Epidemiological Characteristics of Women Participating in Breast Cancer Screening by Bach Mai Hospital
Introduction
Breast cancer is the most common cancer in women worldwide. It is also the leading cause of death among women globally. According to GLOBOCAN 2012, in Vietnam, breast cancer - the most common cancer in women - is ranked as the third cause of cancer death, after liver and lung cancer. Moreover, breast cancer is more common in female over the age of 40. Furthermore, 6-19% of breast cancer cases have a genetic nature. Several genes, for example BRCA1, BRAC2, PTEN, and PT53, are found to be related to breast cancer. In addition, other non-genetic components, such as age, gender, reproductive history, menopause, menstruation, hormone replacement therapy, obesity, smoking, benign breast disease, might also contribute as the risk factors of breast cancer [1-2]. Breast cancer is a curable disease with early diagnosis and a positive treatment strategy. Therefore, screening for early breast cancer is important to increase the curable rate which improves the quality of life for patients as well as reduces the mortality rate. In Vietnam, The Nuclear Medicine and Oncology Center participated in 04 breast cancer screening programs for over 30-year-old Vietnamese women, in which there are 03 programs hosted by Ministry of Health and Bright Future Foundation and 01 program coordinated with Ha Tinh General Hospital. Based on the results of these programs, we conduct a study with these following aims:
a) Describe the epidemiological characteristics of women participating in the breast cancer screening program at Bach Mai Hospitaland
b) Evaluate the results of screening programs for breast cancer screening.
Patients and Methods
Study Population
A descriptive cross-sectional study was conducted among 4250 women at the age of 30 years and older who participated in the breast cancer screening from 2015 to 2017 at The Nuclear Medicine and Oncology Center – Bach Mai Hospital.
Data Collection
A structured questionnaire consisted of two parts: Demographic information and the outcome of breast cancer examination. The collected demographic information included Age, Hometown, Educational level, Occupation, Marital status, history of cancer.
The outcome of breast cancer examination was assessed by using the following criteria:
a) Clinical assessment
b) Ultrasound image
c) Mammography results (if necessary)
Data Analysis
