Concomitant Frontal Fibrosing Alopecia and Alopecia Areata: Trichoscopy as a Clue to the Diagnosis
Introduction
Frontal fibrosing alopecia (FFA) and alopecia areata (AA) are disorders that affect the hair follicle, resulting in alopecia. FFA is considered an irreversible process unlike AA which is often associated with partial or complete recovery. Here, we report a case of a woman presenting concomitant FFA and AA. This association confirms the major role of trichoscopy in the differential diagnosis of scalp disorders and emphasizes on the underlying pathogenesis of both conditions.
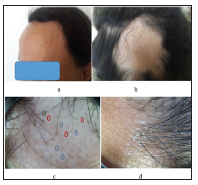
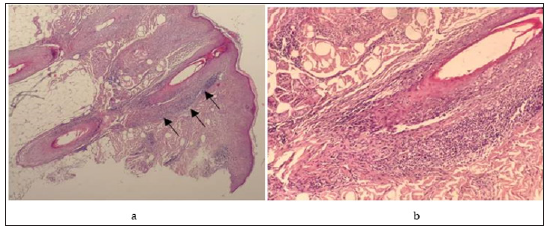
A 53-year-old postmenopausal woman presented with a twoyear- history of progressive hair loss over the occipital region associated to a symmetric recession of fronto-temporal hairline. Her past medical history included hypothyroidism treated with levothyroxine and heart valve replacement under therapy of warfarin and propranolol. Clinical examination showed a symmetric bandlike recession of the fronto-temporal hairline leaving uniformly pale skin (Figure 1a). In the occipital area, a well circumscribed, ten centimetre, patch of non-scarring alopecia was observed (Figure 1b). Examination of the eyebrows and the eyelashes was normal. There were no other skin, nail or mucosal abnormalities. Dermoscopic examination was performed in both regions. In the occipital bald patch, dermoscopy showed brocken hairs, yellow and black dots (Figure 1c). Over the frontal hairline, we observed absence of vellous hairs, a loss of follicular openings, a perifollicular hyperkeratosis and lone hairs. None of yellow dots, exclamation mark hairs or black dots was observed (Figure 1d). Histological examination of a scalp punch biopsy guided by dermoscopy from the frontal hairline showed a prominent perifollicular lymphocytic infiltrate in a lichenoid pattern that targets the isthmus of follicles and spares the hair bulb, leading to the diagnosis of FFA (Figures 2a & 2b).
a. Band-Like Recession of the Fronto Temporal Hairline.
b. Well Circumscribed, Ten Centimetre, Patch of Nonscarring Alopecia in the Occipital Area.
c. In the Occipital Bald Patch: Brocken Hairs (Green), Yellow Dots (Blue) and Black Dots (Red).
d. Over the Frontal Hairline: Absence of Vellous Hairs, A Loss of Follicular Openings, Perifollicular Hyperkeratosis and Lone Hairs.
 a. Lichenoid Infiltrate Targeting The Infundibular and the Isthmus and Sparing the Hair Bulb.
a. Lichenoid Infiltrate Targeting The Infundibular and the Isthmus and Sparing the Hair Bulb.b. Lymphocytic Inflammatory Infiltrate Around the Infundibular and the Isthmus.
Figure 2:
 Collectively, these findings suggest an association between FFA and occipital patchy AA. The patient was treated with intralesional triamcinolone acetonide in frontal and occipital regions once per month during 3 months. Six months later, she achieved a nearly complete hair regrowth in the occipital region (Figure 3). On dermoscopy, the perifollicular hyperkeratosis at the frontotemporal hair margin was still observed. There had been no progression of the hairline recession. The differential diagnosis between FFA and ophiasis variant of AA may be difficult as both diseases are characterized by band like recession of fronto-temporal hairline [1] as observed in our patient. The presence of a patch of non-scarring alopecia in occipital area was consistent with the diagnosis of AA. The trichoscopy helped to make the diagnosis of FFA in the frontal region by revealing typical features which are absence of vellus hairs, loss of follicular orifices and perifollicular hyperkeratosis.
