare case of acute acalculous cholecystitis in a non-ICU setting COVID-19 patient.
Case Presentation
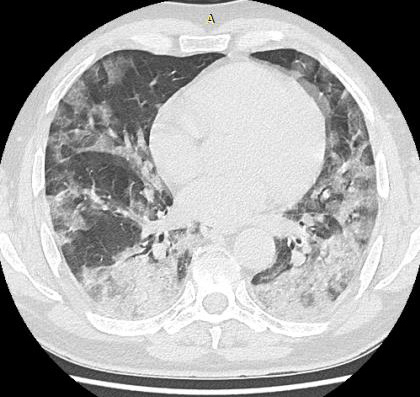
Figure 1: Chest CT scan showing typical findings of COVID-19 pneumonia affecting 35% of lung parenchyma.
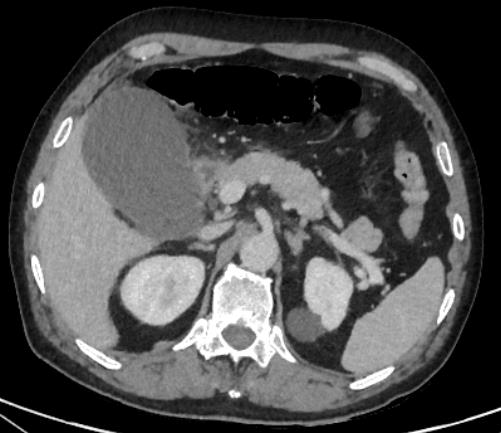
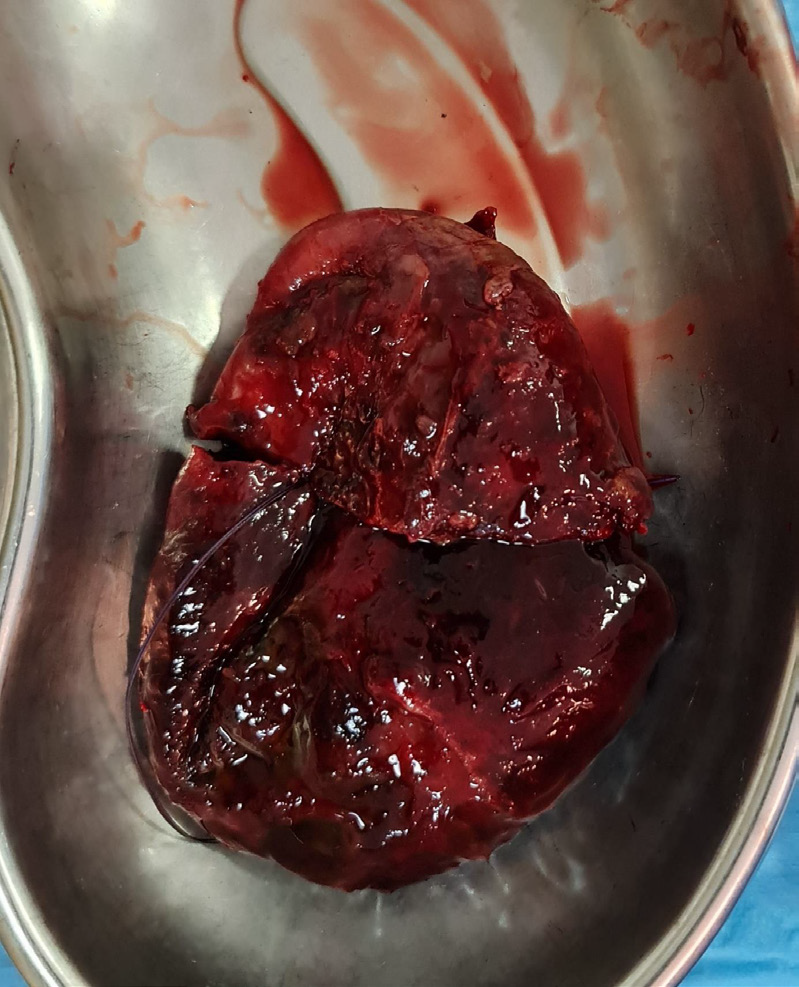
A 52-year-old healthy man, with no past medical history, presented to the emergency department with the chief complaint of fever, myalgia and dry cough evolving for three days. Clinically, he was awake and conscious, with a temperature at 38,3°, blood pressure at 12/07cm Hg, heart rate at 90/min, respiratory rate of 24 breaths/min and O2 saturation at 91 %. Nasopharyngeal RT-PCR was positive for SARS-CoV-2 infection. Laboratory studies showed a normal white blood cell count of 3.64 × 109 /L (normal range, 3.50– 9.50 × 109 /L), elevated blood levels for C-reactive protein (46.7 mg/L: normal range, 0–10 mg/L) and normal kidney and liver tests. The patient was transferred to COVID-19 unit. Chest computed tomography showed typical findings of COVID-19 pneumonia, affecting 35% of lung parenchyma (Figure 1). He was treated by low flow oxygen therapy (3 to 6L) maintaining oxygen saturation more than 93%, methylprednisolone, enoxaparine and vitamins. During his hospital stay, his clinical condition progressively improved. But after seven days, he developed progressive onset of rightsided hypochondrial pain. Physical examination found abdominal distension with right hypochondrium tenderness. Laboratory tests showed that inflammation markers had markedly increased with white blood cell count and C-Reactive protein at 16.97 × 109 /L and 155 mg/L respectively. Ultrasound and computed tomography of the abdomen revealed a severe gall bladder distention with thickened wall and minimal surrounding pericholecystic fluid. No gallstones were identified, and the extrahepatic bile ducts were normal (Figure 2). These findings were consistent with acute acalculous cholecystitis (figure). IV antibiotics were initiated but there was no clinical improvement. After four days, he became hypotensive and tachycardic at 120 beats/min. Emergency surgery was decided. Laparotomy was preferred over laparoscopy to limit aerosolisation. Intraoperative exploration revealed a markedly distended gallbladder with thickened and gangrenous wall. Cholecystectomy was hardly completed because of the severe inflammation of cystic pedicle (Figure 3). Histological analysis showed thickened gallbladder wall with edema and hemorrhage on gross examination. There were no gallstones. Microscopic examination showed fibroinflammatory infiltration with endoluminal obliteration of vessels, ischemic necrosis, venous congestion, edema and hemorrhagic infarction. The post-operative course was uneventful. Abdominal pain was significantly resolved, and vital signs were within normal range with oxygen saturation at 98% on room air. On the 5th post-operative day nasopharyngeal RT-PCR was performed and became negative to SARS-CoV-2. The patient was discharged from the hospital on post-operative day 6 with oral antibiotic, enoxaparine and vitamin supplements. A follow-up examination was done two weeks after surgery and was without abnormalities.