Data were analyzed using Statistical Package for Social Science Version 16.0 software, SPSS. Data were summarized using number and percentage for qualitative variables. Chi-square and Fisher’s Exact test were used to examine the related factors of breast abnormalities, re-screening, and breast self-examination status. A p-value less than or equal to 0.05 was considered statistically significant.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Our study was approved by Science and Ethics Council of Bach Mai hospital. A verbal consent was obtained from all participants before filling the questionnaire.
Results
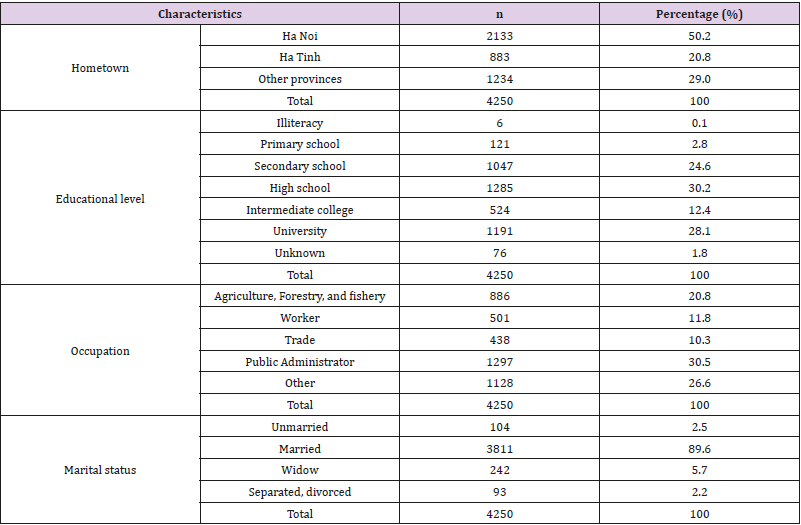
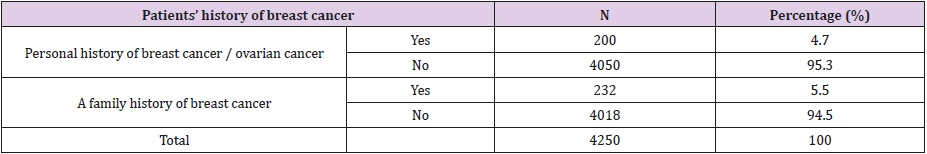
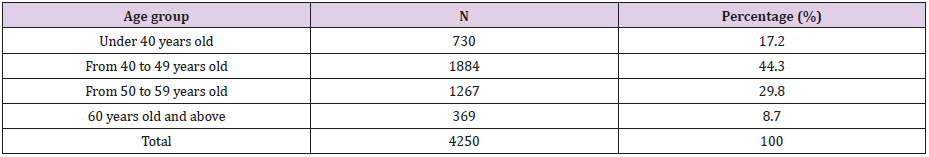
Out of 4,250 women participating in screening, the majority came from Hanoi (accounting for 50.2%). In addition, most of the subjects had an educational level of high school or higher (70.7%), working mostly as public administrators (30.5%) and currently married (89. 6%) (Table 1). Women who had a history of breast cancer and a family history of breast cancer only accounted for 4.7% and 5.5% of all women in the screening (Table 2). The study results showed that most women in the screening were from the age of 40 to 49 with 1884 women, accounting for 44.3%, followed by the age of 50 to 59, with 1267 women, accounting for 29.8 %. The lowest group was the 60 years old and above group, with 369 women participating in the screening, accounting for 8.7%.
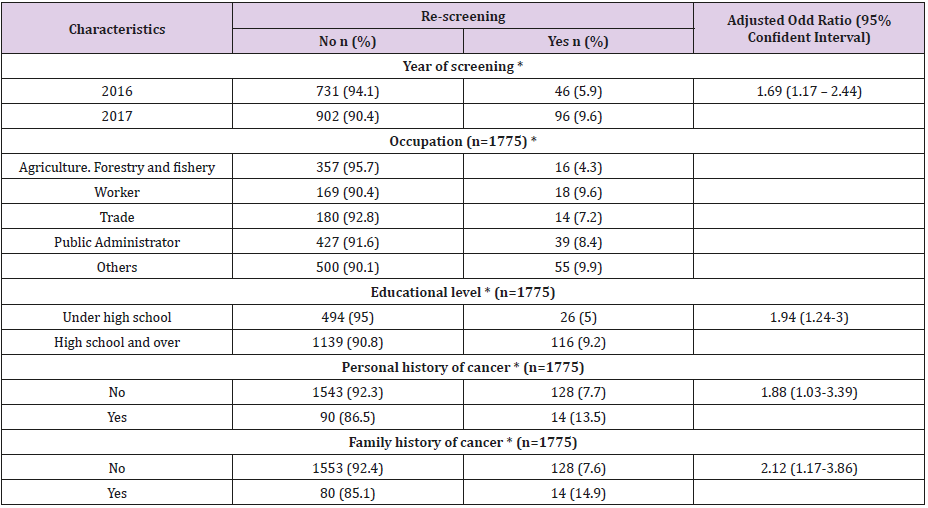
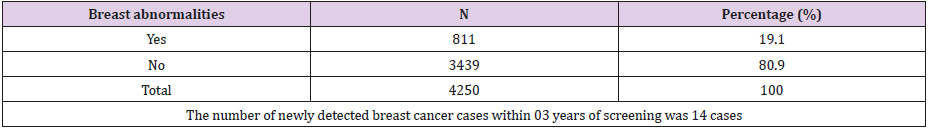
In 2016 and 2017, 1775 women were interviewed about their previous screening experience. The number of women re-screened in 2016 and 2017 was still limited, with 142 people, accounting for 8% of all women screened in 2016 and 2017 (Table 3). After the screening in 2015, the proportion of women re-screening in 2017 was 1.69 times higher than in 2016 (p <0.05). In addition, the results of the study also showed that there was a statistically significant difference in the rate of re-screening between different occupations, educational background, and history of cancer. The screening rate for women with a high school diploma or higher was 1.94 times higher than for those with lower education. Women having a personal or a family history of cancer were recorded with a higher re-screening rate of 1.88 and 2.12 times than those without a history of cancer (Table 4). After 3 years of screening among 4250 women, the results showed that 811 women were diagnosed with breast abnormalities, accounting for 19.1%.
