Frequency and Antibiotic Resistance of Enterobacteriaceae Isolated in Community Urinary Tract Infections at Tebessa Region
Introduction
Urinary Tract Infections (UTI) are among the most frequently acquired infections in the community, but also in hospitals and other health care institutions, causing a huge amount of antibiotic consumption [1]. The Enterobacteriaceae, including Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis and other, is the family most commonly implicated in the etiology of urinary tract infections [2]. Most frequently Escherichia coli are isolated in complicated or uncomplicated nosocomial or community acquired urinary system infections [3]. However, the antibiotic susceptibility patterns of nterobacteriaceae have been constantly changing due to the continuous development of new resistance mechanisms like the production of extended-spectrum beta-lactamases or carbapenemases by bacteria and spread of genes on mobile elements. ESBL-producing bacteria were first reported in the 1983 and are now widespread worldwide. ESBLs confer not only resistance to β-lactam antibiotics but, oftentimes, cross-resistance to other antibiotics such as aminoglycosides, trimethoprim-sulfamethoxazole, and quinolones. Antimicrobial susceptibility studies on uropathogens have been performed in many countries around the world upgrading the medical management of patients with UTIs [4].
Few Studies have Investigated the Prevalence and Risk Factors Associated with Community-Acquired UTIs
The aim of this study was thus to determine the distribution and susceptibility pattern of bacteria isolated in private laboratory from adult outpatients with urinary tract infections in Tebessa over a 3 months period, and to establish the effects of previous antibiotic use or hospitalization on rates of bacterial resistance, as well as identification of ESBL producer strains among the uropathogens. This study is important for clinician in order to facilitate the empiric treatment of patients and management of patients with symptoms of UTIs. Moreover, the data would also help authorities to formulate antibiotic prescription policies.
Material and Methods
Clinical Isolates
A total of 195 non-duplicate strains isolated from patients with urinary tract infections in the period from January 2017 to March 2017 at private laboratory in Tebessa, Algeria, were included in this study. Only strains isolated from outpatients, including patients receiving care at home, were used in the study.
Clinical Isolates
The rapid urinary screening tests are urinary sediment, dipstick, and Gram stain. The dipstick test includes pH, proteins, glucose, ketones, blood, bilirubin, urobilinogen, nitrites, leukocyte esterase and urine density. With the urine sediment test, the following data were obtained: bacteria, nitrites, erythrocytes, hemoglobin, epithelial cells and leukocytes.
Isolation and Identification of Organisms
Samples for urine culture were tested within half an hour of sampling. All samples were inoculated on orientation CHRO Magar and incubated at 37 °C for 24h, and for 48h in case no growth was observed after 24h. A specimen was considered positive for UTI in the light of the number of yielded colonies (≥105cfu/ml) and the cytology of the urine through microscopic detection of bacteriuria and PMNs (≥10 leukocytes/mm3). Identification of isolates was done up to species level using API 20E kits (bioMerieux SA, France) and vitek 2 system.
Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing and interpretation was performed using the vitek 2 system and by the disk diffusion method (Bio-Rad, France) in Mueller-Hinton agar (Bio-Rad) according to the recommendations outlined by the Comité de l’Antibiogramme de la Société Française de Microbiologie CA-SFM 2016. Sensitivity testing was done for Céfotaxim (CTX), Cefoxitin (FOX), Trimethoprim-Sulfamethoxazole (SXT), Ciprofloxacin (CIP), Amikacin (AK), Gentamycin (GN), Nalidixic Acid (NA), Furans (F) Fosfomycin (FF) for each isolate.
Extended Spectrum β-lactamase Test
Extended-Spectrum beta-Lactamase production was detected by a Double-Disk Synergy Test (DDST) and was performed by placing disks of ceftazidime, cefotaxime and aztreonam at a distance of 20 mm (centre to centre) from a disk with amoxicillin/clavulanic acid (20/10μg). Enhancement of the inhibition zone between the disks containing clavulanic acid and cefotaxime, ceftazidime or aztreonam indicated the ESBL production [5,6].