Discussion
AAC is an uncommon condition characterized by inflammation of the gallbladder in the absence of gallstones. It is an insidious clinical condition which typically occurs in critically ill patients, especially related to trauma, surgery, mechanical ventilation, severe burns, total parenteral nutrition, and/or prolonged fasting [4]. Its pathogenesis is thought to be due to gallbladder stasis secondary to lack of gallbladder stimulation, leading to the build-up of intraluminal pressure, which results in inflammation and necrosis of the gallbladder wall. On the other hand, this static condition promotes bacterial colonization of the gallbladder particularly by enteric pathogens such as Escherichia coli, Klebsiella, Bacteroides, Proteus, Pseudomonas, and Enterococcus faecalis [5]. Since the presentation may be insidious and patients often lack right upper quadrant tenderness, clinical diagnosis is challenging [6]. Since late December 2019, the emergence of coronavirus disease 2019 (COVID-19), caused by the novel SARS-CoV-2, has led within a few months to a major global health and economic crisis [7]. It primarily affects the respiratory system, inducing dry cough, dyspnea and anosmia, associated with systemic symptoms like fever and myalgia [2]. Non-specific gastrointestinal symptoms are also seen such as diarrhea and abdominal pain [8]. Although COVID-19 infection mainly affects the lung, other organs such as the liver may be affected, with frequent onset of late cholestasis. However, gallbladder involvement with acalculous cholecystitis is extremely rare. To our knowledge, only 10 cases were reported in the medical literature, since the pandemic declaration. It remains unclear whether AAC is a direct manifestation of the SARS-CoV2 or a consequence of prolonged illness [9]. While most of these cases were described in critically ill patients with long ICU stays, we report the third case of AAC on a healthy patient with mild COVID-19 pneumonia, who did not develop acute respiratory distress syndrome. Alhassan, et al. [10] also reported a recent case of a middle-aged healthy women who developed AAC during her hospital stay for a mild COVID-19 pneumonia.
It was managed by broad spectrum antibiotics with good outcome. It is well known that SARS-CoV2 have a tropism not only to the lungs but also to the liver and the gallbladder. The intracellular entry of the virus occurs through interaction with the angiotensin-converting enzyme 2 receptor (ACE2), which expresses in relatively high amounts in lungs, vascular endothelium and gallbladder [11,12]. Therefore, patients with SARS-CoV-2 infection may be at increased risk from direct viral effects on the vascular endothelium and infection to the biliary tissue [13]. Recently, a case report has described an AAC in an 84-year-old COVID-19 patient, who underwent laparoscopic cholecystectomy. On histological analysis, quantitative reverse transcriptase PCR revealed the presence of SARS-CoV-2 in all 3 sampled regions of the gallbladder wall. This viral RNA detection in the gallbladder indicates direct vesicular involvement [14]. Otherwise, inflammatory cytokine storm generated by the excessive immune response could also be one of the key factors in hepatobiliary injury [12]. Interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), which plasma levels are high in severe inflammatory response, may activate the coagulation cascade, explaining the presence of thrombosed vessels in the gallbladder and the occurrence of ischemic cholecystitis [11,15]. SARS-CoV-2 infection induces inflammation of the vascular endothelium, thereby causing vascular dysfunction, especially in capillaries. Subsequently, microvascular dysfunction leads to a hypercoagulable state, tissue edema, and organ ischemia [12,16,17]. All these evidence support that SARS-CoV-2 may directly or indirectly cause acute cholecystitis.
Conclusion
By reviewing the recent literature, we noticed that the potential mechanisms of COVID-19-associated acalculous cholecystitis in non-ICU setting patients may include the direct effects of viral infection, inflammatory storm and endotheliitis. COVID-19 is proving to have multiorgan involvement during its disease course. Through our case, we aim to highlight the importance of early detection and prompt management of biliary complications such as acute acalculous cholecystitis. As the pandemic continues to spread, further data are necessary to accurately assess the physiopathogenesis of hepatobiliary injury.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.