Cases of Acute Meningitis in Children, Admitted and Treated in Prince Hashim Military Hospital in Zarqa-Jordan
Bacterial meningitis is a serious life-threatening disease affecting the nervous system that needs immediate medical intervention. And the neurological sequel in such conditions following hospital discharge approaches 20%. So, it is essential for physicians to understand the clinical signs and symptoms of the disease and its management and prevention [1-4]. Worldwide Meningitis can occur independently of age health status in spite of introduction of vaccines and availability of antibiotics.
Acute Meningitis may be septic or aseptic. Aseptic meningitis is an inflammation of the meninges with sterile bacterial cultures of Cerebrospinal Fluid (CSF). The most common cause of aseptic meningitis are viral infections that usually get better without treatment [5-7]. Aseptic meningitis may be also due to “partiallytreated” bacterial meningitis, tuberculosis or fungal meningitis. However, acute bacterial meningitis is a true medical emergency, and requires immediate treatment in a hospital [8,9].
Viral meningitis is milder and occurs more often than bacterial meningitis. It usually develops in the late summer and early fall; most infections occur in children under the age of 5 years [10- 12]. Most viral meningitis cases (90%) are due to non-polio enteroviruses, which are viruses that also cause intestinal illness. About half of these cases are caused by the Coxsackie virus and echovirus (two members of the enterovirus family), herpes and mumps virus can also cause viral meningitis [13-15].
Objectives
The purpose of this study was to establish the seasonality, clinical features, and percentage of aseptic meningitis cases among Jordanian children in Zarqa governorate which may help to decrease the empiric use of antibiotics and the length of hospital stay.
Material and Methods
A Prospective observational study was conducted in Prince Hashim military hospital in Zarqa. Participants of the study were patients, admitted and diagnosed as meningitis during the study period (between 1/12/ 2016 to 30/11/2017).
Sampling
Data were collected by a special questionnaire which was filled by direct interview with the parents and data recorded in the patients file. Cases were divided to three groups according to their age (1 month – 2 years, 2- 5 years and more than 5 years). Patients’ history, complains, laboratorial analysis, vaccinations, and treatment were studied. The clinical criteria for diagnosis of meningitis were clinical picture suggestive of meningitis in addition to the presence of pleocytosis (high WBC number in CSF).
Statistical Methods
Descriptive in addition to some inferential statistics such as t-test, ANOVA, and odds ratio calculation were used to analyze the results.
Results
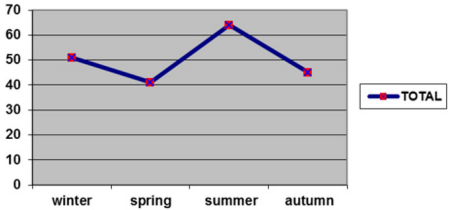
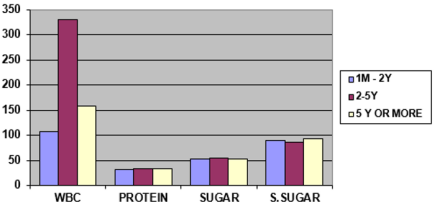
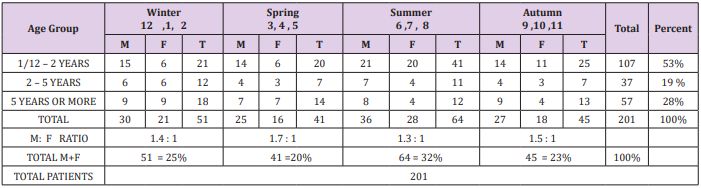
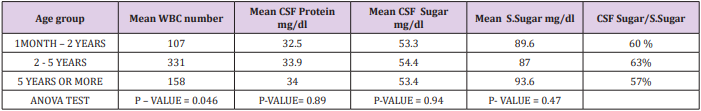
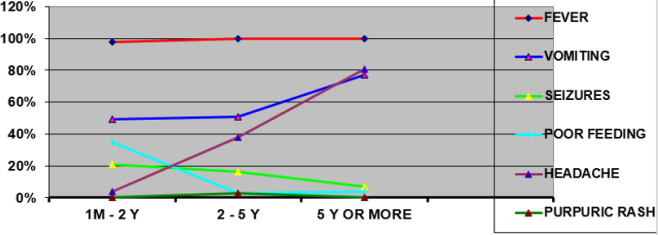
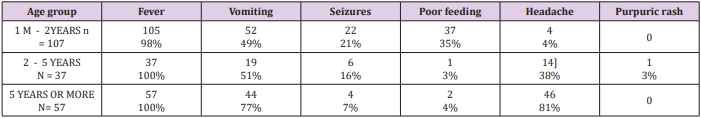
Total of 206 children who were admitted to Prince Hashim Military Hospital with acute meningitis, 53% were under two years old, with male to female ratio (1.4:1). Five were excluded. (Do not fulfill the criteria of the study) Majority of the cases happened in summer and autumn 55%, the least were in spring 20% as shown in Table 1 (Figure 1). Mean number of WBC in CSF was significantly different in the three age groups; the highest was in (2-5 years ) group of age, then the age group of (5 or more) then the age group of ( 1 m - 2 ) years respectively as shown in Table 2 (Figure 2).
