Comparative Evaluation of Clinical X-Ray Densitometric Parameters on the Background of Osteotropic Therapy for Knee Joint Endoprosthesis
Introduction
The most frequent causes of the development of instability of the endoprosthesis components are resorptive processes occurring in the periprosthetic bone tissue. Among all the causes of revision operations, aseptic implant loosening accounts for between 60% and 73.8% [1,2]. The reasons for such an early osteolysis after replacing the joint with an artificial one were attributed to the lack of physiological stress on the affected knee joint, as a result of the existing flexion contractures of the knee joint and the use of nonsteroidal anti-inflammatory drugs that inhibit the function of osteoblasts [3-5]. Bone tissue remodeling is a time-conjugate process: a complete remodeling cycle consists of activation of resorption, followed by activation of bone formation. Osteolysis occurs when the balanced connection between bone formation and resorption is broken. The mechanism of increasing bone resorption and reducing its formation may be associated with the quantitative predominance of functional osteoclasts over osteoblasts [6-8]. Studies based on the X-ray densitometry method show the prevalence of osteolysis in the early periods after knee joint endoprosthesis replacement compared with baseline values [9-12].
In terms of the initial inferiority of bone tissue, in the presence of concomitant osteoporosis, the problem of instability arises especially acutely in connection with the possible development of periprosthetic micro fractures [13,14]. Therefore, the preoperative drug provision of a balanced course of osteolysis and remodeling in the bone bed is an important element of the early and long-term prevention of aseptic loosening of the components of the knee joint endoprosthesis [15]. Therefore, the identification of early signs of osteolysis based on x-ray densitometry and optimal medication exposure will prevent resorption after knee arthroplasty. The aim of our study was to study the effectiveness of the effect of drug correction on the remodeling of the bones forming the knee joint before and after the endoprosthesis in a comparative aspect.
Material and Research Methods
From 2011 to 2014, in the department of adult orthopedics of the NIITO Clinic of the Ministry of Health of the Republic of Uzbekistan there were 126 patients undergoing inpatient treatment for degenerative-dystrophic diseases who were implanted with a De Puy pfc SIGMA knee joint implant with and without posterior cruciate ligament preservation with a rear stabilizer (42 endoprosthesis) according to standard technology. All patients were female, the average age of patients was 57 years (max. 84 years, min. 52 years). 48 patients suffered from primary osteoarthritis of the knee joint, 31 patients with rheumatoid arthritis, and 7 post-traumatic arthrosis of the knee joint. In all patients at the stage of preoperative examination, the terminal stage of gonarthrosis was detected with limited movement in the joint. The patients were divided into two groups of 60 people each. In the first (control) group, general drug treatment provided for the tasks of bone tissue normalization after surgical treatment from the 8th day for 12 months. The patients of the second (main) group received osteotropic drugs (bisphosphonates, calcium D3) for 6 months before the surgery and the next 6 months after implantation of the knee joint endoprosthesis.
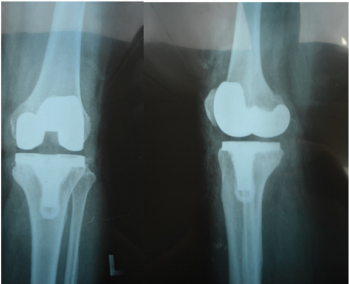
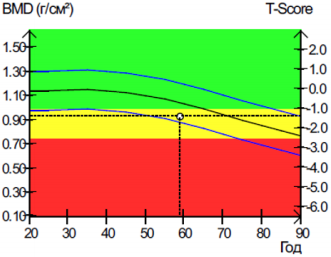
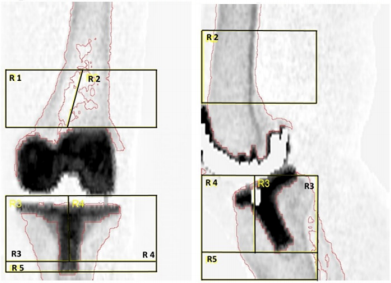
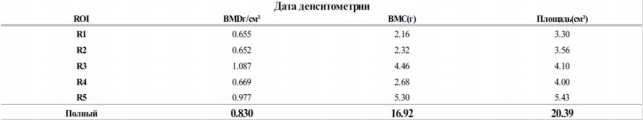
The study of the results of treatment was carried out using a clinical method for assessing the condition of the knee joint using the Lysholm Knee Scoring Scale scale, where a score of 85 points or more is regarded as excellent, 70-84 points as good, 60-69 points as satisfactory, less than 60 as unsatisfactory. The methods of computer analysis of radiographs and dual energy X-ray absorptiometry (DEXA) were used. Digital radiography of the knee joints was performed in a straight and lateral projection before and after the operation (Figure 1). The obtained data were evaluated on the scale of bone Haunsfield +700 (Spongy bone) - 3000 (dense bone), which were processed in the Trophy Windows 2000 program and were subjected to quantitative analysis, which after statistical processing indirectly allows you to determine the density of local bone areas. A systematic assessment of bone mineral density was performed using dual energy x-ray absorptiometry (DEXA) using Stratos. The technique for assessing periprosthetic bone tissue using dual energy x-ray absorptiometry (DEXA) is presented in (Figure 2). The study was conducted on standard ROI (regions of interest, R1-5) points in the frontal and lateral projection of dual energy X-ray absorption (DEXA) of both components of the knee joint endoprosthesis (Figures 3 & 4).
