Tubal Stump Pregnancy in ART Patients Two cases of ectopic stump pregnancy after IVF-ET
Abstract
Ectopic pregnancy (EP) is a complication of pregnancy in which the
embryo attaches outside the uterus. The rate of ectopic pregnancy is
about 1 and 2% that of live births, though it may be as high as 4% among
those using assisted reproductive technology (ART). We present two
cases of interstitial stump pregnancies in patients who previously
underwent salpingectomy for ectopic pregnancies, and a review of the
literature. One patient has been treated with methotrexate (MTX) before
the removal of the tubal stump, while the second has gone directly to
laparoscopic (LPS) surgery. Transvaginal ultrasound examination is
essential for early and accurate management of this condition. It should
be quickly performed to rule out a stump interstitial pregnancy in
women who conceive by ART after bilateral salpingectomy. A correct
attitude towards this condition is not yet internationally standardized
and both medical and surgical options should be promptly considered.
Keywords: Ectopic pregnancy (EP); Assisted reproductive technologies (ART); Tubal stump; Methotrexate (MTX); In vitro fertilization (IVF)
Abbreviations: EP: Ectopic Pregnancy; ART: Assisted Reproductive Technologies; MTX: Tubal Stump Methotrexate; IVF: In Vitro Fertilization
Introduction
Ectopic pregnancies (EP) represent the most serious complication of
the first trimester of pregnancy. In the vast majority of the cases the
embryo prematurely implants itself in the fallopian tube before arriving
in the uterine cavity. Only in approximately 2% of the cases EP occur
in different regions such as the cervix, the ovary or the abdominal
cavity [1-5]. An atypical and insidious severe event is that the embryo
migrates from the uterine cavity
to the contralateral tube. We report two cases in which the EP occurred
in a fallopian stump after in vitro fertilization (IVF) in women
subjected to monolateral salpingectomy for a history of ectopic
pregnancy. We present also a review of literature about interstitial
pregnancies in tubal stump (Table 1) and a review about EP in unusual
sites in women with previous salpingectomy (Table 2) [6-10].
Case report
Case 1
A 36 years old patient referred to our center to ascertain
implantation after IVF-ET at the 58th gestational day. The patient
had a history of right salpingectomy for GEU. HCG was 2293 IU/L.
Obstetrical examination showed a small uterus with no pain.
Ultrasound revealed no intrauterine pregnancy, but a gestational
sac of 14 mm adjacent to the right uterine cornu with no signs of
embryo viability. Power and color Doppler revealed the presence
of the vascular ring with a strong peri-trophoblastic vascular
activity (Figures 1 & 3). After careful counseling it was decided
to attempt medical management using the single dose regimen
with i.m. MTX (50mg/m2). Four days after treatment the patient
complained strong abdominal pains, low blood pressure and severe
anemia. Laparoscopy was carried out and the right tubal stump
was removed. Histological examination confirmed the diagnosis
of ectopic pregnancy of the right tubal stump. The patient was
discharged on day 2 postoperatively and no short- or long-term
complications were reported [11-17].
Figure 1: The gestational sac of 13 x 14 mm with no signs
of embryonic viability in the right interstizial tubal stump
at 58 days of pregnancy (Case 1).
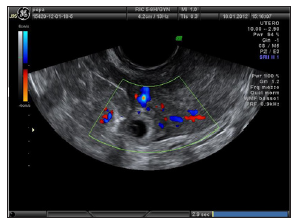
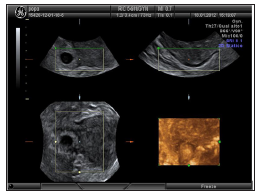
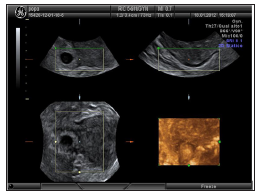
Figure 2: 3D reconstruction of interstitial tubal stump
pregnancy (Case 1).
Case 2
A 25 years old patient referred to our emergency Department
for pain in the right iliac fossa. She was at 7 weeks of gestation after
embryo transfer achieved by ICSI. The patient had a history of right
salpingectomy for GEU. Pelvic examination revealed pain in the right
adnexal area and US showed a gestational sac of 11 x 10 mm with
no signs of embryonic viability in the right interstitial tubal stump
(Figures 4 & 5) and hemoperitoneum. HCG was 8839 IU/L. The
patient was subjected to an emergency laparoscopy and the right
tubal stump was removed. Histological examination confirmed the
diagnosis of ectopic pregnancy in the right tubal stump. The patient
was discharged on day 2 postoperatively and no short- or long-term
complications were reported.
Discussion
Though the etiology of EP is multifactorial, as many as 50% of
women with an EP have no identifiable risks. Widely accepted risks
for EP are not necessarily independent of one another and can vary
depending on the population being reported. Risk factors include
prior EP, prior tubal and generally pelvic surgery, IUD and a history
of pelvic inflammatory disease (PID) [18]. In patients undergoing
ART, the chances of an embryo spontaneously implanting at
the interstitial tubal segment are higher when compared to a
spontaneous pregnancy [19]. Tubal stump pregnancies can occur
when the embryo or the oocyte migrate through the uterine cavity
or when the oocyte passes through a tubal fistula [3,9]. A review
of the literature conducted by Chin et al. [20] reported 22 cases of
cornual pregnancies after IVF-ET.