Collectively, these findings suggest an association between FFA and occipital patchy AA. The patient was treated with intralesional triamcinolone acetonide in frontal and occipital regions once per month during 3 months. Six months later, she achieved a nearly complete hair regrowth in the occipital region (Figure 3). On dermoscopy, the perifollicular hyperkeratosis at the frontotemporal hair margin was still observed. There had been no progression of the hairline recession. The differential diagnosis between FFA and ophiasis variant of AA may be difficult as both diseases are characterized by band like recession of fronto-temporal hairline [1] as observed in our patient. The presence of a patch of non-scarring alopecia in occipital area was consistent with the diagnosis of AA. The trichoscopy helped to make the diagnosis of FFA in the frontal region by revealing typical features which are absence of vellus hairs, loss of follicular orifices and perifollicular hyperkeratosis. Scalp biopsy established a definitive diagnosis of FFA. The histological hallmark of this disease is the presence of lichenoid infiltrate targeting the isthmus and infundibular regions of follicles. This infiltrate spares the hair bulb unlike in AA [1]. Typical trichoscopic features could substitute for biopsy in the diagnosis of FFA [2]. In AA, trichoscopy detects exclamation mark hairs, yellow dots, black dots and brocken hairs, which are characteristic for the diagnosis. However, it has been reported that trichoscopic signs of AA may be noticed at the occiput in FFA patients with extended alopecia [3]. In our patient, the diagnosis of AA in occipital region was further supported by the hair regrowth after intralesional corticosteroids. While there was no hair growth in the frontal region. AA is a T cell dependent autoimmune disease due to a collapse of immune privilege (IP) in the bulb of the hair follicle. In fact, both the bulb and the bulge are normally protected by local immunosuppressive mechanisms from autoimmune attacks. In parallel, it has been postulated that FFA is caused by the same IP collapse but at the level of the bulge, home of epithelial hair follicle stem cells [4]. Indeed, FFA is presumed to mirror the immune process underlying AA, affecting the bulge instead of the bulb [5]. Previous reports of this association described two patients presenting FFA with past history of AA. The authors hypothesized that patients who have once lost IP at the bulb, are again prone to IP loss at the bulge later in life through the same mechanism [6]. To our knowledge, the concomitant association of FFA and AA has not been reported previously.
Scalp biopsy established a definitive diagnosis of FFA. The histological hallmark of this disease is the presence of lichenoid infiltrate targeting the isthmus and infundibular regions of follicles. This infiltrate spares the hair bulb unlike in AA [1]. Typical trichoscopic features could substitute for biopsy in the diagnosis of FFA [2]. In AA, trichoscopy detects exclamation mark hairs, yellow dots, black dots and brocken hairs, which are characteristic for the diagnosis. However, it has been reported that trichoscopic signs of AA may be noticed at the occiput in FFA patients with extended alopecia [3]. In our patient, the diagnosis of AA in occipital region was further supported by the hair regrowth after intralesional corticosteroids. While there was no hair growth in the frontal region. AA is a T cell dependent autoimmune disease due to a collapse of immune privilege (IP) in the bulb of the hair follicle. In fact, both the bulb and the bulge are normally protected by local immunosuppressive mechanisms from autoimmune attacks. In parallel, it has been postulated that FFA is caused by the same IP collapse but at the level of the bulge, home of epithelial hair follicle stem cells [4]. Indeed, FFA is presumed to mirror the immune process underlying AA, affecting the bulge instead of the bulb [5]. Previous reports of this association described two patients presenting FFA with past history of AA. The authors hypothesized that patients who have once lost IP at the bulb, are again prone to IP loss at the bulge later in life through the same mechanism [6]. To our knowledge, the concomitant association of FFA and AA has not been reported previously.The diagnosis of AA and FFA is sometimes challenging since clinical features may overlap, especially in the ophiasis variant of AA. Trichoscopy has proved to be a valuable tool to help diagnosis. Recent studies suggest that AA and FFA are both T-cell dependent autoimmune disorders that target different parts of the hair follicle, but the potential relationship of these diseases needs further research.
a) The diagnosis of alopecia areata and frontal fibrosing alopecia is sometimes challenging especially in the ophiasis variant of alopecia areata.
b) Trichoscopy has proved to be a valuable tool to help differential diagnosis between alopecia areata and frontal fibrosing alopecia.
More BJSTR Articles : https://biomedres01.blogspot.com



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.