Figure 3: Standard ROI points (regions of interest, R1-5) in frontal and lateral projection of dual energy X-ray absorption (DEXA) of both components of the knee endoprosthesis.
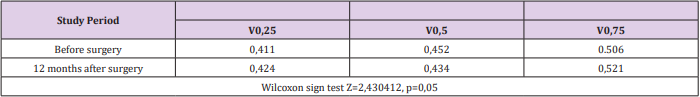
The critical level of significance when testing hypotheses of statistical processing in this study was equal to 5% (p = 0.05). Checking the normality of the distribution was carried out using the Shapiro-Wilkie method, testing hypotheses about the equality of the general variances using the Levene criterion. In case of non-normal distribution of values, median (V0.5), 25th percentile (V0.25) and 75th percentile (V0.75) were indicated in the series. Non-parametric methods were used to test statistical hypotheses: T-criterion of Wilcoxon rank signs, Pearson χ2 criterion.
Results and Discussions
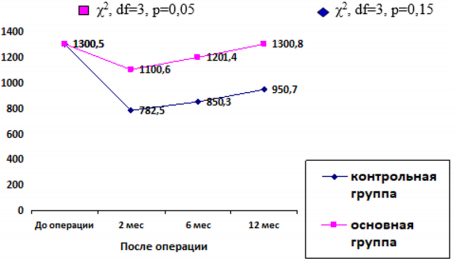
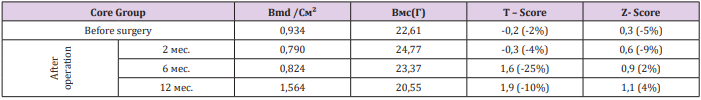
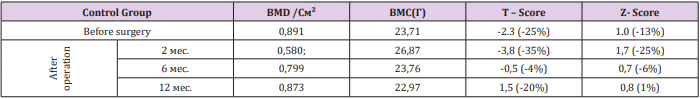
Analysis of the results of the evaluation of digital X-ray on the Haunsfield scale showed that the bone density of the tibial bone tissue in the preoperative period in the interval of 1400 ± 100 conditional units of bone density can be considered normal. After the operative period after 60 ± 3 days, bone loss was observed around the implant with a decrease in density of 35-40% in patients of the first (control group) and 10-15% of patients of the second (main group) (Figure 5). According to the data of dual energy x-ray densitometry (DEXA), according to standard ROI points, a decrease in BMDg / cm² and BMC (g) in R3, R4 is greater than R1, R2, R5. Densitometric analysis before the operation shows a decrease in bone mineral density on average T-score -2.3 (-25%), Z-score - 1.0 (-13%) in patients not taking osteotropic preparations. After the operation, after three months, osteopenia was observed in the periprosthetic zone with an average BMD / cm2 - 0.934; Navy (g) - 22.61; T - score -0.3 (-4%) Z- score 0.6 (9%) in patients taking bisphosphonates and calcium preparations D3, and in the control group, symptoms of osteoporosis were noted with a decrease in the periprosthetic average BMD / cm² - 0.580; Navy (g) 26.87; T - score -3.8 (-35%) Z-score - 1.7 (-25%). After 4 months, there was a slowdown in the rate of loss of bone tissue density in the control group by 4%, in the main group by 20%. Compared with indicators recorded by the end of 2 months, the density bone tissue increased in the control group by 15%, in the primary by 35%. Six months after the total endoprosthesis, the control group continued to slow down the rate of loss of bone tissue density.
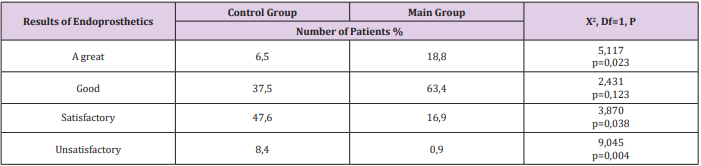
In the main group of patients who took osteotropic drugs for 6 months before surgery, bone loss was completely leveled. Moreover, compared with the rates before surgical treatment, bone density in this group increased by 4%. When analyzing the effectiveness of treatment in patients taking osteotropic drugs before surgery, statistically significant differences were found in the course of remodeling processes than in patients without osteotropic treatment (Tables 1 & 2). The growth of bone mineral density in patients of the main group, by the end of the year amounted to an average of 4% (Table 3). When analyzing the results on the Lysholm Knee Scoring Scale scale, it was stated that the percentage of excellent results was high in the group of patients who received osteotropic therapy to restore bone in the implantation zone 6 months before the surgery. In the control group, there were more satisfactory and unsatisfactory results (Table 4). The criteria in this study were pain syndrome under load, walking upstairs, patient functionality by the end of the year. Despite the osteotropic treatment carried out before the operation, there were isolated cases of unsatisfactory outcome associated with insufficient adherence to the medication regimen in patients with severe osteoporosis.
Table 4: Comparative score on a Lysholm Knee Scoring Scale scale of the results of total knee arthroplasty (n = 120).



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.