No significant difference in means of CSF protein, sugar and serum sugar among the three age groups.
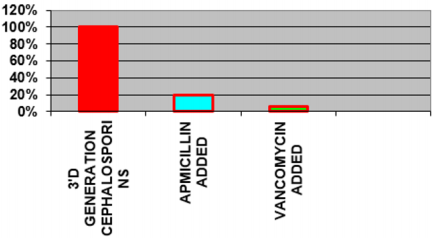
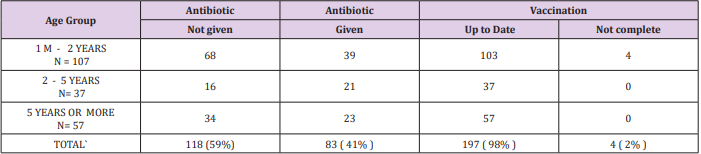
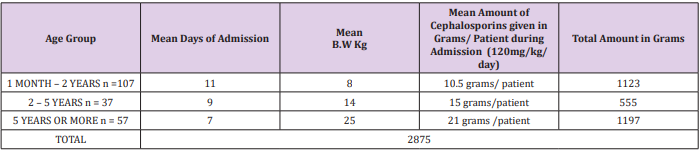
One of these cases had a positive CSF culture (strept.pneumonia). Fever and vomiting were a universal presenting complaint in the three age groups. Convulsions mainly decrease with increasing of age but headache is an increasing complaint by age, Table 3 (Figure 3). Before the admissions 41 % of patients were given antibiotics (oral or parenteral), and during the hospitalization all patients were treated with third generation cephalosporin, and (98%) of these patient were vaccinated up to date (Table 4). Cephalosporin were given to all patients, Vancomycin were given to 6% of patient, but Ampicillin was given to 20% of patients mainly in early infancy (Figure 4).
Discussion
In this study from Zarqa governorate 201 cases of pediatric meningitis were identified over a one-year period. Although not population-based, we are confident that our study captured all inpatient cases in Prince Hashim military hospital in Zarqa, which account for the majority of cases of pediatric meningitis in zarqa governorate. Fever was a universal presenting complaint in the three age groups, vomiting was frequent in the three age groups also, convulsions were mainly decreased with increasing of age, and headache was an increasing complaint in regards of age. 41% of all patients were given antibiotics (oral or parenteral) prior to admission during the present illness. This may explain partially why most of (CSF) cultures were negative. One Patient 5 years old male of the 201 cases has had a positive CSF culture of strept. Pneumonia.
The Practice Guideline Committee in USA does not recommend routine use of latex agglutination for the rapid determination of the bacterial etiology of meningitis, although some would recommend it for patients with a negative CSF Gram stain results [16]. In this study the CSF LATEX wasn’t used. CSF gram stain and differential count for the WBCs in CSF were not available in our hospital lab, during the study period (and are still not available).
Most cases were below 2 years of age (53 %) and occurred during summer and autumn (55%), which goes with the international studies of patients with viral meningitis. All patients (100%) in the current study received antibiotics and were treated as bacterial meningitis inside hospital, although most patients were suspected to have viral meningitis by the clinical picture and CSF findings ,but viral study, gram stain and differential count of WBC in CSF are not available in our hospital. In this study it couldn’t take the risk to treat patients as viral meningitis, depending only on routine CSF analysis and culture.
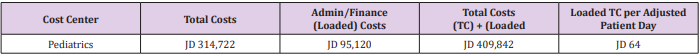
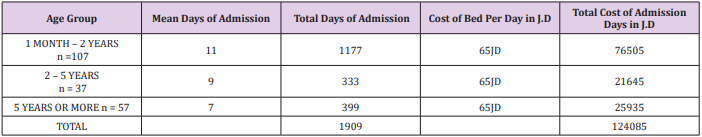
As shown in Tables 5-7 the total cost and economic burden of admissions of patients with meningitis in the hospital is more than 124000 JD per year. (According to prices in year 2016), which could be prevented by using developed diagnostic procedures.
Conclusion
In respect to CSF analysis, culture, age and seasonal distribution, most patients in our study were suspected to have viral meningitis, but they all were treated as bacterial meningitis because of lack of additional lab. investigations such as CSF latex, viral study, WBCs, differential count and gram stain in CSF to confirm viral infection. The use of expensive antibiotics such as 3rd generation cephalosporin in all patients with meningitis including viral cases, in addition to the long stay in hospital (On average 9 days per patient) constitutes heavy economic burden. This economic burden can be greatly reduced if we have proper diagnostic procedures to diagnose viral meningitis, which decreases the days of admission per patient and eliminates the irrational use of antibiotics.
More BJSTR Articles : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.