Blue Light Exposure In The Morning and Low-Dose Aripiprazole Administration at Night Combined to Effectively Treat Wake-Up Difficulty due to Prolonged Sleep Time
Introduction
School attendance is essential for acquisition of both academic and social-emotional functions during development. In Japan, there is an increasing number of adolescents with school non-attendance, and this is recognized as a significant social concern. Although several factors can be reasons for school non-attendance caused by difficulty waking up, lack of synchronization of sleep-wake rhythms to the local time caused by chronic insufficient sleep time, delayed sleep phase syndrome (DSPS), or prolonged total sleep time are considered the most common in these students. DSPS is a circadian rhythm sleep-wake disorder (CRSWD) defined by a persistent delay in sleep onset and wake times, with excessive early day sleepiness, and extreme and prolonged difficulty awaking up with morning confusion. Additionally, prolonged sleep time is an aspect of DSPS. It is necessary to distinguish this from patterns of DSPS in patients from “normal” delayed sleep patterns commonly seen in adolescents, who prefer delayed sleep schedules as a pubertal transition without functional impairment or social distress, but it is difficult to differentiate these at the first visit to a clinic or hospital. To treat these patients, it is, therefore, advisable to carry out a combination treatment.
 Case Presentation
Case PresentationA 15-year-old otherwise healthy junior high school student presented to us with a two-year history of school non-attendance due to wake-up difficulty. Before the problem began, he had been sleeping 12 hours and attending school without any problems. From age 13, he had started excessively using the internet on his smartphone and as shown in (Figure 2), had started to have difficulty falling asleep and waking up at the desired time to prepare for school, resulting in school non-attendance. Before he came to our hospital, melatonergic administration (Ramelteon 4mg/ day) had been attempted, but there had been no improvement. On his first visit to our hospital, Ramelteon administration was discontinued, and we initiated morning blue light therapy with administration of APZ (3mg/day) at 7pm. Additionally, the patient was instructed to go to bed as 9pm. Overnight polysomnography (PSG) was performed on day 17 after treatment initiation, where we excluded sleep-related breathing disorders. We were also able to exclude hypersomnia by multiple sleep latency test consisting of 5 naps conducted on the day after PSG.
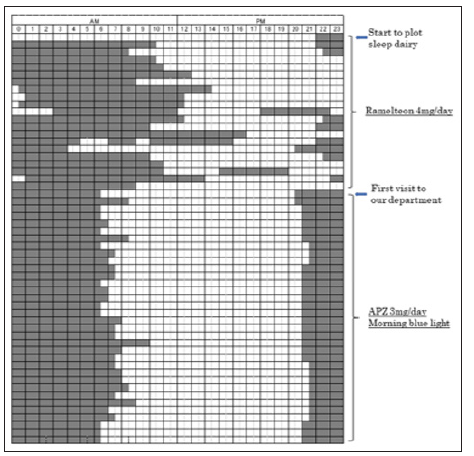 Our treatments resulted in a significantly earlier mean sleep onset and offset time, from 24.0 (22.3-24.3) PM to 21.0 (21.0-21.5) PM, and 11.0 (9.5-12.8) AM to 7.5 (6.5-8.0) AM, respectively. The mean total sleep time was significantly reduced from 12.5 (10.8- 13.3) to 10.0 (9.5-10.5) hours. Soon after intervention, advances in sleep phase occurred (Figure 2). Additionally, daytime sleepiness as measured by Epworth Sleepiness Score (ESS), and depression as measured by using a Self-Rating Depression Scale (SDS), improved from 12 to 4 points in ESS and 42 to 38 points in SDS, respectively. Health-related quality of life as measured by SF-36 score (in physical function, vitality, social function, and mental health) also improved for each item, and the patient was able to attend school again.
Our treatments resulted in a significantly earlier mean sleep onset and offset time, from 24.0 (22.3-24.3) PM to 21.0 (21.0-21.5) PM, and 11.0 (9.5-12.8) AM to 7.5 (6.5-8.0) AM, respectively. The mean total sleep time was significantly reduced from 12.5 (10.8- 13.3) to 10.0 (9.5-10.5) hours. Soon after intervention, advances in sleep phase occurred (Figure 2). Additionally, daytime sleepiness as measured by Epworth Sleepiness Score (ESS), and depression as measured by using a Self-Rating Depression Scale (SDS), improved from 12 to 4 points in ESS and 42 to 38 points in SDS, respectively. Health-related quality of life as measured by SF-36 score (in physical function, vitality, social function, and mental health) also improved for each item, and the patient was able to attend school again.This is the first case report demonstrating the effectiveness of a combination of morning blue light, low-dose aripiprazole, and sleep hygiene education to treat a student with school nonattendance due to wake-up difficulty. Although predominantly broad spectrum white light has previously been used for bright light therapy, researchers recently reported that the circadian rhythm is more responsive to shorter wavelength light (blue to green) than longer wavelength light (yellow to red) [3]. Moreover, blue light influences wakefulness and arousal; it decreases delta-theta range power density (0.5-5.5Hz) and increases high-alpha range power density (9.5-10.0Hz) on the EEG, as well as elevating core body temperature and heart rate [4,5]. We therefore hypothesized that morning blue light exposure could be an effective treatment for these students. Experimental models showed that dopamine regulates the circadian rhythm [6], and several case reports have demonstrated that dopaminergic upregulation using low-dose APZ, a partial agonist of dopamine D2 and/or D3 receptor, advanced the sleep-wake phase and reduced total sleep time [2,7,8].
Complete Calcified Ureteral Stent: A Less Challenging Scenario When Using Adequate Technology-https://biomedres01.blogspot.com/2020/11/complete-calcified-ureteral-stent-less.html
More BJSTR Articles : https://biomedres01.blogspot.com



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.