Results and Discussion
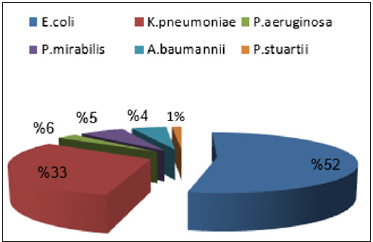
During the study period a total of 195 bacterial isolates from community acquired urinary tract infections were consecutively collected. E. coli was the most isolated organism accounting for 100 (52%). The second commonest isolate was Klebsiella pneumoniae which accounted for 64 (33%) followed by Pseudomonas aeruginosa (6%), Proteus mirabilis (5%), Acinetobacter bumannii (4%) and Providencia stuartii (1%) (Figure 1). These findings are in agreement with results found in Constantine hospital (Eastern Algeria) [7] and those reported at the University Hospital Centre of Benimessous in Algiers [8]. In contrast to our results Thirtyeight Enterobacteriaceae isolates including seventeen Klebsiella pneumonia, thirteen Escherichia coli and eight Enterobacter cloacae were recovered from community-acquired urinary-tract infections at four private-laboratories in Bejaia, Algeria, between March 2007 and May 2009 [9]. In comparison with European regions our study showed that E. coli was less frequent than in France 73% [10] but more frequent than in Ivory Coast [11]. E. coli was the most frequent isolate (60.64% of the total isolates) in a study performed in Lebanon [12].
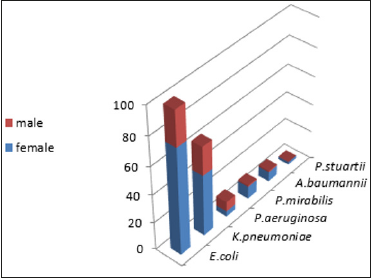
Our results about the sex category most affected by Causative microorganisms for CA-UTI. Show that women are most affected urinary tract infection as this is the most common infection (Figure 2). The development of UTIs depends essentially on anatomical factors and on the physiology of urinary tract infection which is usually ascending; there is a strong colonization of the perineum by enterobacteria of digestive origin, in particular E. coli. Our results showed that women are most affected urinary tract infection. They are particularly at risk of developing UTIs because of their short urethra, and certain behavioral factors which include delay in micturition, sexual activity and the use of diaphragms and spermicides which promote colonization of the periurethral area with coliform bacteria. Infection in women most often results from perineal or periurethral bacteria that enter the urethra and ascend into the bladder, often in association with sexual activity, or due to mechanical instrumentation such as catheterization [13,14].
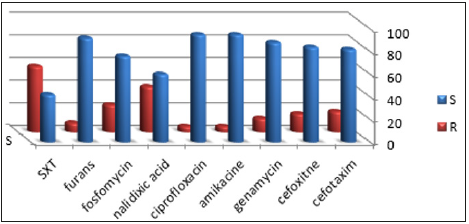
The antibiotic resistance rates of the isolates are summarized in Figure 3. Urinary tract infections are a common problem in general practice and are usually treated empirically. Empirical treatments should be based on local data regarding common pathogens and their susceptibility to available antibiotics. The indiscriminate use of antibiotics has developed many resistant microorganisms creating immense clinical problems in the treatment of infections such as those caused by Enterobacteria strains in urinary tract infection [14].
The most of Enterobacteriaceae were susceptible to cefotaxim, cefoxitin (82%) and amikacine (95%), while and trimethoprimsulfamethoxazole showed a limited activity (Figure 3). It was noticed that resistance to trimethoprim/sulfamethoxazole and nalidixic acid were significant. Resistance to trimethoprim/ sulfamethoxazole for E. coli 49 %, for Klebsiella. 48% and for P. mirabilis was 42%. Resistance to gentamycin was observed in nine isolates of E. coli, seven isolates of Klebsiella and in five isolates of Acinetobacter bumannii. In this study the highest rate of acquired Resistance of E. coli and other Gram-negative pathogens was observed with trimethoprim/sulfamethoxazole (58%). High percentage of resistance to this antibiotic was reported in European countries and Brazil, in the range of 39- 51% [15,16].
