Less than 30 Minutes of Door to Balloon Time can Completely Alter the Clinical Course of the Right Ventricular Myocardial Infarction
What is Already Known?
Inferior MI complicated with right ventricular MI has a higher mortality rate than isolated inferior MI. Early revascularization is the key to reduce mortality rates in this high-risk subset.
What this Study Adds?
The study showed that, there is no difference in mortality and morbidity between patients with pure IMI and patients complicated by RVMI, when early and successful reperfusion therapy was performed with a D2B time of less than 30 minutes. According to our results, the main target in the therapy of RVMI should be decreased total ischemic time and increased post-PCI TIMI flows.
Introduction
There is limited data on the association between right ventricular (RV) function and adverse events after acute right ventricular myocardial infarction (RVMI) [1]. Most of the information on RVMI is from the pre-mechanical revascularization era. RVMI increases the risk of hemodynamic instability, atrioventricular conduction block and increases in-hospital mortality in patients with inferior myocardial infarction (IMI) [2,3]. Significant improvement in the prognosis of RVMI was achieved after reperfusion treatments. However, studies have demonstrated that RVMI is still associated with significant morbidity and mortality, even in the mechanical reperfusion era [4]. A shorter time taken to reperfusion of the occluded vessel contributes to the recovery of RV function. Early revascularization plays an important role in the recovery of RV function; conversely, late revascularization is associated with higher RV dysfunction and complications [5,6]. The purpose of the current study was to investigate the complication rates in patients with IMI with and without RVMI who were treated with early primary percutaneous coronary intervention (PPCI) successfully.
Methods
Patient Selection and Study Protocol
Consecutive patients, admitted with IMI due to proximal right coronary artery (RCA) occlusion and treated with successful PPCI, were included to the study. There was no critical stenosis in the other vessels
Successful PPCI was defined with three criteria:
a) TIMI 3 coronary flow (complete perfusion) after PPCI.
b) Resolution of ST segment elevation > 70%
c) Complete relief of chest pain.
If any of these three criteria was absent, the patient was excluded from the study. The population of this study was specified as patients who have had chest pain within 6 hours. The patients with onset of symptoms over 6 hours were excluded. IMI was diagnosed as the presence of ST segment elevation of at least 0.1 mV in 2 or more inferior leads on electrocardiography (ECG). RVMI was diagnosed as the presence of ST segment elevation in the V4R lead on ECG. All patients were treated according to the institutional acute myocardial infarction protocol, which is driven by the most recent guidelines. In addition, 2D echocardiography was performed to all patients within 24 hours of admission. LV and RV function were determined by echocardiography. All patients were followed prospectively for the occurrence of adverse events.
Data recorded for all patients included demographics, ECG findings, a detailed timeline including time of onset of chest pain, time of arrival at hospital (“door” time) and time of first balloon inflation of the primary angioplasty procedure (“balloon” time). The time interval between the patient’s first arrival at hospital and first balloon inflation was called as door-to-balloon (D2B) time. TIMI risk scores were calculated from the initial clinic history, electrocardiograms, laboratory values collected on admission. After discharge, the patients were evaluated by telephone calls or by hospital checkup programs. The mean follow-up period was 10 months after discharge. The study protocol was approved by the Local Ethics Committee.
Echocardiography
Images were obtained in the left lateral decubitus position using a commercially available system (Vivid 3 pro General Electric-Vingmed, Horton, Norway). Data acquisition was performed at a depth of 16 cm in the parasternal and apical views using a 3.5- MHz transducer. During breath-hold 2D images were obtained and 3 consecutive beats were saved in cineloop format. The reference limits of all echocardiographic parameters were defined according to American Society of Echocardiography Guidelines. The left ventricle end-systolic volume (LVESV), left ventricle end-diastolic volume (LVEDV) were assessed and LV ejection fraction (LVEF) was calculated by using the biplane Simpson method [7].
RV Function Analysis
RV end-diastolic diameter (RVDD) was measured in the apical 4- chamber view. RV fractional area change (RVFAC) was analyzed by tracing the RV end-diastolic area (RVDA) and RV end-systolic area (RVSA) in the apical 4-chamber view using the formula (RVDA-RVSA)/ RVDA x 100. Tricuspid annular plane systolic excursion (TAPSE) was measured in the RV free wall. In the apical 4-chamber view, the M-mode cursor was placed through the tricuspid annulus in such a way that the annulus moved along the M-mode cursor and the total displacement of the RV base from end-diastole to end-systole was measured [8].
Statistical Analysis
Continuous data were presented as mean standard deviation and categorical data were presented as frequencies and percentages. Differences in characteristics between patient groups were evaluated using the unpaired Student t test and chi-square test. Pearson’s chi-square test was used for non-qualitative data when the data were examined (Fisher’s exact Chi-square test was used when the number of value (n) in boxes was below 5). Mann-Whitney U test was used for data not showing normal distribution and Student T test was used for data with normal distribution. The 95% confidence interval was determined and differences were considered significant at 𝑃 < 0.05.
