Prevalence of Diabetic Foot Lesions in Patients With Diabetes Mellitus Under Chronic Hemodialysis in El Gharbia Government Hospitals
Introduction
Diabetes mellitus is a clinical syndrome characterized by hyperglycaemia owing to absolute or relative insulin deficiency. Long-standing metabolic imbalance can lead to development of the complications of diabetes, which typically affect the eye, kidney and nervous system [1]. Several pathogenic processes are tangled in the development of diabetes. These range from autoimmune destruction of the β cells of the pancreas with significance insulin deficiency to abnormalities that result in resistance to insulin action. The basis of the abnormalities in carbohydrates, fats, and protein metabolism in diabetes is deficient action of insulin on target tissues. Type 2 diabetes is most common form of diabetes accounting for 90% of cases [2]. Diabetes mellitus is increasing at epidemic proportion worldwide by 2030 there will be 366 million diabetics in the world because of changing dietary lifestyles and longer life expectancy. Egypt will have at least 8.6 million adults with diabetes and will be the tenth largest populations of diabetics in the world. The eleventh most significant cause of premature mortality in Egypt is diabetes mellitus.
It is responsible for 2.4% of all mortality annually it is also the six most significant cause of frailty in Egypt. It ruins quality of life of patients [3]. Intensive glycaemic control can reduce diabetes complications. In fact, in the last decades, rates of micro vascular and macro vascular complications of diabetes and deaths from hyperglycaemic crisis have considerably decreased. However, complications of diabetes remain the greatest health hazard to people living with diabetes [4]. Diabetic kidney disease, or CKD attributed to diabetes, occurs in 20-40% of patients with diabetes [5-8]. Diabetic kidney disease classically develops after diabetes duration of 10 years in type 1 diabetes, but may be present at diagnosis of type 2 diabetes. Diabetic kidney disease can progress to end-stagerenal disease (ESRD) needing dialysis or kidney transplantation and is the principal cause of ESRD in the United States [9]. Diabetic peripheral neuropathy (DPN) has been associated with chronic pain, sleep disturbance, depressed mood, reduced productivity, and impaired quality of life. It increases the risk for burns and injuries and is risk factor for diabetic foot ulcers, the principal cause of non traumatic lower extremity amputation [10]. Patients with diabetes on haemodialysis are at increased risk of foot complications, which may finally result in lower extremity amputations, resulting in the loss of parts of toes, feet or even legs. Repetition of these problems in the contralateral limb is frequent. Foot complications are more established in patients with longstanding diabetes and end stage renal disease compared with individuals without end stage renal disease [11]. The non-traumatic amputation rate among patients with diabetes on haemodialysis in USA was 10 times as great as among the diabetic populations, suggesting that diabetes is a major risk factor for lower limb amputation in haemodialysis patients. Amputations are associated with reduced quality of life, morbidity, and increased mortality [12].
Subjects and Methods
This is a cross sectional analytical study carried out in patients with diabetes and chronic renal failure for at least 6 months attending all 10 dialysis units in EL Gharbia Government hospitals and this study was carried upon 571 hemodialysis patients. An informed consent was obtained from all participants in the research. All participant’s names will be hidden and will be replaced by code numbers to maintain privacy. The study protocol was approved by the Local Research Ethics Committee of the Faculty of Medicine, Tanta University, and was in accordance with the principles of the Declaration of Helsinki II.
Inclusion criteria:
a) Patients with diabetes mellitus on chronic hemodialysis for at least 6 months.
b) Exclusion criteria:
c) Non-diabetic patients under chronic hemodialysis.
d) Diabetic patients under chronic hemodialysis for period less than 6 months.
Subjects were divided into four groups: Group 1 (Patients without distal sensory neuropathy), Group 2 (Patients with distal sensory neuropathy), Group 3: (Neuropathic patients with some grade of PAD (peripheral arterial disease) and or foot deformity) and Group 4: (Neuropathic patients with foot ulcer or a history of prior lower-limb amputation). Subjects were subjected to the following: Full history taking, Complete clinical examination and Investigations including Fasting and post prandial blood glucose, Albumin/Creatinine ratio, Complete blood count, Liver function tests, Serum Creatinine and blood urea, Total lipid profile, Sodium and potassium, Ankle brachial index (ABI) and Carotid Doppler ultrasound for measurement of intima media thickness (IMT).
Statistical Analysis
Statistical presentation and analysis of this study was conducted, Continuous quantitative variables were expressed as means + SD. Analysis of variance (ANOVA) test was used. P-values <0.05 were considered significant. The computer SPSS program was used for all statistical calculations (Statistical Package for the Social Science; SPSS, Chicago, USA) version 21 for Microsoft Windows, USA.
