Diagnosis of Clinical Narrow Pelvis by Intranatal Ultrasound
Introduction
By definition of Kalganova R.I. a clinical narrow pelvis should include all cases of disproportion between fetal head and woman pelvis, regardless of its size. It is recommended to include in this group of obstetric pathology not only childbirths that ended operatively, but also spontaneous births, during which, especially the biomechanism, insertion and configuration of fetal head, indicate the presence of fetal-pelvic disproportion [1]. High rates of birth injury as a result of pelvic fetal-pelvic disproportion determine the relevance of this study
Materials and Methods
On the basis of maternity hospitals of Trans-Baikal Region in the years 2018-2019 was held retrospective and prospective analysis of 60 labor histories, which were divided into 3 equal groups: group 1 - pregnant women with normal sizes of the large pelvis, group 2 - pregnant women with macrosomia, group 3 - pregnant women with a reduced size of the large pelvis. The groups are comparable in age, extragenital pathology and parity of labor. Intranatal ultrasound was performed by a portable highend ultrasound scanning device MySono U6 Samsung Medison. The study was conducted by a convex sensor with two approaches: transabdominal and transvaginal. The presence of clinical narrow pelvis was evaluated based on assessment of angle labor’s progression (°), degree of head’s configuration in area of swept seam (mm), cross-sectional area of segment of head’s insertion (cm2 ) and ultrasound modification of Vasten symptom. Translabial access was used to determine angle of labor progression, degree of head configuration, and cross-sectional area of head insertion segment; transabdominal access was used to determine ultrasound modified Vasten symptom.
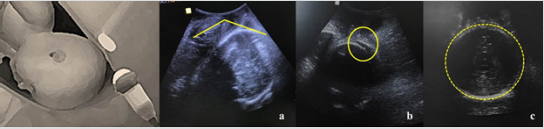
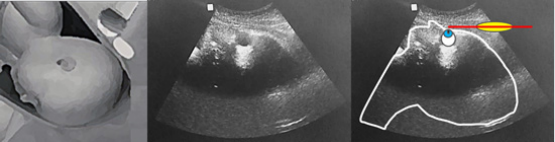
Angle of labor progression was defined as the angle between maximum longitudinal size of t pubic symphysis and the line tangent to the most distant part of the fetal head [2]. Degree of head configuration was defined as the distance corresponding to passage of the parietal bones on each other. To determine cross-sectional area of head insertion segment, the ultrasound sensor was placed between the labia majora in the sagittal position, after which the sensor was rotated 90° into the frontal plane corresponding to the line between the mounds of the ischial bones (Figure 1). Ultrasound modified Vasten symptom was defined as ratio between line of maximum longitudinal size of pubic symphysis and parallel line consisting of a number of points of fetal head presenting (Figure 2). Statistical processing of research results was carried out using IBM SPSS Statistics Version 25.0.
a. angle of labor progression,
b. degree of fetal head configuration
c. cross-sectional area of head insertion segment
Figure 1: Measurement technique by intranatal ultrasound
Results
In group 1, childbirth occurred on a period of 39 weeks ± 3 days, in group 2 - 38 weeks ± 4 days, in group 3 - 40 weeks ± 2 days. The average mass of fetuses at birth in group 1 was 3416 ± 315 g, in group 2 - 2976 ± 289 g (p < 0.05), in group 3 - 4263 ± 238 g (p <0.05). In group 1, 90% of births occurred through the natural birth canal (p<0.05). In 10% there was a deterioration of fetus during the active phase of labor, which, along with discoordination of labor, served as an indication for cesarean section. In group 2, delivery through the natural genital tract occurred in 60%, in group 3 - in 50% of cases (p > 0.05). Angle of labor progression below 120° with full disclosure of uterine throat was observed in patients with subsequent operative delivery in group 2 in 75% (6), in group 3 in 100% (10) of cases (p < 0.05). A reliable relationship between cross-sectional area of head insertion segment and labor outcome was not found, however, this criterion allows us to estimate the progress of labor (by analyzing dynamics of increase in cross-sectional area of head insertion segment). In 30% of 2 group cases and 10% of 3 group cases newborns were diagnosed with cephalohematoma. This complication was associated with the degree of head configuration along arrow-shaped seam equal to 16 mm or more, which indicates the absence of a diagnosis of relative clinical narrow pelvis in these cases (p < 0.05). Ultrasound modified Vasten symptom was positive in 100% of 2 and 3 group’s women, which labors finished by cesarean section due to the clinical narrow pelvis (p < 0.05). In patients whose newborns had cephalohematomas, Vasten’s “uniform” symptom was diagnosed by ultrasound in all cases (p < 0.05).
Discussion
Angle of labor progression, degree of fetal head configuration and ultrasound modified Vasten symptom allow diagnosis of clinical narrow pelvis in pregnant women at high risk in intranatal period, which will optimize delivery tactics and prevent obstetric and perinatal complications.
Acknowledgement
There are no Acknowledgements of the authors. There is no conflict of interest. The source of funding is the personal funds of the authors.
More BJSTR Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.