Results
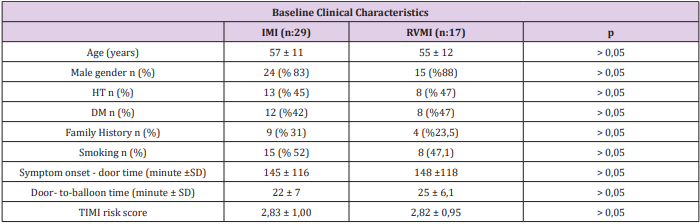
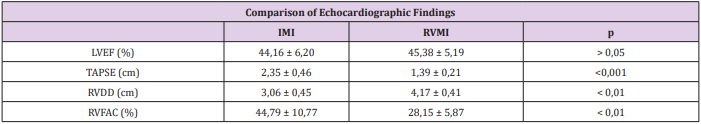
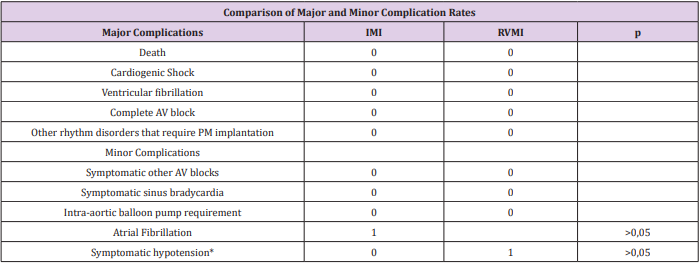
The study population consisted of 46 consecutive patients, admitted with IMI and treated with PPCI. 16 patients had IMI complicated by RVMI. Table 1 summarizes the clinical characteristics of the patient population. Mean age was 56 years, and most patients were men (n: 39; 85 %). The patients presented a mean of 146 ± 117 minutes after the onset of symptoms. The average D2B time at our study population was less than 30 minutes (mean 23.1 ± 6.6 minutes). Patients with RVMI had significantly lower TAPSE (1.39 ± 0.21 cm vs 2.35 ± 0.46 cm, P<0.001) and RVFAC (28.15 ± 5.87 vs 44.79 ± 10.77 p<0,001) and significantly higher RVDD (4.17 cm ± 0.41 vs 3.06 ± 0.45, p< 0.001). No difference was observed in LVEF between the patients with and without RVMI (45.38 ± 5.19 % vs 44.16 ± 6.20 %, P> 0.05) (Table 2). No mortality or major complication was observed during the intensive coronary care unit (ICCU) and hospital stay. A minor complication was observed in one patient with RVMI, this was not statistically significant (p > 0.05). Atrial fibrillation was detected in one patient in IMI group and this was not statistically significant too (P> 0.05) (Table 3).
Table 1: Baseline Clinical Characteristics.
DM: Diabetes Mellitus, HT: Hypertension, IMI: Inferior myocardial infarction, RVMI: Right ventricular myocardial infarction SD: Standard deviation, TIMI: Thrombolysis in Myocardial Infarction
Table 2: Comparison of Echocardiographic Findings.
IMI: Inferior myocardial infarction, LVEF: left ventricular ejection fraction, RVFAC: Right ventricular fractional area change, RVMI: Right ventricular myocardial infarction, TAPSE: Tricuspid annular plane systolic excursion
Table 3: Comparison of Major and Minor Complication Rates
IMI: Inferior myocardial infarction, PM: Pace Maker, RVMI: Right ventricular myocardial infarction
*Inotropic treatment requirement symptomatic hypotension.
Length of stay in ICCU was slightly higher in RVMI group but it was not statistically significant (p>0.05) (Table 4). There was no statistically significant difference between two groups with respect to peak CK-MB levels (p> 0.05). When correlation analysis was performed between peak CK-MB values and length of hospital stay, no significant correlation was found between the length of ICCU / hospital stay and peak CK-MB values in patients with IMI (p> 0.05). However, a significant positive correlation was found between the peak CK-MB values and both length of ICCU and hospital stay in patients with RVMI. (Hospital stay r: 0.668, p<0.001; ICCU stay r: 0.803, p<0.001). After an average of 10 months follow up of patients, no new infarction or mortality was observed in both groups.
Discussion
Our study showed that IMI complicated with RVMI did not increase mortality and morbidity when early and successful reperfusion was performed. Recently many clinical trials showed that, rapid administration of intravenous thrombolytic therapy and increasing use of primary angioplasty reduce mortality and contribute to the shorter hospital stays [9,10]. Although the benefits of these treatments have been demonstrated, over 25% of patients presenting within the first 12 h of symptom onset with ST segment elevation or left bundle branch block fail to receive a reperfusion intervention. It is clear that outcomes for ST elevation myocardial infarction (STEMI) patients are optimized when D2B times are less than 90 minutes [11,12]. Multiple studies also demonstrated that mortality rates improve by achieving decreased D2B times [13]. A review of a large cardiovascular registry (10,965 patients) found that the median D2B time was 96 minutes and only 44% of the patients were meeting the <90-minute national benchmark goal [14]. Cannon et al. showed that mortality increased by 41% for STEMI patients with D2B times over 120 minutes [10].