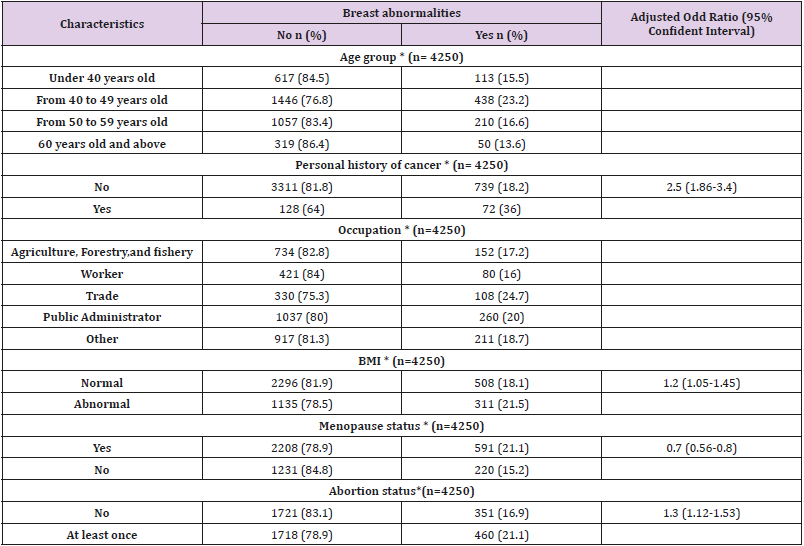
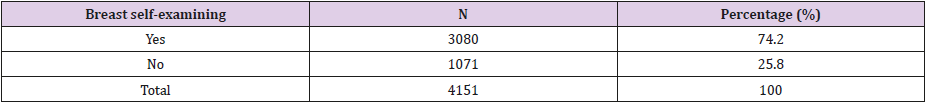
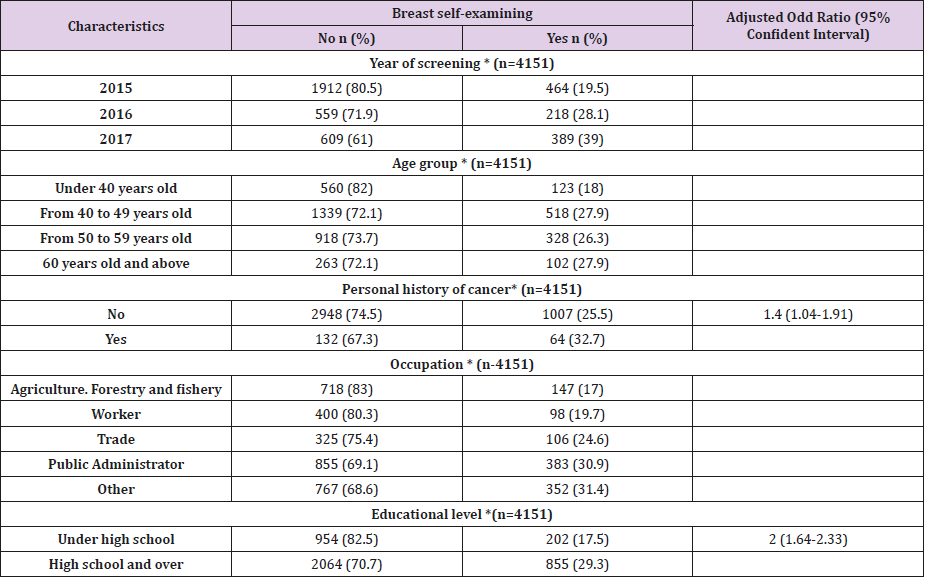
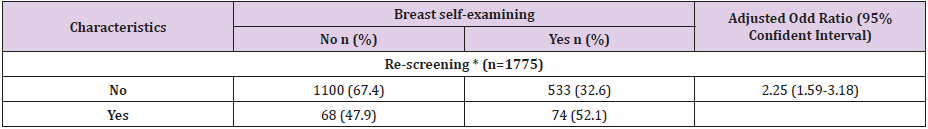
In 2015, 2016 and 2017, the newly detected breast cancer cases were 6 cases, 5 cases, and 3 cases, respectively (Table 5). The incidence of breast abnormalities was statistically significant among age, family history of cancer, occupation, BMI, menopause and abortion status (Table 6). Among 4250 women screened, only 4151 women agreed to answer questions regarding monthly breast self-examination. Only 25.8% of answered women performed monthly breast self-examination (Table 7). The results of the above table showed that the percentage of women performing breast selfexamination increased over the years, age groups and occupations. This difference was statistically significant with p-value<0.05 (Table 8). The results of the above table indicated that the rate of breast self-examination in the re-screening group was nearly 20% higher than that of the first-time screening group. This difference was statistically significant with thep-value<0.05 (Table 9).