Results
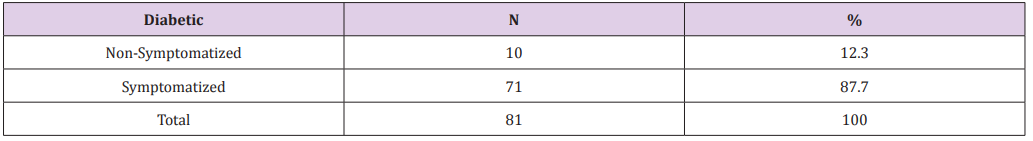
The demographic and clinical data of all participants are shown in Table 1. Among 81 diabetic patients under chronic hemodialysis there were 7 patients (70.0%) males non- symptomatized and 3 patients (30.0%) females non-symptomatized also, there ages range from 24 to 68 years old. Among 71 symptomatized patients there were 28 patients (39.4%) symptomatized males and 43 patients (60.6%) symptomatized females. There ages range from 37 to 67 years old. The duration of diabetes ranged from 3 to 30 years. There was significant statistical relation between duration of diabetes and the development of micro vascular complications of diabetes (P. value 0.041*) as shown in Table 2. The duration of dialysis ranged from 6 to 24 months. Regarding type 1 diabetics: only one patient (10.0%) who did not suffer from distal sensory neuropathy while 4 patients (5.6%) were symptomatized and regarding to type 2 diabetics: There were 9 patients (90.0%) non symptomatized patients while 67 patients (94.4%) were symptomatized. The prevalence of diabetic patients among patients under chronic hemodialysis is shown in Table 3. The table reveled that, among all patients recorded from the chosen hemodialysis units 81 patients (14.2%) were diabetic. Among 81 diabetic patients there were 10 patients (12.3%) do not suffer from distal sensory neuropathy. While 71 patients (87.7%) were suffering from various diabetic foot lesions as shown in Table 4.
Table 1: Distribution of the studied patients according to their sex and age.
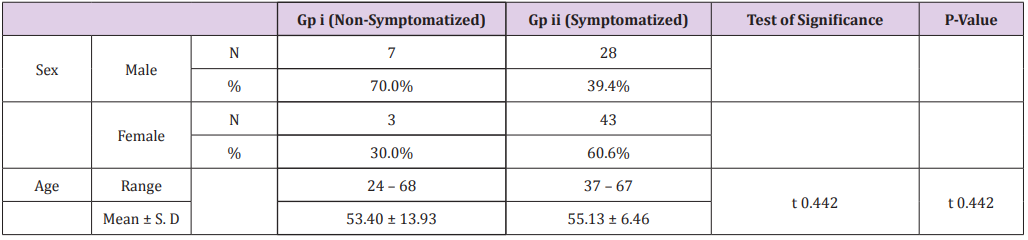
Table 2:Distribution of the studied patients according to duration of diabetes by years and duration of dialysis by month and type of diabetes.
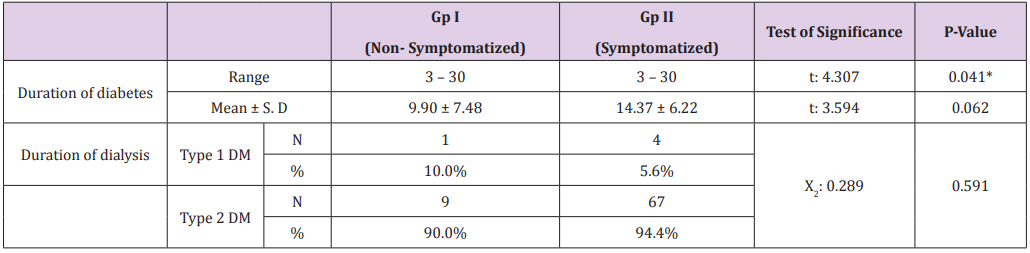
Table 3:Prevalence of diabetic patients among patients under chronic hemodialysis.
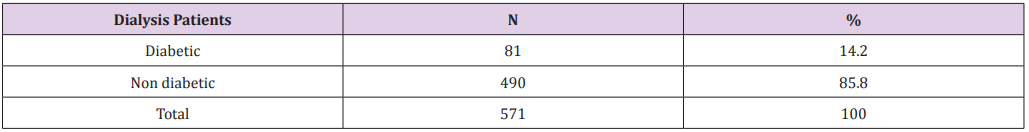
Table 4: Prevalence of diabetic foot lesions among diabetic patients under hemodialysis.
