Intraluminal Pressure Difference of Bakri Balloon in the positive Tamponade test During the Management of severe Post-Partum Hemorrhage
Introduction
Bakri balloon tamponade has been widely used in the management of postpartum hemorrhage recently, with the efficacy is 70%-90% [1]. The proposed mechanism is by creating an intrauterine pressure, including uterine shape changes, secondary uterine activity, balloon–endometrial interactions and distal effects on the flow within the uterine arteries [2,3]. A ‘tamponade test’ is used to determine the clinical effectiveness [3]. There are a few papers involved the measurement of luminal pressure of a variety of balloons in vitro or in vivo. C Georgiou[2] detected pressure generated by the Bakri balloons in two postpartum hemorrhage patients, he got the conclusion that intraluminal pressure within tamponade balloon did not exceed the systolic blood pressure of the patient when a positive tamponade test was established. In our article, we detected and monitored the intrauterine intraluminal pressure (ILPs) within a Bakri balloon every two hours after achieving a positive tamponade test in 30 postpartum hemorrhage patients , recorded the patients’ blood pressure and the amount of blood loss, measured and compared the difference of the ILPs in vivo and in vitro, the aim was to find the optimal inflation liquid volume of filling the Bakri balloon to establish a positive tamponade test, and to explain the working rationale of Bakri balloon about intraluminal pressure.
Materials and Methods
Setting: The obstetric department in the Center of Children and
Women (7,000 births) in Da Lian city, Liao Ning province, China.
Sample: 30 women who required a Bakri balloon and (or) other invasive surgical techniques to control postpartum hemorrhage.
The ethics committee approval in the hospital was required.
To exclude the complex processing of sentence reading, the current study specifically compared Chinese and Japanese word processing in bilinguals while they decided whether two pairs of Chinese characters or Japanese kanjis were similar in meaning or not. Our purpose is to identify the networks involved in semantic processing of Chinese characters and Japanese kanjis, to test if words of both the languages use the same network without involving phonological processing. Furthermore, we want to quantify the differences of semantic processing in the two languages if there are any. This would indicate whether the two groups of bilinguals use the same strategy for semantic processing of logographic characters.
in vitro ILPs in the Bakri Balloon
The ILPs were recorded for the Bakri balloon in the laboratory setting. These readings were obtained using a pressure a Digi Mano (Netech Corp oration, Farmingdale, NY, USA) recorder, which was used widely in clinic medicine. The ILPs were recorded after 50- ml aliquots of normal saline had been used to insufflate the Bakri balloon until a final volume of 600 ml was reached. Five separate series (0–600 ml in 50-ml aliquots) were recorded from five different Bakri balloons.
ILPs in the Bakri Balloon after Positive Tamponade Test Established
From January 2016 to January 2018, patients with massive PPH (blood loss≥1500ml) who needed intrauterine Bakri balloon insertion with (without) other hemostasis techniques were included. After the positive tamponade test established, the ILPs within the Bakri balloon were detected every two hours until the balloon was removed. The cause of the PPH, the sequence of treatments, estimated total blood loss and clinical outcomes were recorded. The procedure for insertion of the Bakri balloon was similar to that described by the inventor [4], vaginal packing was performed when there was evidence of slippage or prolapse of the balloon through the cervix [4]. The distal end of the catheter was tapped to the patient’s thigh, but weights were not used. Ultrasound visualization of balloon placement was necessary in our series [5]. When the balloon was inserted during a caesarean section, the distal end of the balloon shaft was passed through the cervical opening with an assistant pulling the end per vagina. If bleeding was arrested after balloon inflation, the balloon tamponade was continued for 24 hours, after which, the deflation was performed. All patients had an indwelling Foley catheter to monitor urine output, received continuous syntocine for 24 hours until the Bakri balloon was deflated. Broad spectrum antibiotics were used for prophylaxis.
Statistical Procedures
The statistical analysis was performed using SPSS software(version 16; SPSS Inc, Chicago, IL).Continuous data were presented using means and standard deviation (SDs)
Results
in vitro ILPs in the Bakri balloon
The readings demonstrated that in absence of any external restrictions, ILPs increased slowly by the increase of the amount of filled saline liquid, reached to the peak of 60-70mmHg at 600 ml insufflation. There is no fluctations in ILP when the balloon was allowed to stand for 2 hours. when an external compressive force was applied, such as squeezing the balloon by hand, the ILP increased as expected. The numerical relationship between this volume and the resulting ILP is linear, the linear regression model is y=31.033+0.768x, y : intraluminal pressure, x: liquid volume.
Bakri Intrauterine Balloon Tamponade in the Management of Severe Postpartum Hemorrhage Patients
There were 14,886 deliveries in our department during the period. The frequency of primary PPH with an estimated blood loss exceeding 500 ml was 3.6% (n=535). The frequency of massive PPH with an estimated blood loss exceeding 1.5 L was 0.55% (n=82). Among the 82 patients with massive PPH, 30 cases were used with Bakri balloon catheter. During the same period, there were 5 peripartum hysterectomies, 2 involved attempt ed use of the Bakri balloon catheter and were not included in this case series. All the identified cases of PPH that involved use of the Bakri balloon catheter failed initial medical management with oxytoxics, including bolus syntometrine, syntocinon bolus and infusion, and intra muscular carboprost injections. In 18 cases, the Bakri balloon was the only modality of treatment after medical management; in the remaining 12 patients, it was used combined with uterine compression sutures or pelvic artery ligature or pelvic artery embolization. All patients were transferred to a High Dependency Unit, some required transfusion with blood cells or fresh frozen plasma. There were no major complications arising from the use of the Bakri balloon catheter.