Table 6: The relationship between breast abnormalities detection rate and related factors.
* p<0.05, Chi-square test
Table 8: The relationship between breast self-examining rate and related factors.
* p<0.05, Chi-square test
Table 9: The relationship between breast self-examining rate and re-screening rate.
* p<0.05, Chi-square test
Discussion
Breast cancer screening is one of the Vietnam Ministry of Health’s strategies for cancer prevention. Breast cancer screening by clinical examination, breast ultrasound, mammograms make a huge contribution in early diagnosis and effective treatment of breast cancer. In three years from 2015 to 2017, the Nuclear Medicine and Oncology Center has participated in three breast cancer screening programs of the Ministry of Health in collaboration with the Bright Future Foundation and one breast cancer screening program in collaboration with Ha Tinh general hospital. Among 4250 women participating in screening, the majority came from Hanoi (accounting for 50.2%). In addition, most of the subjects had high school educational level and higher (70.7%), mostly working as public administrator (30.5%) and currently married (89.6%). This indicates that screening programs have reached to many women at the age of 40 and over, with different educational levels. However, our study also observed that women with higher level of education are more likely to access to screening program than those with lower educational level. In addition, the policy of universalizing education at all levels has reduced the number of the illiterate and women who had primary and secondary education, which might contribute to affect also contributed to the interpretation of this study results.
Studies showed that 6 to 19% of breast cancer patients were related to family history [3]. In these cases, the disease usually starts at a young age, which high incidence of breast cancer occurs from both sides of the family, with many members suffering from cancer. Based on the incidence of breast cancer in the UK, the probability of breast cancer among person without a family history of cancer was 7.8%while this rate among person having one and two family members with breast cancer were 13.3% and 21.1%, respectively [4]. Currently, genes involved in familial breast cancer, ovarian cancer have been identified as BRCA1, BRCA2, PTEN, TP53; CDH1 [2, 5]. These studies indicate that we also need to focus on communication and encourage women with a family history of breast cancer to seek breast cancer screening and regular examinations every year. However, our study has not found any relation between the family history of breast cancer and breast abnormalities. This may due to the number of women with a personal history of breast cancer and a family history of breast cancer was quite low, accounting for only 4.7% and 5.5%, respectively.
In addition to genetic causes, several other factors are associated with the development of breast cancer such as age, sex, reproductive history, menstruation, menopause, and benign breast disease. Breast cancer is common in the age group of 50-69 [5]. In our study, the age group which was most likely to participate in the screening was 40-49 with 1884 women, accounting for 44.3%, followed by the age group of 50-59, accounting for 29.8% with 1267 participants. The lowest group was an over60yearsold group, with 369 women taking the screening, accounting for 8.7%. Although the program prioritized screening for women who past the age of 40, 17.2% of women under 40 were observed within the screening process. These women were most likely to experience pain in the breast or to feel their own breast lesions, or to have their ultrasound results with cysts, fibrosis, and fibroids in the breast. When they knew about this program, they actively registered for medical examination.
The Ministry of Health’s breast cancer screening program, in collaboration with the Bright Future Foundation, expects women at high risk for breast cancer to have a medical examination every year (as a form of periodic breast cancer screening). After the screening in 2015, the number of women re-screened in 2016 and 2017 was still limited, with 142 people, accounting for 8% of all women in 2016 and 2017. It may be due to the limited knowledge of the women or lack of awareness about breast cancer after the normal results of the previous examination. Another possible reason is that they were unable to register for the screening. In fact, when implementing this screening program, the number of people who wish to apply for free examination is quite high. Many women registered online as well as offline at the Nuclear and Oncology Medical Center – Bach Mai hospital. However, the number of free screening ticket is limited, so many people cannot participate in the program. Therefore, it is urgent to expand the screening program in both time and number of free tickets. In order to do so, actions should be taken to call for more funding from government, donors and social organization.