In our study, the mean D2B time was less than half an hour. Furthermore, the median time from onset of chest pain to hospital arrival was less than 2.6 hours and the median time from onset of chest pain to PPCI was less than 3 hours. The low rate of mortality and morbidity in our study can be explained by early reperfusion therapy. The risk of major complications and in-hospital death is about 31% in IMI patients with RVMI compared to about 5% in IMI without RVMI [2]. The analysis of the SHOCK registry data showed that the patients with predominant RV shock have a high mortality rate despite the younger age, lower rate of anterior MI, and higher prevalence of single-vessel coronary disease. Early reperfusion (PPCI or fibrinolytic therapy) can preserve both right and left ventricular function and also reduce morbidity and mortality [15-17]. Schuler et al. indicated that in most patients with proximal occlusion of the RCA, early reperfusion with thrombolytic therapy contributes to improvement of initially depressed RV function; often, recovery of RV myocardial function is not associated with the changes in LVEF. In contrast, in patients with persistent occlusion, irreversible cardiogenic shock and early death may occur due to RV infarction, despite adequate LV performance [16].
Bowers et al. demonstrated that, complete reperfusion of the RCA by PPCI, results in the dramatic recovery of RV function and an excellent clinical outcome, in patients with RVMI. In contrast, unsuccessful or late reperfusion results in impaired recovery of RV function, persistent hemodynamic compromise, and a high mortality rate [15]. Our study population consisted of patients who underwent early and successful reperfusion treatment. And our results showed that there is no increase in the rate of major complications and in-hospital death in patients with IMI complicated with RVMI compared to IMI without RVMI, when early successful reperfusion therapy was performed. Right-sided ST-segment elevation, particularly in lead V4R, indicates acute RV injury and correlates closely with the proximal RCA occlusion [18,19]. In one report of 200 consecutive patients with acute IMI, the sensitivity and specificity of ST-segment elevation in V4R was shown as 88 % and 78 % (respectively) for concurrent RVMI, by using findings from the results of autopsy, cardiac catheterization, radionuclide imaging, or hemodynamic monitoring as the “gold standard” [2]. Zehender et al. demonstrated that the presence of ST-segment elevation in lead V4R predicts development of major complications and in-hospital mortality strongly and independently [2].
The presence of ST-segment elevation in lead V4R was one of the inclusion criteria for RVMI group in our study. We showed that ST- segment elevation in lead V4R was not an independent predictor of major complications and in-hospital mortality after early successful reperfusion treatment. Anavekar et al. and Zornoff et al. showed that RV function was weakly correlated with LV function and demonstrated that RV function quantified with RVFAC was independently associated with an increased risk of mortality and heart failure [20,21]. Antoni at al. showed that RVFAC and RV strain were independent predictors of the occurrence of the composite end points (all-cause mortality, reinfarction, and hospitalization for HF) [1]. Samad et al. showed that TAPSE predicted mortality independently, after adjustment for LVEF and age [22]. We found that RVFAC and TAPSE values were significantly lower and RV diameter was significantly higher in RVMI group. However, we showed that they were not predictors of mortality and morbidity when early and successful reperfusion performed. Gonzales et al. demonstrated that STEMI patients with TIMI risk classification 0-1, 2-3, and ≥4 has in-hospital mortality of 7%, 13% and 26%, respectively [23].
In our study, the mean TIMI risk score of the patients was 2.83 ± 1.0. However, after early reperfusion treatment there was no mortality in our study. We showed that clinical outcomes could be changed by early reperfusion therapy in patients with RVMI. We found a significant correlation between peak CK-MB level and length of ICCU/ hospital stay in RVMI patients. In fact, there was no statistically significant difference with respect to peak CK-MB level between patients with and without RVMI. Furthermore, the peak CK-MB level was not associated with the development of complications and the length of hospital stay in patients without RVMI. However, the length of hospital stay was prolonged in patients complicated with RVMI who have higher peak CK-MB levels. This was substantially related to increased length of ICCU stay. Increased length of ICCU stay was probably due to the clinician’s concern about RVMI-related complications. Our study showed that the increase of peak CK-MB level was not associated with the development of complications when early and successful reperfusion was performed.
Limitations
The main limitation of our study was the small number of patients. Our results should be tested with more patients in largescale studies. The absence of the patients who have longer door to balloon times may be accepted as a limitation of the study, but the mean door to balloon time is short in our center.
Conclusion
We conclude that, there is no difference in mortality and morbidity between patients with pure IMI and patients complicated by RVMI, when early and successful reperfusion therapy was performed with a D2B time of less than 30 minutes.
Multi-Component Exercise Program and Improving Physical Performances in Older Inpatients: Results from A Pilot Interventional Study-https://biomedres01.blogspot.com/2021/02/multi-component-exercise-program-and.html
More BJSTR Articles : https://biomedres01.blogspot.com




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.