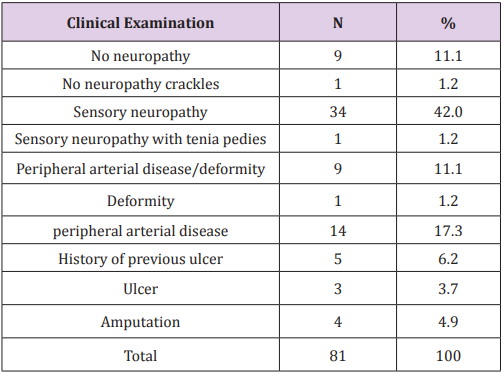
Types of diabetic foot lesions were shown in Table 5 and (Figure 1) that reveled, patients with diabetic foot lesions can be classified into three various groups: Gp a: with sensory neuropathy only included 35 patients (49.4%), Gp b: included 24 patients with peripheral arterial disease with or without deformity (33.8%) and Gp c: included 12 patients with ulcer (Figure 2), history of ulcer or amputation (16.8%). There were 9 patients (11.1%) do not have neuropathy and one patient (1.2%) does not have neuropathy but has crackles, whereas 34 patients (42.0%) have sensory neuropathy, while one patient(1.2%) has sensory neuropathy with tenia pedies, while 9 patients (11.1%) have peripheral arterial disease plus deformity, whereas one patient (1.2 %) with deformity, whereas 14 patients (17.3%) with peripheral arterial disease, while 5 patients (6.2%) with history of pervious ulcer, whereas 3 patients (3.7%) with ulcer, while 4 patients (4.9%) had amputation as shown in Table 6.
Figure 1:Types of diabetic foot lesions among symptomatized patients.
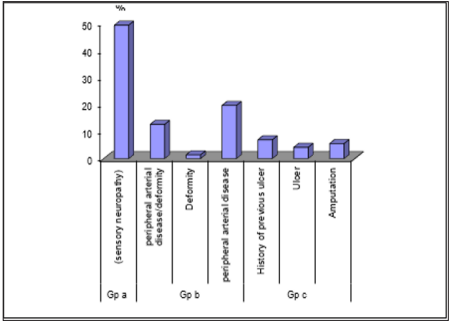
Figure 2:Ulcer at the fifth toe.

Table 5: Types of diabetic foot lesions.
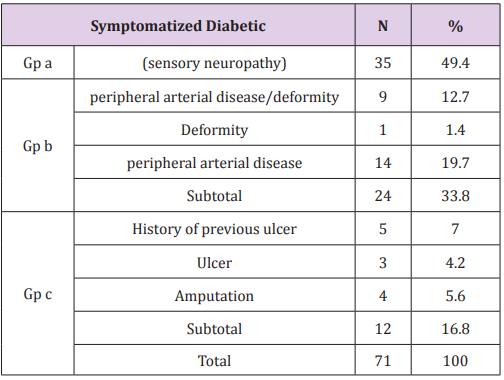
Table 6: Distribution of the studied patients according to their diabetic foot lesions.
According to ankle brachial resistive index: all non symptomatized patients had normal ankle brachial index, while 26 (36.6%) symptomatized patients had normal ankle brachial index, whereas 33 (46.5%) symptomatized patients had moderate limb ischemia, and 12 (16.9%) symptomatized patients had critical limb ischemia. This difference was statistically significant. According to intima media thickness: there were 2 (20.0%) non symptomatized patients with normal intima media thickness, while 2 (20.0%) non symptomatized patients with decreased intima media thickness, whereas 6 (60.0%) non symptomatized patients with increased intima media thickness, while there were 3 (4.2%) symptomatized patients with normal intima media thickness, whereas 1 (1.4%) symptomatized patients with decreased intima media thickness, while 67 (94.4%) symptomatized patients with increased intima media thickness. This difference was statistically significant as shown in Table 7.
Table 7: Distribution of the studied patients according to their radiological examination
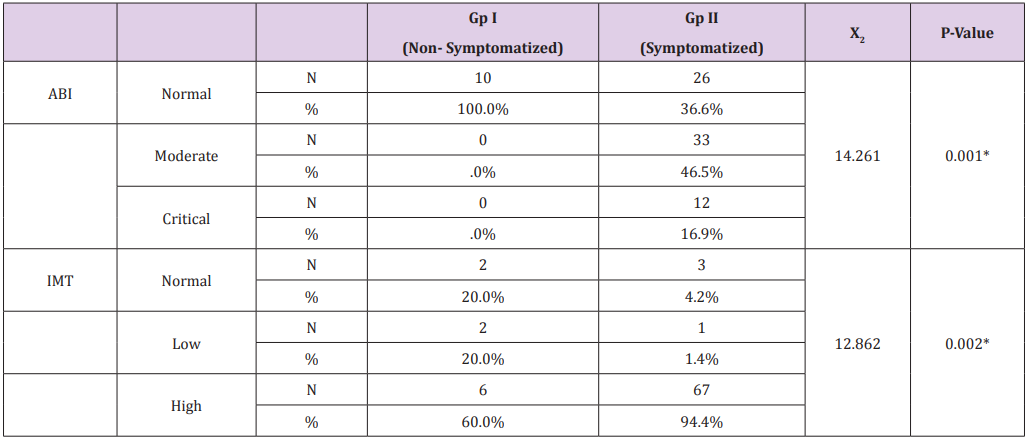
Note: ABI: ankle brachial resistive index.s; IMT: intima media thickness.