After the screening of 2015 and 2016, the rate of women reparticipating in breast cancer screening in 2017 was 1.69 times higher than in 2016 (p <0.05) (Table 4). In addition, the study results also showed that there was a significant difference between the follow-up rate in different occupations, education levels and history of cancer (p< 0.05). The rate of re-screening among women with the educational level of high school and above was 1.94 times higher than that of women with lower educational levels (Table 4). Women with a history of cancer or had a family member with cancer had a 1.88- and 2.12-times higher re-screening rate than women without these factors, respectively. This suggested that women who had higher risk of breast cancer were more likely to do regular follow-up examination than women with lower risk of developing breast cancer.
Over 3 years of screening on 4250 women, screening results showed that 811 women were found with abnormalities in the breast, such as cystic lesions, fibroids, and fibrosis, and abces, accounting for 19.1%. Particularly, in 2015, 2016 and 2017, 6 cases, 5 cases and 3 cases of breast cancer were detected respectively. All these cases were early-stage breast cancer and now have been at the stage of stable disease after treatment. This is one of the important goals of the program, which is to early detect disease, and to increase awareness of women in screening for early detection of cancer in general and breast cancer. Patient with a history of breast cancer, ovarian cancer, and peritoneal cancer had a higher risk of breast cancer [1]. Body mass index (BMI) is an independent risk factor for breast cancer, especially in white women. Some studies have shown an association between high BMI and increased risk of postmenopausal breast cancer. This increased risk was due to an increase in the concentration of endogenous estrogens produced from adipose tissue [1, 6].
The screening results showed a statistically significant difference in breast abnormality rate between different groups in the age group, history of self-cancer, occupation, BMI, menopause and abortion status. Our research also showed that women with personal history of cancer were 2.5 times more likely to have breast abnormalities, compared to one without this history. Furthermore, women with abnormal BMI (malnutrition or obesity) were found to be 1.2 times more likely to develop breast abnormalities than women with normal BMI. In addition, women who underwent abortion had a 1.3 times higher risk of developing abnormalities than women who did not. Finally, menopause was also a factor protecting women from the risk of breast abnormalities (Table 6). The proportion of women who had self-examination of breast gradually increased each year. Thus, this proportion is also differencing between different age groups and occupations. These differences were statistically significant with p <0.05. In addition, women with a history of cancer and high levels of education were 1.4 and 2 times more likely to perform routine breast self-examination than those without a history of cancer and lower education level (p <0.05), respectively.
The rate of breast self-examination in the re-screening group was nearly 20% higher than the group for the first-time screening. This difference was statistically significant with p <0.05 (Table 9). Thanks to the screening program with the activities of examination and consulting, women were aware of self-examination and breast screen regularly. This is also one of the objectives of the Ministry of Health’s screening for early detection of breast cancer in coordination with the Bright Future Foundation. This success implies the need of expanding the screening program and making it more public accessible through the help of Government and the Foundation.
Conclusion
In the total of 4250 women participating in the screening, 70.7% had the educational level of high school and higher. 25.8% of them were aware of breast self-examination.4.7% of women had a history of breast cancer while 5.5% of women had a family history of breast cancer. 65.1% of women participating in screening were between the ages of 40-59. The percentage of re-screening was 8%. Women with a high level of education or history of cancer often have a higher awareness of breast cancer screening than those without it. The screening program has recorded 19.1% of women with breast abnormalities, of which the number of newly discovered breast cancer cases were 6, 5, and 3 in 2015, 2016 and 2017, respectively. The incidence of abnormalities was found with statistically significant differences among groups of age, family history of cancer, occupation, BMI, menopause, and abortion. Even though, the screening results after 03 years has quite limited it still makes a great contribution in changing women awareness of breast cancer. Through 03 years of implementing the breast cancer screening program, our study has observed the increasing in the awareness of breast self-examination and breast cancer rescreening among women, especially those with higher risk. Women who had higher risk of breast cancer were more likely to do regular follow-up examination than women with lower risk of developing breast cancer. In addition, after participating in the breast cancer screen, women were more aware of breast self - examination and breast cancer screening. Therefore, expanding the screening program and making it more public accessible is necessary works that need to be carried out in the future.
For more Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.