The resistance rate to fluoroquinolones observed in this study was quite high, particularly in nalidixic acid (40%), and poses some concerns about their use in empirical treatment of UTIs. Resistance to fluoroquinolones is known to be associated with the previous use of antibiotics, particularly fluoroquinolones, and previous reports have demonstrated that underlying urinary tract diseases predispose patients to repeated UTIs and, in turn, to exposure to antibiotics such as fluoroquinolones [17-19]. Fosfomycin showed activity on 76% of the strains. On the other hand, 92% of the strains are classified with sensitivity by testing the furans. These results are relative to the one found in 2015 in France that a low resistance of the strains studied to fosfomycin with (5%) [10].
In addition, fosfomycin is spared from the multiple resistance mechanisms to which other antibiotics are exposed because of its unique structure and mode of action [20]. This study gives an idea on the rates of antibiotic resistance of the main bacteria involved in urinary tract infections and illustrate the importance of the proper use of antibiotics coupled to surveillance in order to control the spread of these resistances.
Characterization of ESBLs
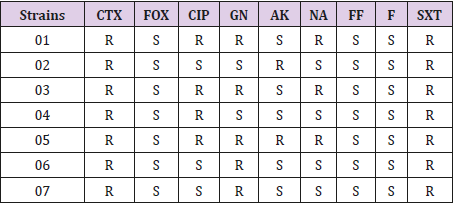
The disk diffusion method showed synergy between ceftazidime, cefotaxime, aztreonam, and amoxicillin clavulanic acid in 07 isolates of E. coli suggesting the production of Extended Spectrum Beta Lactamase (ESBL). All ESBL producing E. coli were resistant to cefotaxime, and trimethoprim-sulfamethoxazole. In contrast, these isolates were susceptible to fosfomycin, cefoxitin and furans. All but two of the ESBL producers were resistant to gentamycin. Only two of the seven ESBL producing E. coli isolates showed resistance to amikacine. Regarding quinolones resistance, three isolates were resistant to nalidixic acid and ciprofloxacin (Table 1).
ESBL producing E. coli have been described in hospitals as causing infectious outbreaks, but the presence of this microorganism has also been reported in community [21-24]. During our study, seven ESBL producing E. coli strains were isolated from the urinary tracts of seven non-hospitalized patients in Tebessa country, Algeria.
Most of the ESBL-Enterobacteriaceae isolates were resistant to the other classes of antibiotics, in particular fluoroquinolones and/or cotrimoxazole, which are commonly prescribed by general practitioners, especially for UTIs. Moreover, the high rate of resistance to fluoroquinolones was associated with ESBL production, as indicated by the marked difference in fluoroquinolones resistance observed between ESBL-producing and nonproducing isolates.
Conclusion
In conclusion the results obtained in this study suggest that E. coli is the most common cause of urinary tract infections, followed by Klebsiella pneumoniae. Urinary tract infections occur more often in women than in men. Ciprofloxacin is the most efficient agent against bacterial uropathogens and represents effective option for empirical therapy. ESBL-producing E. coli in urinary isolates is a growing problem and is spreading over the whole country. The recognition of the epidemiology and risk factors for ESBLproducing bacteria in the community may affect our management and therapeutic approach. In keeping with our finding that previous antibiotic use was the most important independent risk factor for emergence of ESBL-producing bacteria, further studies and new recommendations that guide management of UTIs and antibiotic use are warranted.
Surface Electromyography to Identify Laryngeal Tension in Selective Mutism: Could this be the Missing Link?-https://biomedres01.blogspot.com/2020/10/surface-electromyography-to-identify.html
More BJSTR Articles : https://biomedres01.blogspot.com



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.