Discussion
Diabetic peripheral neuropathy DPN has been linked to chronic pain, sleep disturbance, depressed mood, reduced productivity, and impaired quality of life. It increases the risk for burns and injuries and is risk factor for diabetic foot ulcers, the leading cause of nontraumatic lower extremity amputation [13]. In the symptomatized patients there was 35 patients (49.4%) have sensory neuropathy, 9 patients (12.7%) have peripheral arterial disease and deformity, while one patient (1.4%) has deformity, whereas 14 patients (19.7%) have peripheral arterial disease only, on the other hand 5 patients (7%) have history of pervious ulcer, while 3 patients (4.2%) have ulcer, whereas 4 patients (5.6%) had amputation. These findings are in agreement with study done by Doria et al. [14] indicated that in his study, A total of 92 patients (35.8%) out of the 257 who were receiving renal replacement treatment (89.1%) patients have peripheral neuropathy, while (64.2%) patients have peripheral arterial disease, whereas (54.3%) patients have foot deformities, while patients have pervious ulcer (19.6%), whereas patients have diabetic foot (17.4%), and (16.3%) have amputation [14] and indicated that diabetic peripheral neuropathy occurs not only as a result of hyperglycaemia.
But several other metabolic and vascular mechanisms are also involved. The results of his study revealed that patients with diabetic peripheral neuropathy were older and had a more prolonged duration of diabetes than patients without diabetic peripheral neuropathy. Age and duration of diabetes are well documented risk factors for the development of diabetic neuropathy. Increasing age and disease duration imply a longer period of insult to the peripheral nerves. With regards to macro vascular changes, a significant difference was noted on the prevalence of atherosclerotic changes in the carotid and/or lower limb arteries, but no significant difference was shown in the prevalence of peripheral arterial disease PAD as detected on ankle brachial index ABI Yuki et al. [13,15] reported that peripheral arterial disease is one of the important determinants of overall survival in patients on haemodialysis. The survival rates of Japanese haemodialysis patients without PAD were 94% at 1 year and 73% at five years, and rates in haemodialysis patients with PAD were 90% at 1 year and 59% at 5 years. In contrast, the survival rates of haemodialysis patients with foot lesions in these series were very poor, at 65% at 1 year, 36% at 3 years, and 23% at 5 years, with a mean survival of only 1.8 years [15].
Foot ulceration or amputation was more common in people with longer duration of diabetes, and lower serum albumin levels. These data suggest strongly that dialysis patients with pervious foot ulceration (Figure 3) or limb loss and those with peripheral arterial disease face extremely high risks of disabling complications this was in agreement of our study [16]. We did not systematically assess the site and severity of peripheral oedema and the severity of peripheral arterial disease, which are potential confounders of the relationship between dialysis therapy and ulceration. Although not all studies have been able to demonstrate that prevention programmes in diabetes are able to reduce ulcer incidence (Figure 4). In a haemodialysis patients, foot care education, foot assessment and provision of special shoes was associated with favourable outcomes. The institution of multi-disciplinary foot care for those with diabetic foot lesions and pervious renal transplantation resulted in reduction in episodes of gangrene and major amputation; ulcer healing times were reduced to those previously reported in diabetic patients without renal transplant [17].
Figure 3:claw toes and healed ulcer at the top of the second toe.

Figure 4: crackles at the sole and heel of the foot.

Conclusion
The longer the duration of diabetes the more the patients are prone to the development of diabetes complications, diabetic patients under hemodialysis had a high prevalence of diabetic foot lesions, and most of them had one or more risk factors for developing an ulcer in the future. We suggest that all such patients should be considered at high risk and that proper foot care including preventive measures (e.g., scheduled foot examinations and education) and therapeutic intervention should be a must for all diabetic subjects in or initiating hemodialysis.
Darbepoetin Alpha For the Treatment of Anemia in Systemic Mastocytosis-https://biomedres01.blogspot.com/2021/01/darbepoetin-alpha-for-treatment-of.html
More BJSTR Articles : https://biomedres01.blogspot.com



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.