ILPs of Bakri Balloon in the PPH Patients
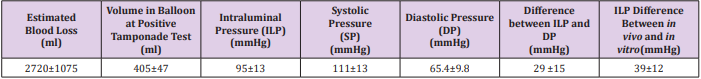
Following the establishment of a positive tamponade test, the saline liquid volume in balloon was 405±47ml, Intraluminal pressure (ILP) in Bakri balloon was 95±13mmHg, which is higher than in vitro, the difference is 39±12mmHg. ILPs in Bakri balloon did not show obvious fluctuation during the patient bed rest but increased when extra forces applied to the patient’s abdomen, such as cough, uterine massage. Patients’ average systolic pressure were 111±13 mmHg, diastolic pressure was 65.4±9.8 mmHg, which revealed that the actual ILPs in Bakri did not exceed the patient’s systolic blood pressure but did exceed the patient’s diastolic blood pressure (Table 1).
Discussion
Uterine tamponade balloons are emerging as a fertility sparing and lifesaving option in the management of PPH [6]. In 1992, Bakri introduced intrauterine balloon tamponade for the treatment of obstetric hemorrhage during cesarean delivery [7]. Recent literature has shown an overall success rate of 75% to 94% at avoiding embolization or hysterectomy. The principle of balloon tamponade therapy is to fill the uterine cavity to control bleeding with pressure [8]. This is achieved as a result of uniform pressure over the open sinuses of the uterus, the pressure on the blood vessel is greater than the pressure within the vessel. If pressure is applied for long enough, the blood will clot and form a permanent seal [9]. In non-uterine systems in which bleeding is successfully counteracted by balloon tamponade, relative ely low ILPs are used. For example, only 25-30 mmHg is required when using the Sengstaken–Blakemore tube in the oesophagus [10].In the bladder, a pressure equal to the diastolic arterial pressure’, approximately 75–80 mmHg, is required [11]. However, there does not appear to be any published experimental recordings of postpartum uterine pressures or data on the actual pressures required to stop bleeding from a postpartum hemorrhage uterus.
Our study sought to detect the intraluminal pressure to establish positive tamponade test in vivo, assess the mechanism to explain the attainment of a positive tamponade test . We found that Bakri balloon could exert a positive tamponade test at 405±47 ml filling volumes, which was recommended by the manufacturers and other scholars. As noted previously, the intraluminal pressure can be impacted by external forces, such as fundal contractility. We found a linear regression relationship between the intraluminal pressure and the balloon volume in vitro, the linear model is y=31.033+0.768x , (y : intraluminal pressure , x: liquid volume). Our results were similar to Kathleen M [12] and Georgiou [2]. Georgiou had published a series of intraluminal pressure readings during the establishment of uterine tamponade using the Bakri balloon, he found a curvilinear relationship between the intraluminal pressure and the balloon volume in vitro and higher pressures in vivo, but with the limitations based on only two cases in vivo [2]. We obtained 30 cases, including 12 cases combined with other surgical hemostasis techniques, these cases could provide reproducibility of the results, were able to demonstrate uterine activity simultaneously independently from ILP recordings.
We found that when positive tamponade test established, ILPs increased in vivo and was higher than in vitro, the average difference is 39±12 mmHg. which was almost equal to uerine spiral artery vasculature pressure [13]. We also found the actual ILPs did not exceed the patient’s systolic blood pressure but did exceed the patient’s diastolic blood pressure to achieve a positive tamponade test, which was in accordance with C Georgiou’s conclusion [2]. The relationship between ILP, intraluminal volume, systolic/ diastolic blood pressures and bleeding cessation were inconsistent. We speculated that uterine wall compliance with the intrauterine balloon which inflated by some volume liquid, the good fitness of the balloon- uterine interface, stimulate uterine muscle fibers that form a figure of eight , result in uterine contraction and placenta bed vasculature hemostasis after delivery. Thus, the clinical endpoint of a positive tamponade test may be a function of the pressure exerted by uterine contraction combined with the ball boon liquid luminal pressure, which could explain the difference between the ILPs in vivo and in vitro.
So, we proposed that to establish a positive tampona de test, some prerequisites should exist. The first prerequisite is that the uterine is enlarged and atonic, which could not able to counteract an increase in uterine cavity volume and could not expel the inserted balloon. We once had a postpartum hemorrhage patient, with part of placenta retention, vaginal bleeding with the uterine in good contraction, Bakri balloon was tried three times but expelled from the uterus immediately, at last, uterine artery embolization worked. The second prerequisite is that a good fitness of balloon-uterine interface, the balloon should be in some kind of material, with some tension, elastic, so that the effect of contact by the balloon at the uterine surface could elicit uterine secondary contration. The third prerequisite is the ILPs should be higher in vivo than in vitro at the corresponding liquid volume, the increased value is worked out by the uterus secondary contraction force combined with the inside balloon and is almost equal to the uterine spiral artery vasulature pressure ,30-40mmHg. During pregnancy, the spiral artery in the endometrium and myometrial segments is the main blood supply to the uteroplacenta, the vasculature pressure is 20-40mmHg [13]. We proposed the value of increased ILPs could be used to help to determine whether the positive tamponade test set up.
Conclusion
After a positive tamponade test was established, the intralum inal pressure within the tamponade balloon increased in vivo than in vitro, the difference value was roughly equal to the uterine spiral artery vasculat ure pressure.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.