In women with a history of salpingectomy, some cases of
unusual implantation sites have been reported. Fisch et al. [12]
in 1996 reported a case of an abdominal pregnancy following in
vitro fertilization in a women subjected to bilateral salpingectomy.
Dmowsky et al. [14] reported a retroperitoneal ectopic pregnancy
located in the head of pancreas in a similar patient. Ferland et
al. [11] reported a retroperitoneal pregnancy in a patient with
previous right salpingectomy secondary to an ectopic gestation.
Agarwal et al. [21] studied 26 ectopic pregnancies detected after
embryo-transfer during a 7-year period and seven were located
in the cornual or tubal stump after prior salpingectomy. Four
out of seven women were treated with MTX, but in only one case
conservative treatment was successful. The other three cases were
tubal implantations, with one rupture during treatment. Chang et
al. [22] presented a case of bilateral simultaneous tubal sextuplets
pregnancy after in-vitro fertilization–embryo transfer following
salpingectomy. Chen et al. [13] described three cases of cornual
pregnancies occurring after IVF-ET.
Two of these patients had prior bilateral salpingectomy,
whereas another had prior tuboplasty for tubal disease. Nabeshima
et al. [23] presented the case of a 38-year-old woman, with a
history of left salpingectomy for an ectopic pregnancy, admitted
for treatment of another presumed ectopic pregnancy. Surgery
was performed for a suspected left cornual pregnancy and with
laparoscopy the gestational sac was removed; the uterus was
preserved. Unilateral and even bilateral salpingectomy cannot
prevent subsequent heterotopic pregnancy. Even more catastrophic
conditions may occur because the ectopic gestation is always
located within the interstitial tubal portion, rather than in the
ampullary portion of the fallopian tube [24]. The uterine cornu has
an abundant blood supply from branches of the ovarian and uterine
arteries and a ruptured cornu can have tragic consequences from
sudden and excessive blood loss. For this reason, these pregnancies
are generally associated with very high serum HCG levels and the
mortality rates for interstitial pregnancy are estimated to be 7-15
times higher than another EP [25].
At the beginning, the traditional treatment for interstitial
pregnancy was cornual resection by laparotomy or hysterectomy
[26]. In the last decades operative laparoscopy has generally been
considered the “gold standard” for the treatment of tubal ectopic
pregnancies [27], but medical treatment is viewed with increasing
interest. The medical treatment is of particular relevance in the case
of infertile patients for whom any avoidance of additional surgical
intervention translates into a reduced risk of repeating ectopic
pregnancy, in addition to maximal preservation of their future
fertility potential. The estimated success rate for medical treatment
with methotrexate of interstitial pregnancy is lower than that for
treatment of ectopic pregnancies located in the tubal ampulla or
isthmus [28]. Although medical therapy can be successful at serum
HCG concentrations considerably higher than 3000 IU/l, quality-oflife
data suggest that methotrexate is only an attractive option for
women with an hCG below 3000 IU/l [29-31].
In 2016, the Royal College of Obstetricians and Gynaecologists
(RCOG) released a new guideline providing evidence-based
guidance on the diagnosis and management of ectopic pregnancies
[32]. Concerning interstitial or cornual pregnancies, it pointed
out that even if a pharmacological approach using methotrexate
has been shown to be effective, there is insufficient evidence to
recommend local or systemic approach. Moreover, RCOG guideline
has confirmed the main role of surgery in the management of
cornual pregnancy with conservative, laparoscopic or open surgical
methods, and it reported medical therapy with methotrexate and
potassium chloride injection as an option prior to later laparoscopic
horn excision. Nevertheless, an international consensus on the
management of cornual or stump pregnancy is still far, as all the
evidence reported in the guideline come from non-analytical
studies, such as case reports or are based on expert opinion.
Reviewing the literature, we found only one case of tubal stump
pregnancy treated successfully with a single i.m. dose of MTX (100
mg) with a serum HCG concentration of 12.470 IU/ml 4]. The
presence of cardiac activity in an ectopic pregnancy is associated
with a reduced chance of success following medical therapy and
should be considered a contraindication to medical treatment
[32,33]. Therefore, a similar behavior should be considered for EP
of the tubal stump. In conclusion, early transvaginal ultrasound
should be considered in women with a history of salpingectomy in
order to allow early diagnosis of EP of the tubal stump. Physicians
should remember to consider this severe condition when surgically
treating conditions such as PID and EP and remove the fallopian
tube entirely [34-43].
Kinetics Study The Catalyze Mode Of The Formamide
Degradation Reaction By Aux Cluster (X=0, 1, 2, 3):
Point, Line Or Surface? - https://biomedres01.blogspot.com/2020/02/kinetics-study-catalyze-mode-of.html
More BJSTR Articles : https://biomedres01.blogspot.com



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.